Mediastinum
Evaluation of the mediastinum usually begins with chest radiography. The chest radiograph can confirm that there is a mediastinal abnormality and help localize it within the anterior, middle, or posterior mediastinum. Contrast-enhanced computed tomography (CT) usually suffices for further evaluation of anterior and middle mediastinal widening or a mass, although magnetic resonance imaging (MRI) can also be used to define abnormalities seen on the chest radiograph. For posterior mediastinal lesions, MRI is often the preferred study because of its ability to evaluate the relationship of a mass to intraspinal contents. Nuclear medicine studies can be helpful for evaluation of distant metastases in patients with neural crest tumors.
NORMAL ANATOMY
A review of the differences between the anatomy of the pediatric and adult chest is presented. Recognition of normal variants is important so that they are not confused with pathologic alterations.
THYMUS
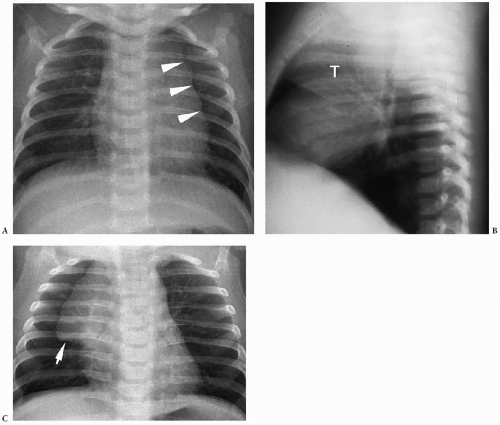
Chest radiographs of newborns commonly show a prominent thymus (Fig. 2.1). Occasionally, a wavy contour of the lateral margin of the thymus is seen. This wave sign is due to anterior costal cartilage indenting the soft thymus at several levels (Fig. 2.1B). On frontal radiographs, the thymus sometimes will have a sharp inferior margin, referred to as the sail sign (Fig. 2.1C).
Chest radiographs of newborns commonly show a prominent thymus.
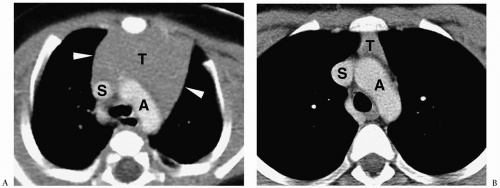
On CT and MRI in patients under 5 years of age, the thymus is often quadrilateral shaped with convex or straight margins (1,2). In older children, it assumes a triangular or arrowhead configuration with straight or concave margins (Fig. 2.2). With rare exception, the left lobe is larger than the right. Prior to puberty, the thymus appears homogeneous with an attenuation value equal to that of chest wall musculature. After puberty, areas of heterogeneity due to fatty infiltration may be seen. The signal intensity of the prepubertal thymus is slightly greater than that of muscle on T1-weighted images and slightly less than or equal to that of fat on T2-weighted and fat-suppressed images. After puberty, the T1-weighted signal intensity increases, reflecting fatty replacement (2). Ultrasonography shows a characteristic appearance of echogenic foci or septae within hypoechoic parenchyma (3).
Thymic lobar thickness (the largest dimension perpendicular to the long axis of the lobe) decreases with age, decreasing from 1.50 ± 0.46 (SD) cm for the 0- to 10-years age
group to 1.05 ± 0.36 cm for patients between 10 and 20 years of age (1). Thymic lobar width (largest dimension parallel to the long axis of the lobe) shows little change with age.
group to 1.05 ± 0.36 cm for patients between 10 and 20 years of age (1). Thymic lobar width (largest dimension parallel to the long axis of the lobe) shows little change with age.
Occasionally the thymus may extend into the superior or the posterior mediastinum.
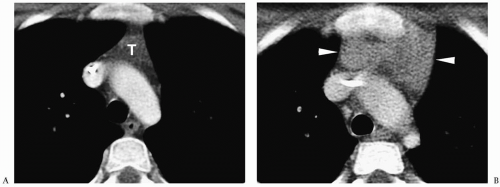
Ectopic location is uncommon, but occasionally the thymus may extend into the superior mediastinum, simulating adenopathy, or into the posterior mediastinum, simulating neuroblastoma. Demonstration by CT or MRI of a continuous margin between the aberrant thymus and the thymic tissue in the anterior mediastinum and the lack of compression of adjacent mediastinal structures supports the diagnosis of ectopic thymus (Fig. 2.3).
