Fig. 10.1
Bähren classification. (a) Type 0 (normal), no venous reflux. (b) Type I, single gonadal vein without duplication. (c) Type II, single gonadal vein with accessory veins (gonadal, lumbar, iliac veins, IVC). (d) Type III, duplicated gonadal vein with a single trunk. (e) Type IV, competent renal/gonadal junction with reflux to collateral vessel(s). (f) Type V, gonadal vein that drains into a circumaortic renal vein
Bähren et al. [17] developed the following anatomic classification system:
Type 0 = no evidence of venous reflux on venography
Type I = reflux into a single gonadal vein without duplication (Fig. 10.2)

Fig. 10.2
A 12-year-old boy with left varicocele. Type I was demonstrated with a single gonadal vein
Type II = reflux into a single gonadal vein that communicates with accessory gonadal, lumbar, and/or iliac veins, or the vena cava (Fig. 10.3)
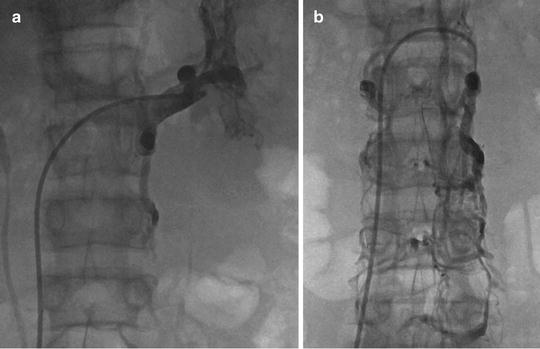
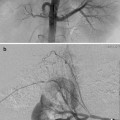
Fig. 10.3
A 14-year-old boy with left-sided varicocele. (a) Selective catheterization of the left renal vein shows the anastomosis of the internal spermatic vein (ISV) with the left renal vein. (b) ISV catheterization shows multiple collaterals with lumbar veins (type II)
Type III = reflux into a gonadal vein duplicated caudally, coalescing into a single trunk at the renal vein junction (Fig. 10.4)

Fig. 10.4
A 13-year-old boy with type III varicocele with duplicated veins coalescing into a single trunk
Type IV = competent valves at the renal/gonadal junction but reflux into a renal hilar and capsular collateral vessel that communicates with the gonadal vein (Fig. 10.5)

Fig. 10.5
A 14-year-old boy with renal hilar collateral vessels (type IV)
In our series of 93 pediatric varicoceles, we encountered 54 % type 1, 10 % type II, 17 % type III, 14 % type IV, and 5 % type V [19].
Indications for Treatment
The main indications for varicocele treatment in adolescents are pain, discomfort, testicular atrophy, and recurrence after surgical ligation. The timing of treatment is controversial in the literature. The Best Practice Policy Committee of the American Urological Association and the Practice Committee of the American Society for Reproductive Medicine recommend that adolescents and young men with a varicocele but a normal-size ipsilateral testicle or normal semen analysis, or both, should be offered annual follow-up monitoring [20].
Equipment: Occluding Agents
Many agents have been used to occlude the ISV. The most frequently used agents are Sotradecol (STS), foam, and coils [2]. Some authors also reported varicocele treatment with glue, detachable balloons, particles, and hot contrast material [2, 12, 14, 16, 21]. Selected embolic materials are described below.
Sotradecol
1 % or 3 % sodium tetradecyl sulfate creates an endothelial surface damage-induced inflammatory reaction. STS has a low risk of extravasation, systemic dispersion, and adverse reactions.
STS Foam
STS foam is a mixture of 2 mL STS, 1 mL Lipiodol, and 3 mL of air. It improves the distribution of the sclerosing agent and its contact with the endothelial wall. Gandini uses two 10 mL Luer-Lock syringes containing 1 mL of 3 % STS and 4 mL air connected through a three-way stopcock that is vigorously mixed to form the foam prior to injection.
Coils
Some authors have reported good results with coils alone. However, early recurrence will take place with the endogenous lysis of the thrombus. We suggest the use of coils in association with a sclerosing agent. Also, late recurrence is frequently related to coil erosion. In Shlansky-Goldberg et al.’s study, the technical failure was 12 % and recurrence 4 % with coils in 173 varicoceles [22].
Glue (n-Butyl Cyanoacrylate)
Glue (n-butyl cyanoacrylate) is a tissue adhesive agent. This agent is permanent; however, recanalization can be observed. Sze et al. reported no recurrence in 17 patients who had undergone embolization for postsurgical recurrence [18].
Absolute Ethanol
Absolute ethanol is a permanent agent that induces thrombosis by denaturing blood proteins, dehydrating vascular endothelial cells, and precipitating their protoplasm; the agent denudes the vascular wall.
Treatment
Surgery
surgery is performed by high retroperitoneal or transinguinal ligation of the ISV. The problem is the high frequency of venous collaterals, with either recurrence or persistence of the varicocele. Surgical recurrence rate or persistence of venous reflux in the pampiniform plexus ranges between 0 and 28 % [22]. Following a laparoscopic approach, the recurrence rate reported is 7–9 % [20], and for microsurgical technique, the recurrence rate is 0–3 % of cases [23, 24].
Percutaneous Embolization of Varicocele
Patients are treated on an outpatient basis under sedation or general anesthesia. See Chap. 3 for sedation information. Intraprocedural monitoring includes heart rate, blood pressure, and pulse oximetry.
When performing varicocele embolization, careful collimation, pulsed fluoroscopic acquisition, and appropriate gonadal shielding are important to minimize the patient dose. Videocapture is used rather than exposures.
Traditional technique involves the use of a sclerosing agent in the lower ISV and placement of coils in the proximal portion. Sandwich technique was described by Goffette et al. (Fig. 10.7) [25]. Distal occlusion is performed with a nest of coils just above the pubic ramus. Thereafter, sclerosing agent is injected to reach all potential collaterals. Finally, coil occlusion is performed proximally. This approach avoids the reflux of the sclerosing agent to the scrotum and prevents phlebitis of the pampiniform plexus. Success rate of this technique is 91 % and lack of recurrence is reported in 73 % of cases. Mazzoni et al. [21] reported no recurrence in 79.4 % and Feneley et al. in 81 % [26].


Fig. 10.7
Sandwich technique: distal occlusion is performed with coils (stainless steel: 25–5 mm –5 cm) just above the pubic ramus. Sclerosing agent (5 cc of Sotradecol) is injected. Finally, proximal coils (stainless steel: 25–5 mm –5 cm) occlusion is performed
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree