Maxillofacial Trauma
10.1 Introduction
Maxillofacial trauma represents a significant cause of morbidity and financial cost in the United States. More than three million people sustain maxillofacial injuries each year,1 and many of these injuries require hospital admission. In 2007, the cost of treatment of facial fractures in U.S. emergency departments was nearly one billion dollars.2
Imaging plays an important role in the management of patients with maxillofacial trauma. Proper imaging allows for the rapid diagnosis of craniofacial fractures and associated injuries. Cross-sectional imaging, particularly the use of three-dimensional (3D) reconstructions, has become vital to surgical planning. Intraoperative computed tomography (CT) has increasingly been used to provide essential anatomic information directly at the point of care. This chapter discusses the causes of maxillofacial injuries, the major patterns of facial fractures, and current imaging practices concerning maxillofacial trauma.
10.2 Epidemiology
Maxillofacial trauma accounts for a major use of health care resources in the United States, with an average hospitalization of 6 days and a mean cost of $60,000 per patient.2 Motor-vehicle collisions and assault cause most maxillofacial trauma. In industrialized nations, assault accounts for an increasing proportion of maxillofacial trauma, with increasing numbers of cases reported in some countries.3 Motor-vehicle collisions are also an increasing cause of such fractures in developing countries.3 The cause of maxillofacial fractures also may vary within a country from region to region, with interpersonal violence more frequent in urban areas and motor-vehicle collisions and falls more common in rural areas.4 Falls, sports, and work-related injuries round out the most common causes of maxillofacial trauma, with falls accounting for most maxillofacial injuries in the older population.5
The typical patient with maxillofacial trauma is a man in the third decade of life. Maxillofacial trauma affects men more than women, with male-to-female ratios reported as high as 11:1, but more commonly found in the range of two to four men affected for every woman affected.6–8 Alcohol use plays a significant factor in maxillofacial injury, with some reports finding as many as 87% of maxillofacial trauma cases to involve alcohol.9
The increased use of seat belts and air bags in automobiles has decreased the incidence of facial fractures and lacerations resulting from motor-vehicle collisions.10 An analysis of the effect of safety devices on the incidence of facial trauma found that 59% of patients with facial fractures resulting from motor-vehicle collisions did not use any safety device.11 Further, the lack of use of air bags or seat belts during motor-vehicle collision increased the incidence of facial fractures.11
10.3 Normal Anatomy
The facial bones and supporting musculature and tissues provide both function and form. The facial bones provide important protection for the brain and eyes. They house the structures necessary for sight, smell, and taste. The facial skeleton provides the framework for the vital functions of ventilation, mastication, and phonation. Lastly, the face is the portal to the outside world and is the organ of social interaction. In patients with congenital or post-traumatic facial deformity, appearance is rated as the fifth most important function of the face after breathing, vision, speech, and eating.12
The buttress system of the face is helpful in conceptualizing facial anatomy and is essential in planning surgical reconstruction. The facial buttresses are composed of regions of relatively thickened bone that support the physiologic functions of the face, such as mastication.13 They also provide targets of sufficient thickness to accommodate surgical fixation hardware.
There are four pairs of vertically oriented buttresses (▶ Fig. 10.1):
Nasomaxillary or medial maxillary buttress runs from the anterior maxillary alveolar process superiorly along the frontal process of the maxilla to the region of the glabella.
The zygomaticomaxillary or lateral maxillary buttress extends from the lateral maxillary alveolar process over the zygoma and includes the lateral orbital wall. This buttress bifurcates at the zygoma and travels posteriorly along the zygomatic arch.
Pterygomaxillary or posterior maxillary buttress is located at the posterior maxillary alveolar process and extends along the posterior wall of the maxillary sinus to the base of the pterygoids. This buttress is not surgically accessible.
Vertical mandibular buttress courses along the vertical ramus of the mandible to the mandibular condyle and skull base at the glenoid fossa of the temporomandibular joint.
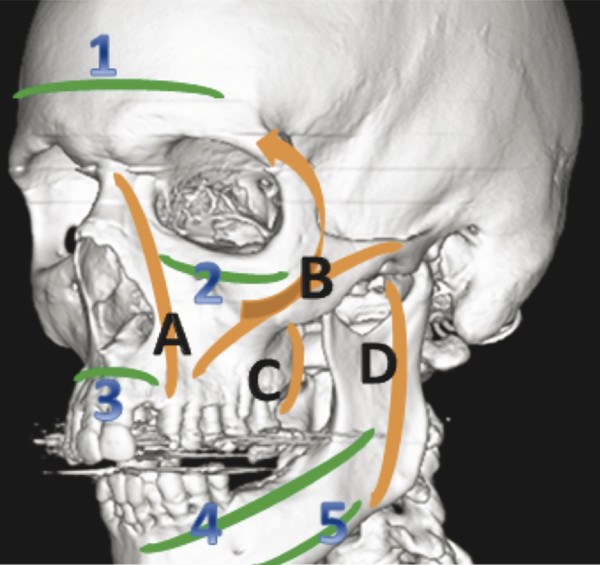
Fig. 10.1 Facial buttress anatomy. Vertical buttresses: (A) Nasomaxillary or medial maxillary buttress, (B) zygomaticomaxillary or lateral maxillary buttress, (C) pterygomaxillary or posterior maxillary buttress, (D) vertical mandibular buttress. Horizontal buttresses: (1) frontal bar, (2) upper transverse maxillary buttress, (3) lower transverse maxillary buttress, (4) upper transverse mandibular buttress, (5) lower transverse mandibular buttress.
The bony nasal septum also represents a weak vertical buttress present centrally. There are five horizontal buttresses of the face (▶ Fig. 10.1):
The frontal bar extends along the thickened frontal bone of the inferior forehead at the supraorbital ridges between the frontozygomatic sutures.
Upper transverse maxillary buttress travels along the infraorbital rims and includes the insertion site of medial canthal tendon in the medial orbit, an important structure for naso-orbito-ethmoid (NOE) fracture evaluation, described below.
The lower transverse maxillary buttress is located centrally at the palatoalveolar complex and extends laterally and posteriorly along the maxilla.
The upper and lower transverse mandibular buttresses are the lower-most buttresses. The upper mandibular buttress extends from the central portion of the mandible along the dentoalveolar arch. The lower mandibular buttress travels along the most inferior aspect of the mandible.
10.4 Imaging
CT is the modality of choice for evaluating maxillofacial trauma. CT has supplanted conventional radiography for this purpose, given CT’s speed of data acquisition, wide availability, and high sensitivity and specificity.14 In cases of severe trauma, CT examinations of the head and cervical spine are often performed concurrently. The use of a 64- or 128-slice multidetector row CT scanner allows for the maxillofacial CT to be reformatted from the source images obtained for head and cervical spine CT, thereby eliminating unnecessary radiation exposure and time.
Current multidetector CT scanners provide isometric voxel size with excellent spatial resolution of reformatted and 3D images. The CT protocol for evaluation of maxillofacial trauma should include axial images no more than 1 mm thick from the top of the frontal sinuses to the bottom of the mandible. Coronal and sagittal reformats can then be reconstructed at 0.5- to 1-mm intervals. The use of 3D reconstructions in maxillofacial trauma has steadily increased as multidetector row CT technology has advanced.
The 3D images allow easy visualization of the degree of fracture comminution and displacement, aid in localizing displaced fracture fragments, and allow evaluation of complex facial fractures in multiple planes.15 3D images are helpful for planning fracture fixation and operative reconstruction by surgeons16,17 and provide an overall “big picture” as to the extent of facial injuries.
The reported sensitivity of CT in the detection of facial fractures ranges from 45 to 97%, with specificity of near 100%. The wide range of reported sensitivity is likely due to the difficulty of visualizing some fractures in a single plane, such as identifying an orbital floor fracture using only axial images. Coronal reformats in addition to axial source images are particularly helpful in facilitating fracture detection, thus improving sensitivity. In fact, one study found that using a combination of axial images, multiplanar reconstructions, and 3D volume-rendered reformats was more accurate than using either axial images alone or axial images with multiplanar reconstructions.15 Evaluation of all three sets of images yielded a sensitivity of 95.8% and specificity of 99% for maxillofacial fractures.15
Surgeons are increasingly requesting intraoperative CT to assess the adequacy of facial fracture reduction and fixation during surgery, which allows for immediate revision and reduces the need for future revision procedures.18 Additionally, early complications such as graft malposition can be identified.
Although clearly displaced or comminuted fractures are readily detectible by CT, nondisplaced fractures can be more difficult to identify, and some fractures are occult. In these cases, recognizing the presence of soft tissue injury or secondary signs of injury may be the only way to detect these fractures. Soft tissue swelling, subcutaneous stranding, and hematoma identify the site where blunt injury occurred. Subcutaneous emphysema within the masticator space, malar region, or orbits, along with pneumocephalus, may indicate a fracture involving the paranasal sinus walls. Hemorrhagic effusions with the paranasal sinuses, manifested as hypderdense layering fluid, should always prompt a thorough search for fractures.
10.5 Facial Fractures
10.5.1 Nasal Fractures
The nasal bones are the most commonly fractured facial bones.19 Nasal fractures are commonly caused by motor-vehicle collisions, assaults, and sports-related injuries.20 The bony components of the nose include the nasal process of the frontal bone, the frontal processes of the maxilla, the ethmoid, the vomer, and the nasal bones (▶ Fig. 10.2). The distal portions of the nasal bones are susceptible to fracture because of the broadness and thinness of the bone in this region.
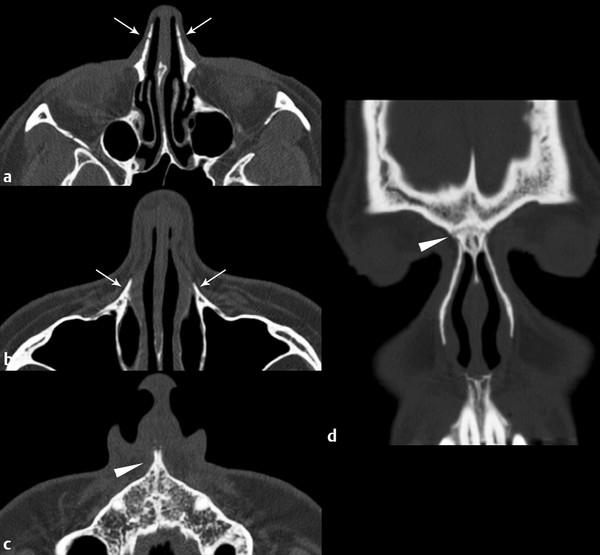
Fig. 10.2 Normal anatomy of the nasal bones on computed tomography (CT). Axial CT demonstrates (a) ethmoidal grooves within the nasal bones (arrows), which are sometimes mistaken for fractures; (b) frontal processes of the maxilla (arrows); and (c) anterior nasal spine (arrowhead). Coronal reformat (d) through the nasal bones showing frontonasal suture (arrowhead).
The signs and symptoms of nasal fractures include tenderness to palpation, palpable deformity, malposition, ecchymosis, epistaxis, and cerebrospinal fluid (CSF) rhinorrhea. Some authors suggest that imaging is not required for suspected simple nasal fractures because management is influenced chiefly by clinical rather than imaging findings.21 Clinical suspicion for other facial fractures or any concerning physical examination finding, such as copious epistaxis or rhinorrhea, dictates the need for CT evaluation.
Nasal fractures are classified clinically by severity (▶ Table 10.1). Type I injury refers to soft tissue injury without underlying damage to the bony structures of the nose. Type IIa injury is defined as a simple unilateral nondisplaced nasal bone fracture, and type IIb injury is simple bilateral nondisplaced fractures. Type III injury refers to simple displaced fractures. Type IV injury denotes a closed comminuted fracture. Type V injury describes either an open comminuted fracture or any type of nasal fracture in combination with airway obstruction, septal hematoma, CSF rhinorrhea, crush injury, or associated NOE fractures.22
| Classification | Description |
| Type I | Soft tissue injury without underlying injury to the nose |
| Type IIa | Simple unilateral nondisplaced nasal bone fracture |
| Type IIb | Simple bilateral nondisplaced nasal bone fractures |
| Type III | Simple displaced nasal bone fracture |
| Type IV | Closed comminuted nasal bone fracture |
| Type V | Open comminuted nasal bone fracture or any fracture type with airway obstruction, septal hematoma, CSF rhinorrhea, crush injury, or NOE fracture |
| CSF, cerebrospinal fluid; NOE, naso-orbito-ethmoid. Adapted from Higuera S, Lee EI, Cole P, Hollier LH Jr, Stal S. Nasal trauma and the deviated nose. Plast Reconstr Surg. 2007; 120(7, Suppl 2)64S–75S. | |
Severe nasal fractures may result in marked cosmetic defect or deformity of the nasal airway causing narrowing or occlusion. Nasal fractures may be treated conservatively or with closed or open reduction. Treatment modality depends on the fracture type and severity, as well as the presence of nasal deformity.22
Concomitant fractures of the nasal septum may occur in conjunction with nasal fractures (▶ Fig. 10.3). The nasal septum is composed predominately of the quadrangular cartilage. It is of utmost importance to identify the presence of a septal hematoma (▶ Fig. 10.4), which can lead to cartilage necrosis and saddle-nose deformity. Septal injury in pediatric patients can result in disruption of growth centers and result in delayed facial deformity.
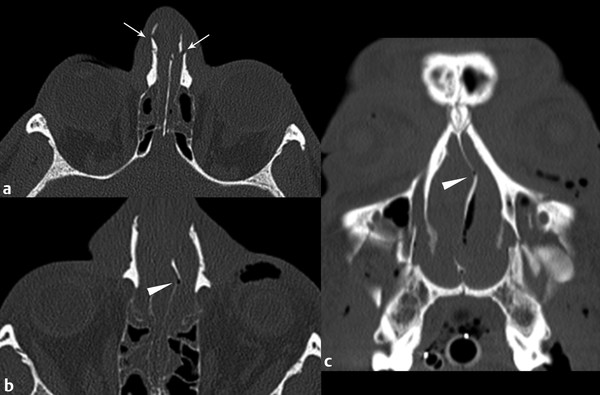
Fig. 10.3 Bilateral nasal fractures and nasal septal fracture. Axial computed tomography (CT) (a) shows bilateral, displaced nasal bone fractures (arrows). Associated nasal septal fracture is evident on axial CT (b) and coronal reformat (c) (arrowheads).
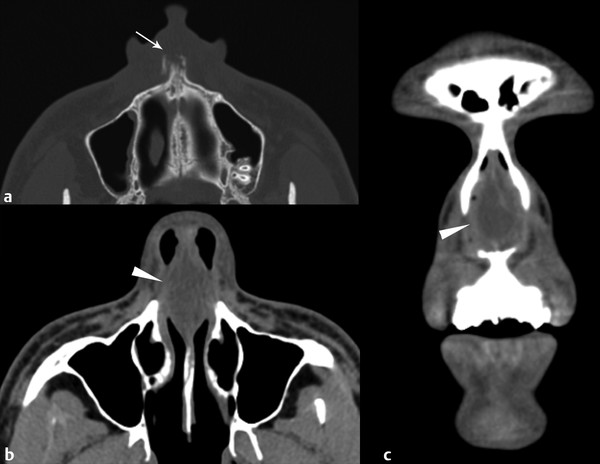
Fig. 10.4 A 16-year-old boy was punched in the nose. Axial computed tomography (CT) (a) shows fracture of the anterior nasal spine (arrow). Soft tissue algorithm CT (axial) (b), (coronal) (c) demonstrates hematoma of the nasal septum (arrowhead).
10.5.2 Naso-Orbito-Ethmoid Fractures
The NOE region is anatomically complex and includes the convergence of the orbit, nose, and maxilla. Trauma to the midface can result in fractures of this region. NOE injuries are frequently associated with other midface fractures and craniofacial injuries. The key anatomic structure within the NOE region is the central fragment of the medial orbital rim, into which the medial canthal tendon inserts.
Many complex classification systems for NOE fractures have been described. Markowitz el al23 proposed a simplified classification system that relies on the degree of comminution of the NOE central fragment (▶ Fig. 10.5) and the status of the medial canthal tendon. In type I injury, there is a large single segment central fracture fragment (▶ Fig. 10.6), and the medial canthal tendon is intact. Type II injuries are comminuted, but the medial canthal tendon insertion is spared. Type III fractures have severe comminution of the central fragment with involvement of the insertion site of the medial canthal tendon. Type II and type III injuries may not be distinguishable by imaging, as discussed later in this chapter.
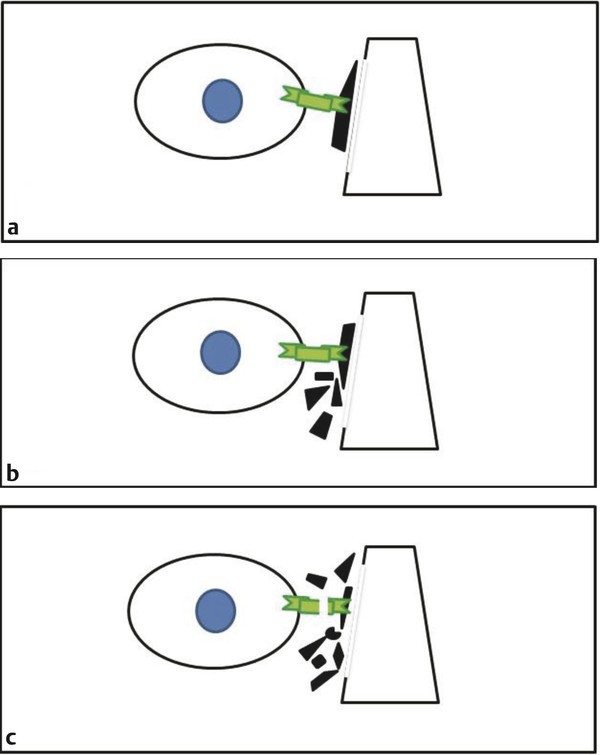
Fig. 10.5 Markowitz-Manson classification of naso-orbito-ethmoid (NOE) fractures. Iris of the eye shown in blue. Medial canthal tendon denoted in green; fracture fragments in black. (a) Type I demonstrates large central fragment. (b) Type II refers to comminuted central fragment with fragments external to medial canthal tendon insertion. (c) Type III refers to marked comminution of central fragment and disruption of medial canthal tendon.
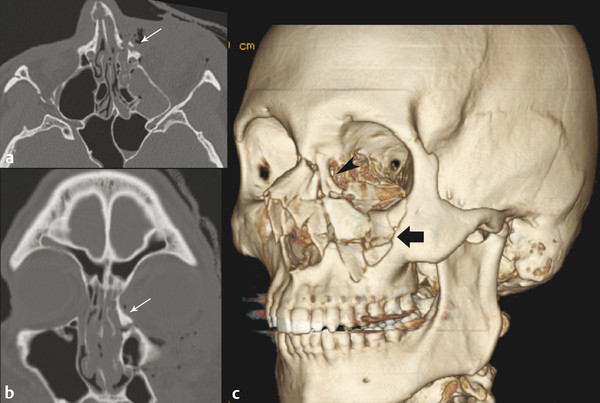
Fig. 10.6 Type I naso-orbito-ethmoid (NOE) fracture. Axial computed tomography (CT) (a) showing fracture involving medial canthal tendon attachment site (arrow). Coronal CT (b) demonstrates large single central fragment (arrow). Three-dimensional reformat CT (c) better demonstrates large central fragment (arrowhead) consistent with type I NOE fracture. Comminuted depressed fracture of the left anterior maxillary sinus wall and inferior orbital rim are also present (black arrow).
The diagnosis of NOE fracture is made by physical examination and imaging. Bimanual palpation of the NOE region may reveal mobility and crepitus, suggesting instability and the need for open reduction and fixation.24 CT is vital in the evaluation of NOE fracture. Axial and coronal series allow for assessment of bone, soft tissue injuries, and associated fractures.25 The accuracy of NOE fracture assessment is improved by evaluation of a combination of multiplanar CT and 3D volume-rendered CT.26 The medial canthal tendon itself cannot be assessed by CT, and integrity of the medial canthal tendon can be determined only during surgery. Damage to the medial canthal tendon can be inferred on imaging, however, by the degree of comminution and displacement of the central fragment (▶ Fig. 10.7).
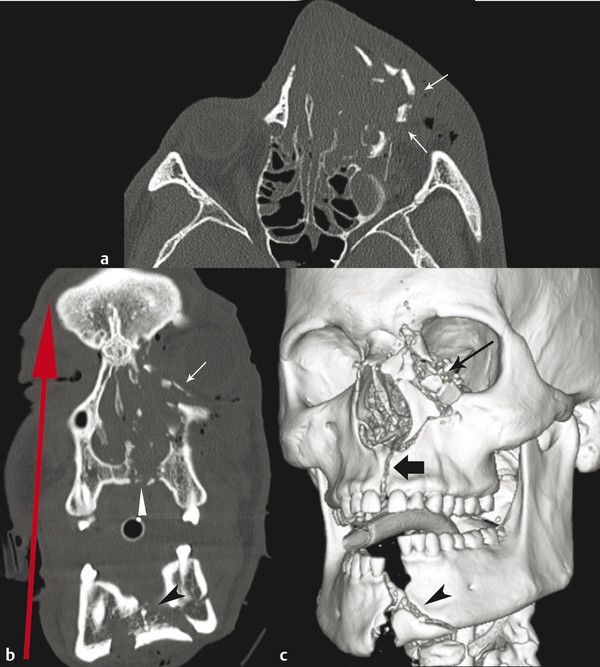
Fig. 10.7 Self-inflicted gunshot wound with type III naso-orbito-ethmoid (NOE) fracture. Axial computed tomography (CT) (a) shows comminuted and severely laterally displaced left NOE fracture (arrows). Injury to the medial canthal tendon is inferred from the comminution and displacement of fragments. Coronal reformat (b) shows additional fractures of the left nasal wall, medial orbital wall, infraorbital rim (arrow), hard palate (white arrowhead), and mandible (black arrowhead). Bullet trajectory is suggested by the pattern of fractures (red arrow). Volume-rendered reformat (c) shows comminuation and displacement of the NOE fracture (black arrow), anterior maxillary fracture extending superiorly to infraorbital foramen (thick black arrow), and comminuted, displaced symphyseal fracture of the mandible (arrowhead).
10.5.3 Zygomaticomaxillary Fractures
The paired zygomatic bones of the face comprise a central bone with four processes that abut the maxillary, temporal, frontal, and sphenoid bones. The zygomatic bone, or zygoma, forms a large portion of the lateral orbital wall and a portion of the orbital floor. The zygoma is bisected vertically by the zygomaticomaxillary buttress and horizontally by the upper transverse maxillary buttress.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree