Fig. 4.1
Volume rendering (VR) should not be overemphasized as a screening tool to diagnose facial fractures. In that case, the left non-displaced condylar fracture, barely demonstrated on VR, is an easy diagnosis on panoramic radiography. Note bilateral intermaxillary fixation, left side mandibular angle fracture treated with screws and a displaced right extracapsular condylar fracture
The clear sinus sign, i.e. the absence on CT scans of sinus fluid or opacification to exclude fractures involving the sinus walls, can be used for a rapid triage of facial fractures. Generally speaking, fractures through sinus walls tear mucosal vessels producing haemorrhage; thus, in the acute phase, the absence of free fluid in a sinus cavity is an evidence against the hypothesis of a fracture. As the floor of the orbit is the roof of the maxillary sinus, the medial orbital wall is the lamina papyracea, and the orbital roof is the floor of the supraorbital ethmoidal cells or the frontal sinus; fractures may cause blood levels in these sinuses. The clear sinus sign is reliable to exclude injuries requiring surgical intervention, identifying severe facial ZMC and orbital and sinus fractures. However, it should be stressed that 10% of complex facial fractures may not have associated sinus opacification (Fig. 4.2); furthermore nasal bone and mandibular fractures cannot be ruled out at all [6].
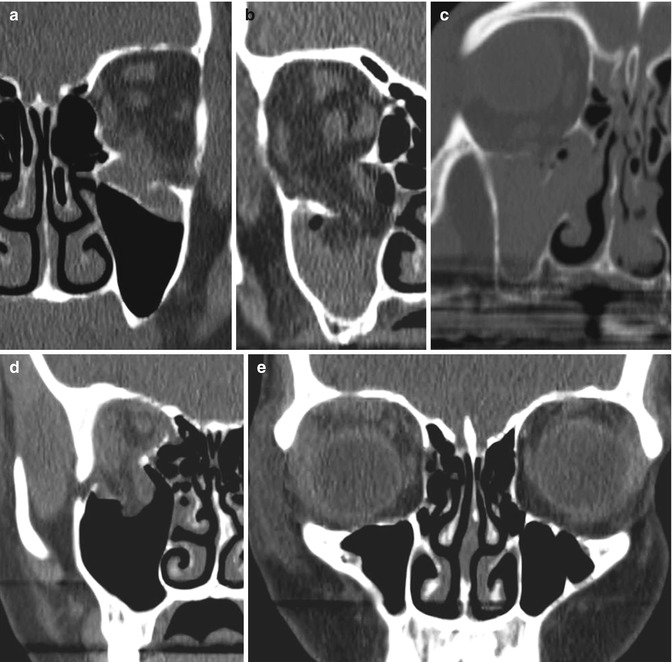
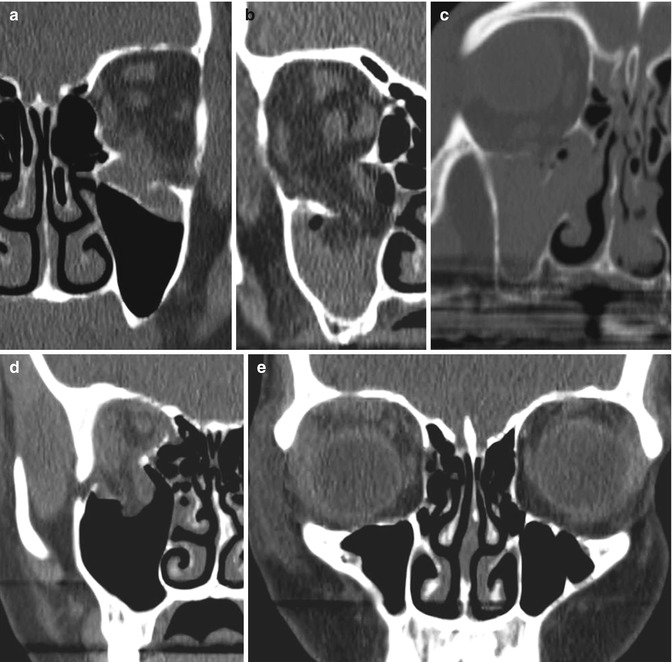
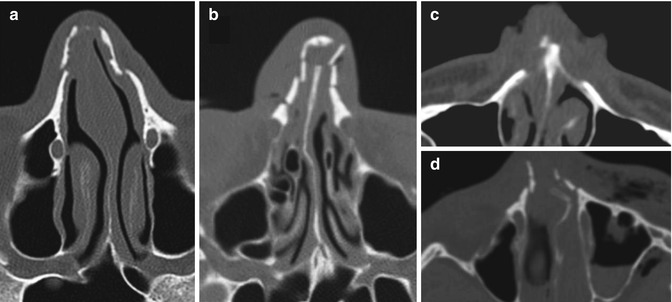
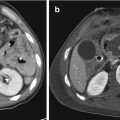
Fig. 4.2
Orbital floor “blow-out” fractures on parade. (a) Displaced fracture with subperiosteal haematoma and rounding of the inferior rectus muscle. Note the lack of haemosinus and, therefore, a false negative clear sinus sign. (b) Displaced fracture with large herniation of fat and inferior rectus muscle. (c) Displaced fracture with complete haemorrhagic opacification of the maxillary sinus. (d) Displaced fracture with herniation orbital content and hypoglobus (e), again with a false negative clear sinus sign
A note about the CT appearance of foreign bodies is mandatory before offering a systematic approach to facial fractures. Metallic foreign bodies are easy to find with CT, while glass, plastic, wood and vegetable matter have a variable density and may be overlooked. As a general rule, any density with a highly geometric shape is likely a foreign body [7]; blood and gas may be a clue to the presence of a possible foreign body. When a wooden foreign body is suspected, CT evaluation with −500 HU level and 1000–2000 HU width is recommended, given the aspected density in the range of +20 to −600 HU [7]. Apart from the special harm of foreign bodies into the orbit, delayed consequences of an overlooked, retained foreign body in other soft tissues of the face (e.g. pain, suppurative infection, tetanus) cannot be underestimated.
4.4 Orbital Fractures
Orbital fractures may rarely require emergency orbital surgery, as most of the fractures can be addressed with close observation or can be repaired after several weeks [8]. However, provided that the airway is secured and vascular injuries are excluded, orbital trauma should be addressed at the beginning of the reporting process, as a comprehensive ophthalmic clinical evaluation is usually limited in the acute polytrauma setting, especially in the unconscious patient. Therefore, the radiologist is often the primary specialist calling for globe injuries and tensive orbit.
Systematic approaches can be used in the setting of a busy emergency workflow; general radiologists taking patient responsibility “from head to toe” and even neuroradiologists having little clinical interest in head-neck imaging may take advantage from some mnemonics such as “BALPINE”—bones, anterior chamber, lens, posterior globe structures, intraconal orbit, neurovascular structures and extraocular muscles/extraconal orbit [9].
While the absence of an orbital fracture doesn’t rule out a globe injury, an eye which is intact on CT scan is likely not to have a penetrating injury, and immediate surgical intervention is probably not required [10].
Evaluation of the globe (Figs. 4.3 and 4.4) should include width of anterior chamber (decreased in corneal lacerations or anterior displacement of the lens, increased in globe ruptures), lens position (dislocation) and density (acute traumatic cataract, hypoattenuating compared with the nonaffected side), posterior chamber haemorrhage, globe deformity, intraocular air and foreign bodies (vide infra). CT provided an overall accuracy of 81% in the diagnosis of globe rupture [11]. Reference to the ophthalmologic examinations is in any case pivotal to avoid misinterpretations in case of previous ocular surgery, e.g. intraocular haemorrhage as seen on CT confused with surgical changes (Fig. 4.5).
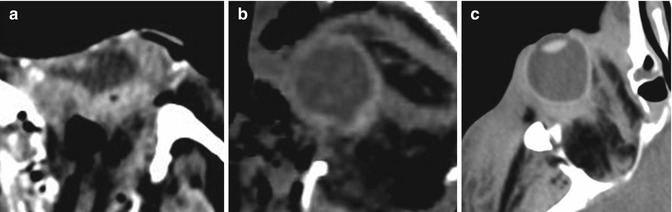
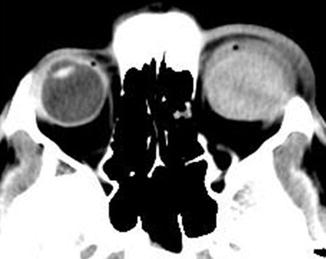
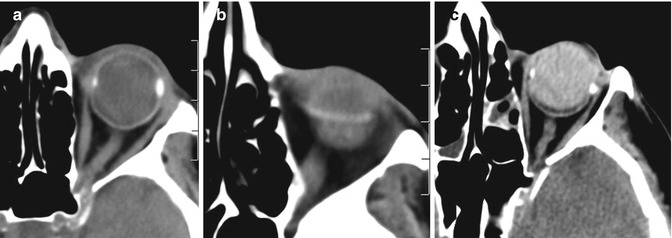
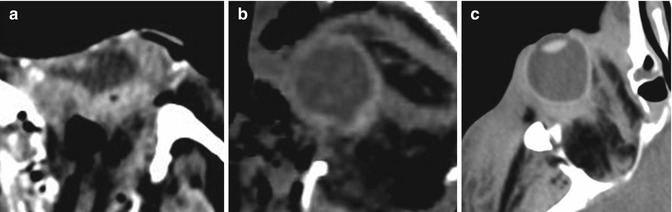
Fig. 4.3
“Flat tyre” appearance (a) and abnormal contour of the globe (b), suggesting an open globe injury. Both the eyes had eventually to be enucleated. Posterior “tenting” of the globe, secondary to posttraumatic haematoma and tension orbit (c)
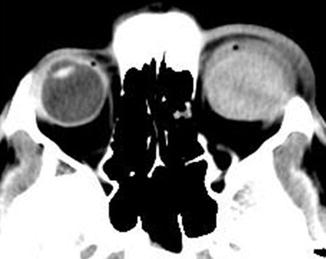
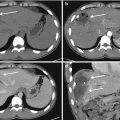
Fig. 4.4
Young firework casualty with a massive vitreous haemorrhage. Homogeneous hyperattenuation in the posterior segment of the globe and periorbital soft tissue swelling. The anterior segment is obscured
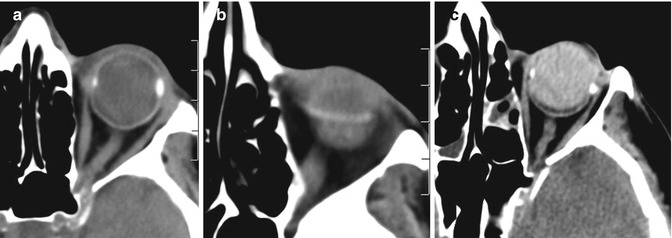
Fig. 4.5
Radiologist should familiarize with materials used to treat retinal detachment, including gas, scleral bands and silicon oil (a–c). Note the hyperattenuating silicon oil in the posterior segment of the globe, mimicking haemorrhage
After an orbital trauma, tension orbit (Figs. 4.3c, 4.6 and 4.7) can be defined as a threat to vision because of the presence of an acute and exceeding increase of orbital content (blood, air, bone, foreign bodies) stretching the optic nerve [12]. The anterior displacement of the eye (proptosis), caused by the mass effect, stretches the optic nerve, thus compromising its vascular supply and ultimately leads to ischaemic optic neuropathy. The procession of CT changes in tension orbit is described by Mancuso and Verbist [12]: (1) space-occupying process within the orbit; (2) proptosis; (3) full extended, stretched optic nerve, entirely visible all in one plane of section; and (4) optic nerve diameter diminished due to the stretching. At point 4 tension orbit is incipient, and a potential emergency surgical decompression may be warranted. By the next point, a loss of visual acuity can be predicted with near certainty: (5) posterior globe assuming a cone-shaped or tented appearance and (6) continued worsening of previous points, mainly the tenting of the globe. Even when “incipient”, direct communication with the clinical team is mandatory for the radiologist.
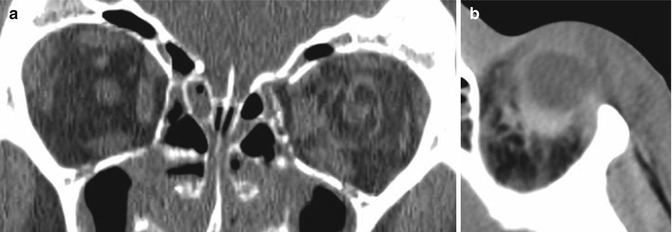
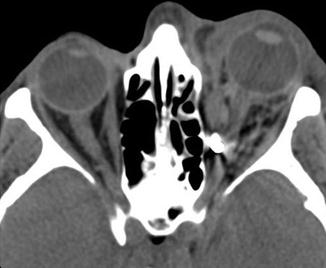
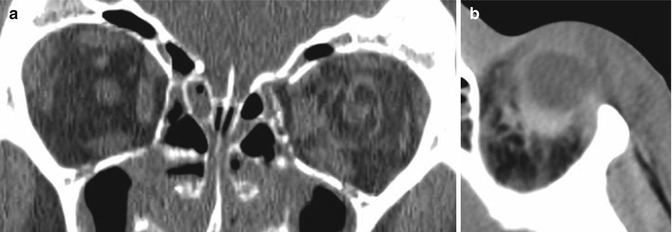
Fig. 4.6
Despite the absence of significant displaced fractures, intraconal and retrobulbar haematoma should induce a prompt clinical evaluation for tension orbit
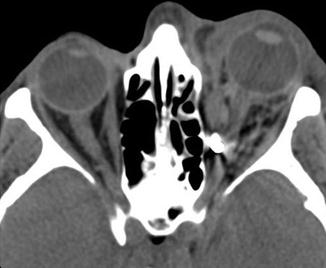
Fig. 4.7
An extraocular metallic foreign body is seen in the region of the medial rectus muscle, along the path of the optic nerve. Note the extra- and intraconal haematoma tracking along the nerve, which appears stretched, with evident proptosis
Orbital fractures can be isolated or associated with other midfacial fractures (e.g. Le Fort II and III, NOE, ZMC fractures). A solitary non-displaced fracture of an orbital wall usually doesn’t require any treatment. Displaced wall fractures may have a blow-in or a blow-out pattern.
The orbital apex, formed by the superior orbital fissure and optic canal, is the crossroad between the orbit and the intracranial structures. Fracture of this area can be associated with optic nerve impingement and intraorbital haematoma. Given the little room available in that area, even small injuries can be extremely dangerous to the optic nerve: extremely careful inspection and reporting are therefore de rigueur (Fig. 4.8).
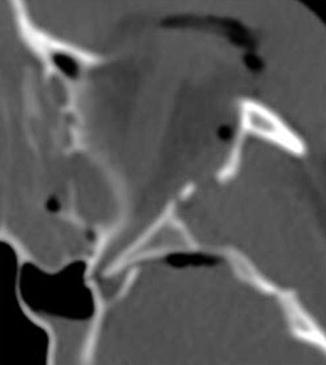
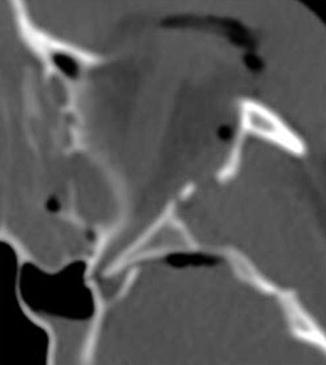
Fig. 4.8
Bone impingement of the superior orbital fissure. Such a detail may be overlooked in the bone disaster of a big facial crash but can be responsible for ptosis, proptosis, ophthalmoplegia, fixation and dilatation of the pupil, anaesthesia of the upper eyelid and forehead
Blow-out fractures (Figs. 4.2 and 4.9) are among the most common orbital fractures. They are produced by a direct impact on the orbit causing a sudden increase in intraorbital pressure. This leads most commonly to a fracture of the medial wall and/or the orbital floor. It should be noted that non-traumatic dehiscence of lamina papyracea can be found in 6.5% of population [13]. Medial and inferior rectus muscles can be trapped in the fracture, leading to restriction of gaze and diplopia. Indirect signs of blow-out fractures are orbital emphysema (from communication with adjacent air-containing sinuses), fat and/or extraocular muscle projecting as a soft tissue mass into the maxillary or ethmoidal sinuses and fluid (blood) in the sinuses. Extraocular muscles may appear swollen and round, as a result of contusive damage and lack of soft tissue support.
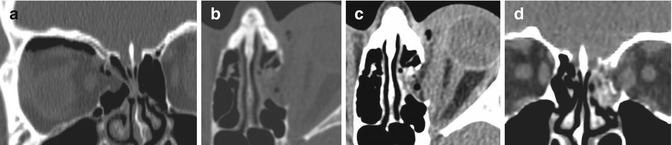
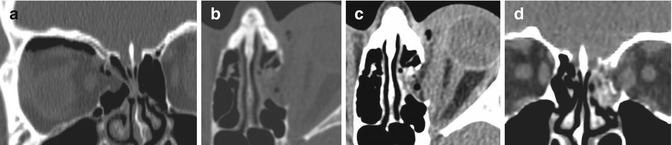
Fig. 4.9
Medial orbital wall blow-out fractures: note the variable amount of orbital emphysema and the swollen medial rectus muscle
In children a characteristic orbital floor blow-out fracture is the so-called trapdoor fracture, a greenstick fracture in which prolapsed orbital tissues may be entrapped on the maxillary sinus side of the orbital floor. These features may be easily overlooked at imaging [14].
Fracture of the orbital roof occurs in the adult population, although they are more common in children. It is often frequently associated with frontal sinus and skull base fractures, dural tears, intracranial haemorrhage and brain injuries. Direct blows to the forehead may cause inward displacement fractures of the orbital roof: these so-called blow-in fractures (Fig. 4.10) may be associated to globe injuries, and displaced bone fragments may impinge and damage the optic nerve. Prior to age 7, the frontal sinus is not pneumatized, and frontal hits can fracture the orbital roof in isolation [15]. Apart from the classic cases above-mentioned, “blow-in” and “blow-out” patterns may variably affect the orbital walls (Fig. 4.11).
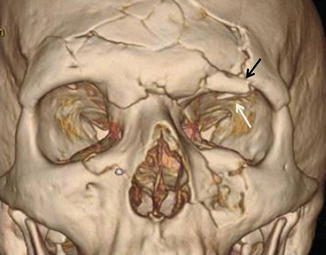
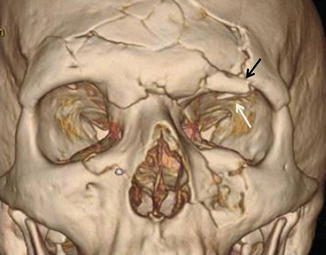
Fig. 4.10
Left superior orbital rim fracture (black arrow) with “blow-in” of the roof (white arrow) in the setting of a complex midfacial fracture involving the frontal bone. Note the reduction in the vertical dimension of the left orbit
Fig. 4.11
Although less usual than the counterparts, “blow-in” patterns may affect the floor (a) and “blow-out” the roof (b) of the orbit. Note orbital emphysema in both cases and quite extensive subperiosteal haematoma in (b), continuing in the frontal sinus
The optic nerve is vulnerable to shearing effects that may lead to traumatic optic neuropathy. The risk of traumatic optic neuropathy may be predicted by the presence of intraconal haematoma (the best predictor), intraconal emphysema, optic canal fracture, haematoma along the posterior globe and extraconal haematoma. In these cases early ophthalmologic consultation is recommended [16].
The orbit should be also screened for dilation of the ophthalmic veins, as a sign of traumatic carotid-cavernous fistula.
4.5 Frontal Sinus Fractures
Frontal sinus fractures can lead to significant complications such as meningitis, encephalitis, intracranial abscesses, osteomyelitis and mucoceles. Posterior table involvement and the presence of pneumocephalus should be noted, suggesting an associated dural tear (Fig. 4.12). Nasofrontal outflow tract injury and obstruction are to be stressed [17]. As already stated, prior to age 7, the frontal sinus is not pneumatized, and frontal hits often fracture the orbital roof in isolation [15].
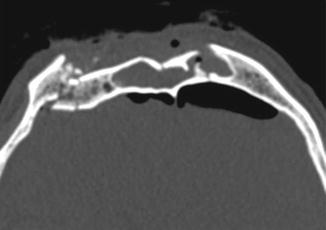
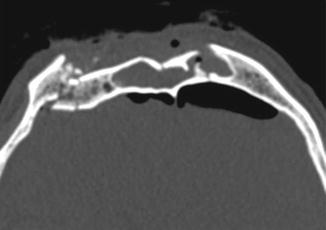
Fig. 4.12
Comminuted and displaced fracture of the anterior and posterior walls of the frontal sinus with associated opacification of the sinus and pneumocephalus, suggesting a dural tear
4.6 Midfacial Fractures
4.6.1 Nasal Bone Fractures
The nasal bones are the commonest fractured bones of the face (Fig. 4.13). Most of nasal fractures occur within the lower and thinner portion of the bones, in the transverse plane, while normal sutures and nasociliary grooves are longitudinally oriented and do not cross the midline, as fractures can. Plain films of nasal bone fractures have high rates of false positive and false negative findings and are inadequate for an accurate diagnosis of nasal bone fractures. Old nasal fractures heal by ossification in only 50% of cases, whereas the remaining heal more or less by fibrosis connecting the fragments, and thus the old fractures are visible on CT/X-rays for the rest of the patient’s life [18]. Fracture and focal thickening of the nasal septum should be carefully reported, as they may lead to haematoma, necrosis, infection, abscess and eventually airflow obstruction or nasal saddling. The anterior nasal spine is an often overlooked structure; however, it is involved in the cosmetics of the lower nose. Although treatment usually consists of a simple closed reduction, incorrect diagnoses and inadequate reductions can cause secondary deformity. Additional operation like corrective rhinoplasty or septoplasty could be needed later [19].