LYMPH NODES
Mediastinal lymph nodes generally are not seen on CT scans or MRI in children prior to puberty, and their presence should be considered abnormal. In adolescents, small nodes up to 1.0 cm in the longest axis can be seen. Nodes are of soft tissue attenuation on CT and have signal intensity between muscle and fat on both T1- and T2-weighted images.
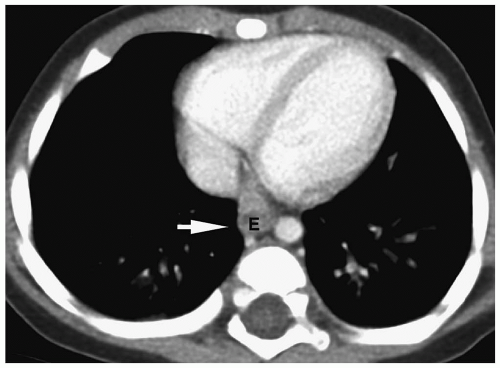
AZYGOESOPHAGEAL RECESS
The contour of the azygoesophageal recess varies with patient age. The contour of the recess is convex laterally in children under 6 years of age, either convex or straight (noncave) in children between 6 and 12 years of age, and most often concave or adultlike in adolescents and young adults (ages 12 to 20 years) (4) (Fig. 2.4). The variation in appearance of the
azygoesophageal recess may relate to the size of the azygos vein or the esophagus and the degree to which they intrude into the recess.
azygoesophageal recess may relate to the size of the azygos vein or the esophagus and the degree to which they intrude into the recess.
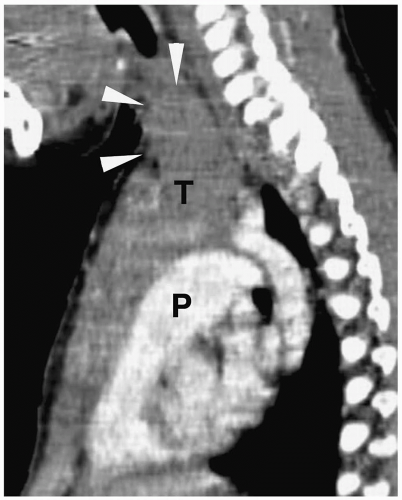 Figure 2.3 Superior thymic extension in 3-month-old boy. Sagittal contrast-enhanced CT scan shows the thymus (T) extending into the base of the neck (arrowheads) (P, pulmonary outflow tract). |
MEDIASTINAL MASSES
MEDIASTINAL PATHOLOGY
A mediastinal masses in children are usually lymphoma, neurogenic tumor, or cyst of foregut origin. Abundant mediastinal fat, aneurysms, or tortuosity of the mediastinal vessels are rare in children. Fat-containing masses in children usually are teratomas. Rarely, they represent thymolipomas or herniation of omental fat through the foramen of Morgagni. Lesions with near-water attenuation values include pericardial cysts, thymic cysts, lymphangiomas, and duplication cysts of foregut origin. When a mass has attenuation value or signal intensity equal to that of soft tissue, a specific pathologic diagnosis generally is not possible. Determining the location of the mass in the mediastinum, however, can narrow the differential diagnosis.
Lymphoma, neurogenic tumor, and cyst of foregut origin are the common mediastinal masses in childhood.
ANTERIOR MEDIASTINAL MASSES: SOFT TISSUE ATTENUATION
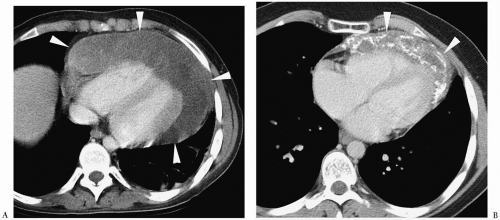
The anterior mediastinum is the most common site of thoracic masses in children, and most of these arise in the thymus (1,2,5,6). The chest radiographic appearance of most thymic masses is mediastinal widening on the frontal radiograph and a substernal opacity on the lateral radiograph (Fig. 2.5).
The anterior mediastinum is the most common site of thoracic masses in children.
Lymphoma
Lymphoma is the most common cause of an anterior mediastinal mass of soft tissue attenuation in children, with Hodgkin disease occurring 3 to 4 times more frequently than non-Hodgkin lymphoma. Approximately 70% of children with Hodgkin disease have intrathoracic involvement at clinical presentation, and the mediastinum is involved in >95% of cases. About 40% of pediatric patients with non-Hodgkin lymphoma have chest disease at diagnosis, and only 50% of this disease involves the mediastinum. Hodgkin disease usually causes enlargement of the thymus or anterior mediastinal nodes, whereas non-Hodgkin lymphoma predominantly affects middle mediastinal lymph nodes.
Lymphoma is the most common anterior mediastinal mass in children.
On CT and MRI, the infiltrated thymus appears as an enlarged, quadrilateral gland with convex or multilobulated margins (Fig. 2.6) (7,8). Usually, both lobes of the thymus are enlarged, but on occasion thymic infiltration predominantly affects one lobe. Thymic and nodal calcification can be seen in untreated lymphoma, but more often it is a
post-treatment sequela (Fig. 2.7) (9). Rarely, thymic lymphoma has large cystic components, presumably due to ischemic necrosis secondary to rapid tumor growth. Lymphoma shows little enhancement after intravenous administration of contrast medium. Lymphadenopathy in other mediastinal compartments and pleural effusion are common associated findings.
post-treatment sequela (Fig. 2.7) (9). Rarely, thymic lymphoma has large cystic components, presumably due to ischemic necrosis secondary to rapid tumor growth. Lymphoma shows little enhancement after intravenous administration of contrast medium. Lymphadenopathy in other mediastinal compartments and pleural effusion are common associated findings.
Lymphoma shows little enhancement after administration of contrast medium.
 Figure 2.5 Hodgkin disease, thymic infiltration. A, Posterior-anterior and B, lateral chest radiographs show a large anterior mediastinal soft tissue mass (arrowheads) and left pleural effusion. |
Successfully treated lymphomas usually decrease in size, but the mediastinum may not return to normal on serial CT examinations (7,10). Differential diagnostic considerations in these cases include fibrosis versus persistent or recurrent lymphoma. Serial CT examinations can often distinguish between these two conditions. In general, masses due to fibrosis remain stable or decrease in size, whereas tumors are likely to increase in size.
Magnetic resonance, gallium-67 scintigraphy, and positron emission tomography (PET) with 2-[F-18]-fluoro-2-deoxy-D-glucose (FDG) have been used to assess treatment response in the instances in which CT is not diagnostic (11,12,13,14). Posttreatment fibrosis has low signal intensity (similar to that of muscle) on T1- and T2-weighted and fat-suppressed sequences, whereas active neoplasm has high signal intensity on T2-weighted sequences. However, increased signal intensity is not specific for tumor and it also may be associated with infection, hemorrhage, acute radiation pneumonitis, necrosis, and immature fibrotic tissue. Gallium and FDG accumulate in viable tumor, but not in fibrotic tissue.
Thymic Hyperplasia
Thymic hyperplasia in children is most often “rebound” hyperplasia associated with chemotherapy, particularly therapy with corticosteroids (15,16). The initial response to steroid therapy is depletion of lymphocytes from the cortical portion of the gland. Thymic hyperplasia results when the cortisone levels return to normal and lymphocytes repopulate the cortex. Rebound hyperplasia can occur during the course of chemotherapy or several months after the completion of therapy. Rare causes of hyperplasia include myasthenia gravis, red cell aplasia, and hyperthyroidism.
Thymic hyperplasia in children is most often “rebound” hyperplasia associated with chemotherapy.
Hyperplasia produces diffuse enlargement of the thymus with preservation of the normal shape (Fig. 2.8). The attenuation value, signal intensity, and scintigraphic activity of the hyperplastic thymus are similar to those of the normal organ and hence are not helpful in differentiating tumor and hyperplasia. It is the absence of other active disease and a gradual decrease in thymic size on serial imaging studies that supports the diagnosis of rebound hyperplasia as the cause of thymic enlargement (7).
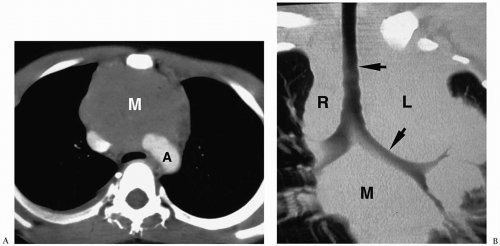
Thymoma
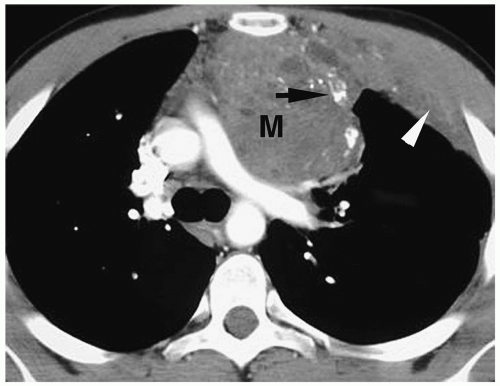
Thymomas account for less than 5% of pediatric mediastinal tumors. Virtually all thymomas are benign and arise sporadically. Rarely, they are found in association with myasthenia gravis, red cell aplasia, or hypogammaglobulinemia. CT findings of benign thymoma range from a focal soft-tissue mass bulging the lateral thymic margin to a large lobulated mass, totally replacing the thymus (17). Sometimes they contain calcifications and cystic areas, representing necrosis or hemorrhage. On T1-weighted MR images, thymomas have signal intensity similar to that of muscle. On T2-weighted and fat-suppressed images, the signal intensity approaches that of fat. The CT and MRI appearance of invasive (i.e., malignant) thymoma is that of an anterior mediastinal mass associated with mediastinal or chest wall extension or metastatic implants along mediastinal, pleural, or pericardial surfaces, usually limited to one side of the thoracic cavity (Fig. 2.9). The presence of tumor extension or metastases helps to separate benign and invasive thymomas.
Thymomas account for less than 5% of pediatric mediastinal tumors.
Miscellaneous Soft-Tissue Attenuation Lesions
Other causes of a diffusely enlarged thymus with soft tissue attenuation are leukemia and Langerhans cell histiocytosis.
Thyroid abnormalities are rare causes of an anterior mediastinal mass in children. In childhood, intrathoracic thyroid gland is more likely to represent true ectopic thyroid tissue rather than substernal extension of a cervical thyroid gland. The CT features of intrathoracic thyroid are a well-defined, intensely enhancing soft tissue mass anterior to the trachea.
Thyroid abnormalities are rare causes of an anterior mediastinal mass in children.
ANTERIOR MEDIASTINAL MASSES: FAT ATTENUATION
Germ-Cell Tumors
Germ-cell tumors are the second most common cause of an anterior mediastinal mass in children and the most common cause of a fat-containing lesion. Approximately 90% of germ-cell tumors are benign and either dermoid cysts (containing only ectodermal elements) or teratomas (containing tissue from all three germinal layers). Most are found within or adjacent to the thymus.
Germ-cell tumors are the most common cause of a fat-containing mediastinal lesion.
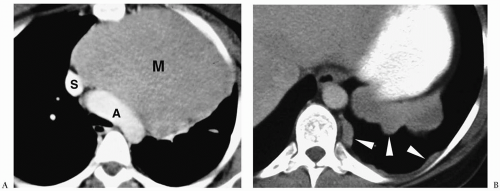
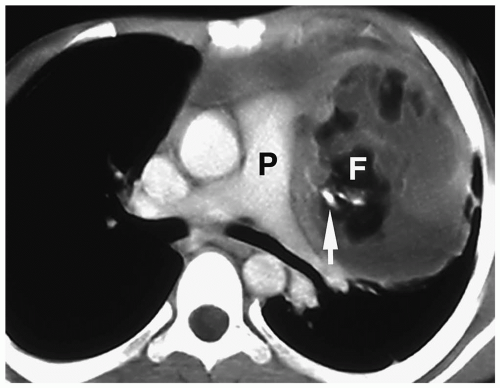
On CT, benign dermoid cysts and teratomas have well-circumscribed margins, thick walls, and heterogeneous contents, containing an admixture of fluid, fatty tissue, and calcification (Fig. 2.10) (16,18,19). A fat-fluid level and amorphous bone or
teeth occasionally can be seen within these tumors. Soft tissue elements are not a dominant component of a benign teratoma. On MRI, germ-cell tumors are heterogeneous masses with variable signal intensities depending on the relative amounts of fluid and fat. Fluid usually has a signal intensity less than or equal to that of muscle on T1-weighted images, although it can be greater than that of muscle if the contents contain blood or proteinaceous material. Fluid usually is hyperintense to fat on T2-weighted and fat-suppressed images. Fatty tissue shows high signal intensity on both T1- and T2-weighted images and absent signal on fat-suppressed sequences. Calcification and bone have low signal intensity on all imaging sequences.
teeth occasionally can be seen within these tumors. Soft tissue elements are not a dominant component of a benign teratoma. On MRI, germ-cell tumors are heterogeneous masses with variable signal intensities depending on the relative amounts of fluid and fat. Fluid usually has a signal intensity less than or equal to that of muscle on T1-weighted images, although it can be greater than that of muscle if the contents contain blood or proteinaceous material. Fluid usually is hyperintense to fat on T2-weighted and fat-suppressed images. Fatty tissue shows high signal intensity on both T1- and T2-weighted images and absent signal on fat-suppressed sequences. Calcification and bone have low signal intensity on all imaging sequences.
Benign teratomas have heterogeneous contents, containing an admixture of fluid, fatty tissue, and calcification.
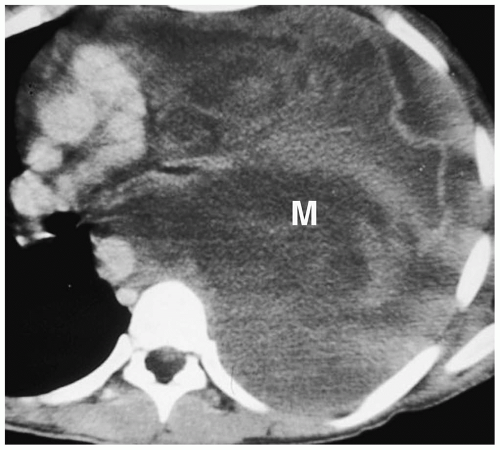
Approximately 10% of germ-cell tumors are malignant. A malignant teratoma generally appears on CT and MRI as a poorly defined, predominantly soft tissue mass, sometimes containing calcification and fat (Fig. 2.11). Other malignant germ-cell tumors arising in the anterior mediastinum are seminoma, embryonal cell carcinoma, choriocarcinoma, and endodermal sinus (yolk sac) tumor. The nonteratomatous tumors typically tend to be heterogeneous, soft-tissue density masses, often containing low-density areas of necrosis (Fig. 2.12). Calcifications are relatively uncommon. Malignant germ-cell tumors invade and encase mediastinal structures.
Approximately 10% of germ-cell tumors are malignant. Malignant teratoma appears as a poorly defined, predominantly soft tissue mass.
Thymolipomas
Thymolipoma is an uncommon cause of an intrathymic tumor (20). Pathologically, this tumor contains mature fat and strands of thymic tissue. Most cases in the pediatric population occur in the second decade and are discovered incidentally on plain radiographs. The tumor often is large, extending caudally to the diaphragm and may mimic cardiomegaly or a cardiophrenic mass. On CT and MRI, it appears as a heterogeneous mass containing fat and some soft tissue elements. Thymolipoma does not compress or invade adjacent structures.
Lipoblastoma
Lipoblastomas contain immature adipose tissue and fibrous septa. They are found in infants and young children, usually in the extremities or trunk, but they may involve the mediastinum (21). On CT and MRI, lipoblastomas are heterogeneous masses containing an admixture of fat and soft tissue. The patient’s age helps to separate this lesion from thymolipoma, which has a similar appearance.
ANTERIOR MEDIASTINAL MASSES: FLUID ATTENUATION
Cystic Hygroma
Mediastinal cystic hygromas (lymphangiomas) are developmental tumors of the lymphatic system that occur in the antero-superior mediastinum and are almost always inferior extensions of cervical hygromas (22). Isolated mediastinal involvement is rare, occurring in about 1% of cases. On CT, they appear as nonenhancing, thin-walled, multiloculated masses with a near-water attenuation value. On MRI, cystic hygroma has a signal intensity equal to or slightly less than that of muscle on T1-weighted images and greater than that of fat on T2-weighted or fat-suppressed images (Fig. 2.13). Contrast enhancement is absent unless the lesion contains vascular components or is infected. Hemorrhage can cause a sudden increase in tumor size and can increase the CT attenuation or the T1-weighted MR signal intensity. Other findings include infiltration of adjacent soft tissues and encasement of mediastinal structures. Occasionally, marked dilatation of adjacent veins is noted (23).
Mediastinal cystic hygromas are usually inferior extensions of cervical hygromas.
Thymic Cysts
Thymic cysts usually are congenital lesions resulting from persistence of the thymopharyngeal duct, but they can occur after trauma or thoracotomy. Characteristically, they are thin-walled, homogeneous masses of near-water density on CT (Fig. 2.14), low signal intensity on T1-weighted MR images, and high signal intensity on T2-weighted and fat-suppressed sequences. The attenuation value or the signal intensity on T1-weighted images may be higher than that of simple cysts if the contents of the cyst are proteinaceous or hemorrhagic. Multiple thymic cysts have also been described in children with HIV infection and Langerhans cell histiocytosis (24,25).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree