Overview
The male pelvis contains the urinary bladder, a portion of the ureters, musculature, vasculature, and the genitourinary system, which includes the prostate gland, seminal vesicles, scrotum, testicles, and penis.
The emphasis of this scanning protocol chapter is the genitourinary system. As part of reproduction, the male genitourinary tract provides a means to perpetuate the species. The spermatozoa are manufactured in the testes; the ductal system stores and helps propel the sperm during ejaculation via the penis; the alkaline secretions from the prostate gland and seminal vesicles help the sperm survive to complete the process of reproduction.
Anatomy
Prostate Gland and Seminal Vesicles
• The prostate gland:
• Is retroperitoneal (it lies in the portion of the abdominopelvic cavity posterior to the peritoneal sac), anterior to the rectum and inferior to the urinary bladder.
• Consists of fibromuscular and glandular tissue that surrounds the neck of the urinary bladder and prostatic urethra (portion of male urethra surrounded by prostate gland).
• Is about the size of a chestnut and conical in shape; approximately 3.5 cm long, 4.0 cm wide, and 2.5 cm anterior to posterior. The base, its broadest aspect, is superior to its apex.
1. Peripheral zone: located posterior and lateral to the distal prostatic urethra. Normally, it is the largest zone.
2. Central zone: extends from the base of the prostate to the verumontanum (landmark area near the center of the prostate gland) and surrounds the ejaculatory ducts (two ducts that transport sperm and pass through the prostate gland to empty into the prostatic urethra).
3. Transition zone: located on both sides of the proximal urethra. Normally, it is the smallest zone.
• The seminal vesicles:
• 2 convoluted, sac-like structures that lie superior to the prostate gland and posterior to the urinary bladder.
• Approximately 5 cm (2 inches) in length and less than 1 cm in diameter. They join the vas deferens ducts (part of ductal system that transports sperm) to form the ejaculatory ducts.
Scrotum and Testicles
• The scrotum:
• Is a pouch of skin that is continuous with the abdomen. It is suspended from the base of the male pelvis between the perineum (area between the anus and the scrotum) and the penis.
• Externally, the median raphe or median ridge divides the scrotum into lateral portions.
• Internally, the scrotum is divided into 2 sacs by a septum that is formed by the continuation of the external skin, superficial fascia, and contractile tissue. Each scrotal sac contains a testis, epididymis, and proximal portion of the ductus (vas) deferens (Figure 14-2).
• 2 spermatic cords extend from the scrotum through the inguinal canals and internal inguinal rings into the pelvis. Each cord contains the ductus (vas) deferens, testicular arteries, venous pampiniform plexus (veins that drain the testes and become the spermatic veins superiorly) lymphatics, autonomic nerves, and cremaster muscle fibers.
• Each testicle is:
• A male gonad. Male gonads are the organs that make the gametes (spermatozoa).
• Approximately 1.5 to 2 inches (3 to 5 cm) long, 1 inch (2 to 3 cm) wide, and 1 inch (2 to 3 cm) anteroposteriorly. Before age 12, testicular volume is less than 5 mL. With maturity, the average testicular volume is approximately 25 mL. Testicular size decreases with advancing age.
• Covered by tunica albuginea, a dense fibrous tissue which extends into the posterior testicle wall and forms the mediastinum testis and interlobar septa:
• The septa of the mediastinum radiate into the testicle and separate into 200 to 300 lobules. Each lobule contains 1 to 3 convoluted seminiferous tubules that produce sperm then empty it into the straight tubules, which lead to a network of ducts called the rete testis. This network of ducts exits the testis through the mediastinum testis into a series of coiled epididymal efferent ducts.
• The epididymis is primarily composed of the ductus epididymis a single convoluted, tightly wrapped, 1.5 inch, smooth muscle tube encapsulated by a serosal layer. When unwrapped, the tube measures about 20 feet (6 m) in length and 1.5 inches (3.8 cm) in diameter. The epididymis is connected to the superior portion of the testis and runs along the posterior aspect to the base of the testis, where it drains into the ductus (vas) deferens. The ductus epididymis is subdivided into a head, body, and tail: the head (globus major) is the larger superior portion consisting mostly of the efferent ducts that empty into the ductus epididymis; the body runs along the posterior aspect of the testis and contains the ductus epididymis; the tail (globus minor) is the smaller inferior portion, where the ductus epididymis empties into the ductus (vas) deferens.
• The ductus (vas) deferens is a thicker, less convoluted continuation of the ductus epididymis that joins with the seminal vesicles to form the ejaculatory ducts, which course through the prostate and empty into the prostatic urethra.
Penis
• The penis:
• Is composed of 3 cylindrical masses of smooth muscle and erectile tissue that enclose vascular cavities:
• 2 corpora cavernosa situated dorso-laterally and
• 1 corpus spongiosum in the midventral region, which contains the spongy urethra (longest portion of male urethra).
• The 3 corpora are bound and separated by fibrous tissue, the tunica albuginea. Superficial to the tunica albuginea is a thick fibrous envelope and a loosely applied covering of skin, called Buck’s fascia (Figure 14-3).
• Along with the urethra, receives blood from the pair of pundendal arteries, which are branches of the internal iliac arteries. The primary veins of the penis are the superficial and deep dorsal veins.
Physiology
• As part of reproduction, the male genitourinary tract provides a means to perpetuate the species.
• The male gametes or spermatozoa are produced in the testes and mature in the epididymis. The function of the ductal system is to store and help propel the sperm during ejaculation via the penis. Without the alkaline secretions from the prostate gland and seminal vesicles, the sperm could not survive to complete the process of reproduction.
• The reproductive function of the penis is to eject semen into the female vagina. During ejaculation, increased pressure within the urethra causes the urinary bladder sphincter to close, which prevents urine from being expelled into the vagina and semen from entering the bladder.
Sonographic Appearance
Prostate Gland and Seminal Vesicles
Prostate Gland
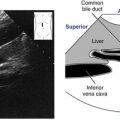
• The majority of the parenchyma of the prostate appears homogeneous and midgray, with medium-level echoes. The periurethral glandular stroma that surrounds the urethra is slightly hypoechoic relative to surrounding prostatic parenchyma. At the midline of the gland the prostatic urethra walls appear echogenic.
• A normal prostate gland should appear symmetrical with a smooth contour and well-defined margins.
• Calcifications may be seen throughout the gland in older patients.
• The central and transition zones of the prostate are not normally distinctive. The peripheral zone appears homogeneous and slightly hyperechoic relative to adjacent parenchyma.
Seminal Vesicles
• These are identified as ovoid structures with low-level echoes, just superior to the prostate gland. They appear hypoechoic relative to the prostate gland.
• They should appear symmetric in size, shape, and echogenicity.
• They are horizontally oriented, therefore, they are seen in long axis on transverse plane scans.
• They are easier to visualize when the urinary bladder is partially filled.
• The vas deferens and ejaculatory ducts may be difficult to distinguish from surrounding structures. However, when seen, the vas deferens is medial to, and has an echo texture similar to, the seminal vesicles. The ejaculatory duct will appear as bright double lines.
Scrotum and Testicles
Scrotum
• Various layers of the scrotum are not normally differentiated on ultrasound. The combination of the scrotal wall layers typically appear as a single, bright, echogenic stripe.
• The highly echogenic spermatic cord may be visualized as it courses through the inguinal canal. As mentioned, the ductus deferens may be difficult to appreciate sonographically. Color flow Doppler is useful in identifying the blood vessels within the cord.
Testicles
• The parenchyma is homogeneous with medium-level echoes similar to those of the thyroid gland. Echo texture and size of each testicle should be compared to its opposite side.
• The mediastinum testis appears as a bright line running along the long axis of the testis.

The transtesticular artery runs in a direction opposite the centripetal arteries. See Color Plate 1.
• A few millimeters of anechoic fluid visualized between the two layers of the tunica vaginalis is a normal finding.
• The epididymis appears isosonic/isoechoic or slightly hyperechoic relative to the testicle. The texture of the epididymis, however, is generally more course in appearance. Echo texture and size of each epididymis should be compared to its opposite side.
• A testicular vascular normal variant identified sonographically in 10% to 20% of cases is the transtesticular artery coursing through the testis in a direction opposite the centripetal arteries (Figure 14-4).
• Color Doppler technical considerations:
• Confirm intratesticular and epididymal flow using both color and conventional waveform analysis. Use the mediastinum testis as a point of reference when demonstrating intratesticular flow. With acute torsion less than 6 hours or chronic torsion more than 24 hours, there is absent intratesticular flow and increased peristesticular flow. Color Doppler cannot differentiate malignant hypervascularity from inflammatory hypervascularity.

• Color Doppler arterial/venous flow characteristics:
• The testis has low vascular resistance. Testicular, capsular, centripetal, and recurrent rami arteries have low resistance flow. Their waveforms are characterized by broad systolic peaks and high levels of diastolic flow similar to the internal carotid artery. Cremasteric and deferential arteries have high systolic peaks and lower levels of diastolic flow similar to the external carotid artery.

• Intratesticular veins accompany companion arteries. Their waveform is continuous or phasic.
• Spermatic cord/pampiniform plexus has minimal to moderate flow.

• The epididymis has a very slight flicker or dashes of flow.

• Testicular, deferential cremasteric, centripetal, and capsular arteries have moderate flow.

Penis
• Corpus spongiosum and corpora cavernosa appear homogeneous with medium-level echoes.
• The single corpus spongiosum:
• In axial sections, is identified at the midline surrounding the urethra, which appears slightly hyperechoic compared to the corpus spongiosum.
• Compressed by the transducer, it will appear elliptical in shape.
• The 2 corpora cavernosa:
• Are surrounded by the tunica albuginea, which appears bright and distinctive.
• Are posterior to the corpus spongiosum and appear symmetrical, round or oval, with bright borders from the tunica albuginea.
• In short axis sections, the axial, anechoic lumen of the cavernosal artery is easily identified in the center of each corpus cavernosum; their pulsations can be seen in real time.
• In longitudinal sections they appear divided by the central, linear, bright appearance of the cavernosal arterial walls.
Preparation
Patient Prep
Prostate Gland
Endorectal Sonography
The prostate gland is best evaluated by endorectal (or transrectal) sonography. Transabdominal male pelvis examinations to evaluate the prostate gland are rarely performed now because the high frequency endorectal transducer can be placed closer to the area of interest and produce superior, highly detailed images.
• The patient should have a self-administered enema before the examination. If for some reason the patient cannot have the enema, the study should still be attempted.
• Explain the examination to the patient. Verbal or written consent is required and the examination should be witnessed by another health-care professional. The initials of the witness should be part of the film labeling.
• The sonographer or physician inserts the transducer.
Scrotum


• The scrotum should be supported on a rolled towel placed between the patient’s thighs to isolate and immobilize the scrotum for scanning. Cover the penis with a towel and tape the towel to the abdominal wall.
• Explain the examination to the patient. The examination should be witnessed by another health-care professional and their initials should be part of the film labeling.
• Use warm gel as a scanning couplant.
• To scan the scrotum the sonographer’s gloved fingers should be placed underneath the scrotum and the thumb over the top of the scrotum. This hand position further stabilizes the scrotum and has the advantage of allowing correlation between a palpable mass and its sonographic findings. Also, the sonographer’s fingers are easily identified as they appear bright and highly reflective and are used as reference points for localizing masses (Figure 14-5).
Penis
• The penis should be supported on a rolled towel placed between the patient’s thighs to isolate and immobilize the penis for scanning.
• Explain the examination to the patient. The examination should be witnessed by another health-care professional and their initials should be part of the film labeling.
• Use warm gel as a scanning couplant.
Transducer
Prostate Gland
Endorectal Sonography
• 5.0 MHz or higher.
• Preparing the transducer includes providing a water path. Preparation includes one of the following 3 options:
1. Some transducer manufacturers provide a finger-like sheath that slides onto the transducer head. The sheath is secured by a small rubber band, and 20 or 30 mL of nonionized water is injected into the sheath through a pathway inside the transducer handle. Tip the transducer down and tap the water-filled sheath so any air bubbles will rise to the top and can be aspirated. Fill a condom half full with sonographic gel, then insert the sheathed transducer. Apply additional lubrication to the outside of the condom before insertion. A small rubber hose can be attached to the transducer pathway to introduce or aspirate water from the sheath to adjust for any air bubbles that might occur and cause artifacts.
2. Apply gel to the end of the transducer, then cover it with a condom. Secure the condom with a rubber band and make sure there are no air bubbles at the tip. Apply additional lubrication to the outside of the condom before insertion. Use an inner balloon filled with 30 to 50 mL of nonionized water as a water path.
3. Cover a transducer with a disposable sheath or condom and secure it with a rubber band; lubricate the outside; then insert the transducer into the rectum. Fill the sheath or condom with 30 to 50 mL of an unionized water for a water path.
• Following the examination, any tubing or stopcocks and the disposable sheath or condom covering the endorectal probe should be disposed. The probe should be soaked in an antimicrobial solution. Follow manufacturer’s instructions and infectious disease recommendations for solution type and soak time. If the sheath or condom was torn during the procedure, the probe’s fluid channels must be flushed with the antimicrobial solution.
Scrotum
• 5.0 MHz or higher, real-time, linear or a curved linear transducer.
• 7.0 MHz to 10.0 MHz is preferable for pediatric applications.
• 3.5 MHz to 7.0 MHz conventional Doppler with color flow imaging (low flow filter, scale, and optimized resolution).
• If necessary, use a gel standoff pad to improve imaging. They can be helpful when evaluating anterior lesions.
Penis
• 5.0 MHz, high resolution, real-time, linear transducer.
• 7.5 MHz, 10.0 MHz.
• Conventional Doppler with color flow imaging (low flow filter, scale, and optimized color gain).
• In some cases, a gel standoff pad may improve imaging.
Patient Position
Prostate Gland
Endorectal Sonography
• Left lateral decubitus with knees bent toward the chest.
• Lithotomy position.
Scrotum
• Supine with the legs slightly spread or in a semi frog-legged position.
• Upright.
Penis
• Supine with the legs slightly spread or in a semi frog-legged position.
• Upright.
Prostate Gland Survey