Magnetic resonance (MR) imaging is gaining increased acceptance in the emergency setting despite the continued dominance of computed tomography. MR has the advantages of more precise tissue characterization, superior soft tissue contrast, and a lack of ionizing radiation. Traditional barriers to emergent MR are being overcome by streamlined imaging protocols and newer rapid-acquisition sequences. As the utilization of MR imaging in the emergency department increases, a strong working knowledge of the MR appearance of the most commonly encountered abdominopelvic pathologies is essential. In this article, MR imaging protocols and findings of acute pelvic, scrotal, and gastrointestinal pathologies are discussed.
Key points
- •
Magnetic resonance (MR) imaging of the abdomen and pelvis is playing an increasing role in the emergency setting, both in primary diagnosis and as a problem-solving modality.
- •
MR imaging is especially useful in patients in whom exposure to ionizing radiation is a concern, including patients who are pregnant, children, and patients with chronic diseases that necessitate multiple scans, such as Crohn disease.
- •
MR sequences should be tailored to the patient’s specific clinical presentation with the aim of minimizing scan time while maximizing diagnostic accuracy.
Introduction
Magnetic resonance (MR) imaging is an established imaging method for the evaluation of many abdominal and pelvic diseases. The ability to distinguish different types of soft tissues based on their intrinsic signal intensity, multiplanar capability, and the identification of pathology without exposing patients to radiation are the major advantages of MR imaging. Although imaging of the gastrointestinal (GI) tract can be a challenge for MR imaging because of peristalsis, fast MR techniques allow accurate depiction of many acute GI conditions. MR imaging can provide clear, valuable information for clinical management in patients with acute pelvic pain, acute scrotum, and suspected appendicitis. In addition to these conditions, acute pancreaticobiliary diseases, such as acute cholecystitis, cholelithiasis, choledocholithiasis, cholangitis, and pancreatitis also can be depicted with MR imaging and MR cholangiopancreatography (MRCP), which are discussed in the article (See Bates DDB, LeBedis CA, Soto J, et al: Use of MR in Pancreaticobiliary Emergencies , in this issue). In this article, the authors discuss MR imaging protocols and findings of acute pelvic, scrotal, and GI pathologies.
Introduction
Magnetic resonance (MR) imaging is an established imaging method for the evaluation of many abdominal and pelvic diseases. The ability to distinguish different types of soft tissues based on their intrinsic signal intensity, multiplanar capability, and the identification of pathology without exposing patients to radiation are the major advantages of MR imaging. Although imaging of the gastrointestinal (GI) tract can be a challenge for MR imaging because of peristalsis, fast MR techniques allow accurate depiction of many acute GI conditions. MR imaging can provide clear, valuable information for clinical management in patients with acute pelvic pain, acute scrotum, and suspected appendicitis. In addition to these conditions, acute pancreaticobiliary diseases, such as acute cholecystitis, cholelithiasis, choledocholithiasis, cholangitis, and pancreatitis also can be depicted with MR imaging and MR cholangiopancreatography (MRCP), which are discussed in the article (See Bates DDB, LeBedis CA, Soto J, et al: Use of MR in Pancreaticobiliary Emergencies , in this issue). In this article, the authors discuss MR imaging protocols and findings of acute pelvic, scrotal, and GI pathologies.
Normal anatomy and imaging techniques
Female pelvic structures (uterus, cervix, vagina, ovary, and adnexa) are readily demonstrated on MR imaging. T2-weighted imaging is the mainstay sequence for differentiation of zonal anatomy of the uterus. Three distinct zones ( Fig. 1 ) of the premenopausal uterus include an innermost layer of uterine endometrium, middle layer (junctional zone), and outermost layer. The innermost high T2 signal intensity represents the endometrium with varying thickness depending on age and menstrual cycle. Generally, an endometrial thickness of less than 10 mm is considered normal in reproductive-age women, whereas thickness of less than 5 mm is considered normal in postmenopausal women. The middle layer is the junctional zone, which represents the inner myometrium. The junctional zone has low signal intensity relative to the adjacent outermost layer. The outermost layer is the myometrium, which has intermediate signal intensity on T2-weighted images. The uterine cervix also demonstrates zonal anatomy on T2-weighted images: central hyperintense zone of endocervical mucosa, middle hypointense zone of fibromuscular stroma, and outer intermediate signal intensity of loose stroma. This zonal anatomy is indistinct in the postmenopausal uterus, in which the junctional zone may not be visualized. On T1-weighted images, the uterus is isointense to the muscle and zonal anatomy is not appreciated. The normal ovarian stroma has intermediate signal intensity on T1-weighted images. On T2-weighted images, ovarian follicles demonstrate very high signal intensity. The ovarian medulla usually has higher signal intensity than the ovarian cortex. The vagina also demonstrates zonal anatomy on T2-weighted images: central hyperintense signal of mucosa and intraluminal fluid, middle hypointense zone of submucosal and muscularis layer, and outer hyperintense zone of adventitial layer and vascular plexus.
The testicles lie within each hemiscrotum and are suspended by the spermatic cords. They have homogeneously intermediate signal intensity on T1-weighted images and are slightly hyperintense on T2-weighed images. Normal testicles show slow and steady contrast enhancement after gadolinium administration. The surrounding tunica albuginea and the visceral layer of tunica vaginalis are seen as a thin stripe of low signal intensity on both T1-weighted and T2-weighted images due to their fibrous component (see Fig. 1 ). The epididymes are located along the superolateral aspect of the testicle and consist of head, body, and tail. The epididymal tail continues as the vas deferens to the spermatic cord. The epididymis has signal intensity similar to the testicular parenchyma on T1-weighted images and lower signal intensity than that of testicular parenchyma on T2-weighted images.
Distended bowel loops contain T2 hyperintense fluid, which serves as a natural contrast medium. The normal bowel wall is barely visible when the bowel loops are distended. Its thickness is up to 1 to 2 mm for small bowel and 3 mm for the large bowel. The small bowel diameter is usually less than 2.5 cm in diameter. The appendix is a blind-ended tubular structure arising from the cecum with T1 hypointensity and T2 hyperintensity. Its wall thickness is less than 2 mm and the total axial diameter is usually less than 6 mm. Air bubbles within the lumen may be depicted. When fat suppression technique is applied adequately, the periappendiceal tissues appear hypointense.
Imaging protocols
MR imaging in the emergency setting requires the use of streamlined protocols to minimize imaging time while maintaining diagnostic accuracy for the most commonly encountered abdominopelvic pathologies. For the evaluation of lower abdominal and pelvic pain, our protocol begins with multiplanar T2 single-shot fast spin-echo (SSFSE) sequence to identify pathology and establish the best plane for additional imaging. This is followed by axial T2 fast-spin echo and axial short tau inversion recovery (STIR) sequences to highlight pathologies. In patients who are not pregnant, fat-saturated T1-weighted precontrast and postcontrast images are obtained ( Table 1 ). Ideally acquisition will be monitored by the interpreting radiologist to adjust imaging planes and prescribe additional sequences as necessary for problem solving.
| Acute Appendicitis | Acute Appendicitis (Pregnant) | Pancreaticobiliary Pathology |
|---|---|---|
| Axial, coronal, and sagittal T2 SSFSE | Axial, coronal, and sagittal T2 SSFSE | Coronal balanced steady state gradient echo |
| Axial T2 FSE | Axial T2 FSE | Coronal T2 SSFSE |
| Axial STIR | Axial STIR | Axial fat-saturated T2 |
| Axial T1 fat-saturated precontrast and postcontrast | — | Axial 3-point Dixon |
| — | — | Dynamic contrast-enhanced fat-saturated T1 (pre-, 25, 35, 70, 180, and 240 s) |
| — | — | 3D MRCP |
For evaluation of pancreaticobiliary pathology, our protocol includes coronal balanced steady-state gradient echo (FIESTA), coronal T2 SSFSE, axial fat-saturated T2, axial 3-point Dixon, dynamic contrast-enhanced fat-saturated T1 (pre-, 25, 35, 70, 180, and 240 seconds), and 3-dimensional MRCP.
Pelvic emergencies
Degenerating Leiomyoma
Uterine leiomyomas are the most common pelvic tumor in women, with a prevalence of 20% to 30% in women older than 30 years. Abnormal menstrual bleeding, pelvic pain, or pressure-related symptoms can occur depending on number, size, and location of leiomyoma. Pain can occur in up to 30% of patients, and is usually a result of acute degeneration. Large leiomyomas may outgrow their blood supply, leading to ischemia and necrosis. There are many types of degenerating leiomyoma: hyaline, calcific, cystic, myxoid, fatty, and red degeneration. The most common type is hyaline degeneration, which accounts for up to 60% of degenerating leiomyomas.
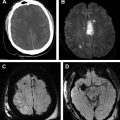
Because of its high soft tissue contrast, MR imaging is an excellent modality for detection of leiomyoma and related complications. Nondegenerating leiomyomata appear well-circumscribed, homogeneously hypointense on T2-weighted images when compared with the outer myometrium. Several types of leiomyoma degeneration can be suggested based on MR appearances with an overall accuracy of 69% ( Fig. 2 ). Hyaline and calcific degenerations show low signal intensity or cobblestone appearance on T2-weighted images. Red degeneration represents hemorrhagic infarction secondary to obstructing venous return. It appears as T1 hyperintensity on the periphery of the leiomyoma or diffusely throughout the entire leiomyoma, and variable signal intensity on T2-weighed images. Sometimes, low T2 signal intensity rim can be seen. Myoma with myxoid degeneration will appear very hyperintense on T2-weighted images and enhances after gadolinium administration. Cystic degeneration also demonstrates high T2 signal intensity, but the cystic components do not enhance following gadolinium administration. MR imaging has good performance in diagnosis of hemorrhagic and cystic degeneration, with reported sensitivity of 100% and 80% and specificity of 86% and 98%, respectively.
Twisted Pedunculated Leiomyoma
Acute torsion of a pedunculated leiomyoma is a very rare complication of leiomyoma. A leiomyoma may twist around its stalk, resulting in sudden onset of pain due to venous congestion and then arterial compromise. The size of the myoma itself serves as a key factor for irreversible torsion. The larger size of the leiomyoma, the more difficult for spontaneous detorsion. Clinical signs, symptoms, and ultrasound findings often mimic those of ovarian torsion and depend on the degree of torsion. MR imaging can demonstrate the pedunculated leiomyoma adjacent to the uterus, its stalk extending from the mass to the uterus and a separate, normal ipsilateral ovary. The presence of “bridging vascular sign” or curvilinear/tortuous vascular structures between the uterus and the mass suggest a uterine origin of the mass. A separate, ipsilateral ovary is helpful to exclude an ovarian torsion. The lack of internal enhancement of leiomyoma helps suggest infarction secondary to a twist ( Fig. 3 ).
Pelvic Inflammatory Disease/Tubo-ovarian Abscess
Pelvic inflammatory disease (PID) is a spectrum of upper genital tract infection in women, including endometritis, salpingitis, tubo-ovarian abscess (TOA) and/or pelvic peritonitis. It usually affects young sexually active women as a result of ascending spread of microorganisms from the lower genital tract. Currently, the diagnosis remains a challenge because signs and symptoms (lower abdominal or pelvic pain, deep dyspareunia, abnormal bleeding, and abnormal vaginal or cervical discharge) are nonspecific, and present in only approximately 20% of patients. TOA is a severe form of the acute PID that causes significant morbidity and occasional mortality. Transvaginal ultrasound is generally recommended as the first-line imaging modality, whereas MR imaging is a problem-solving tool for difficult cases. Computed tomography (CT) is usually reserved in patients with peritonitis and for guidance of interventional treatment. MR imaging is more specific and more accurate for identification and characterization of complex uterine and adnexal lesions than ultrasound. A direct comparison between MR imaging and transvaginal ultrasound shows that MR imaging has sensitivity, specificity, and accuracy of 95%, 89%, and 93%, respectively. In this study, ultrasound demonstrates sensitivity, specificity, and accuracy of 81%, 78%, and 80%, respectively.
Fallopian tubes distended with pus can be clearly demonstrated on MR imaging ( Fig. 4 ) as a sausagelike structure in the parauterine regions with content of varying signal intensity. Although fluid is generally T1 hypointense and T2 hyperintense, pus may exhibit complex signal intensity on both T1-weighted and T2-weighted images. T1 hyperintensity and heterogeneous T2 signal intensity may be expected secondary to internal debris or hemorrhage. TOA can be seen as a multilocular cystic structure or an ill-defined heterogeneous mass with cystic and solid components. It often shows various signal intensity on both T1-weighted and T2-weighted images with enhancement of the walls, septae, and solid portions. Edematous change of surrounding pelvic soft tissue is usually present and seen as increased signal intensity on T2-weighted images. MR imaging has sensitivity ranging from 90% to 95% and specificity ranging from 89% to 93% for the diagnosis of acute PID. Presence of surrounding pelvic soft tissue edema, and thick/smooth and enhanced septa of the mass combining with a correct clinical context can help accurately differentiate acute PID/TOA from ovarian tumors.
Ovarian Torsion
Torsion of the ovary, either complete or incomplete, around its ligamentous support often results in compromised blood supply to the ovary. When this occurs, venous blood flow becomes obstructed, leading to ovarian stromal congestion, edema, and eventually arterial ischemia with necrosis. Ovarian torsion usually affects premenopausal women, especially those who have underlying adnexal mass. In fact, up to 81% of ovarian torsion occur on preexisting adnexal lesions such as functional cyst, corpus luteal cyst, or mature teratoma. Right-sided torsion is more common than the left side. Ultrasound is usually the first imaging modality for suspected ovarian torsion. CT and MR imaging serve as a second-line imaging test after equivocal ultrasound findings but they may be an initial imaging in patients with nonspecific presentation.
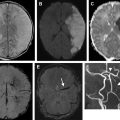
MR imaging findings consistent with ovarian torsion ( Fig. 5 ) include ovarian enlargement, edematous ovary (increased T2 signal intensity), abnormal location of the torsed ovary, twisted vascular pedicle (so-called whirlpool sign), lack of contrast enhancement, and restricted diffusion in the wall of the twisted mass. Multiple, small, peripherally located ovarian follicles may be observed, which are a result of pressure effect from stromal edema. Other MR imaging findings include abnormal uterine deviation to the side of torsion, adnexal fat infiltration, free fluid, and fallopian tubal thickening. Although MR imaging has been shown to have a good sensitivity of 86% and a positive predictive value of 100% for the diagnosis of ovarian torsion, some pitfalls have been reported. Ovarian lesions containing subacute hemorrhage, such as hemorrhagic corpus luteal cyst ( Fig. 6 ) or hypovascular tumor, may mimic torsion. Absence of a twisted vascular pedicle and preserved ovarian enhancement make the diagnosis of torsion unlikely in these cases. Infarction or degeneration of pedunculated or broad ligament leiomyoma may also mimic ovarian torsion. In these cases, identification of a normal ipsilateral ovary is the key to a correct diagnosis.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree