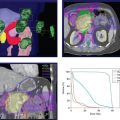
FIGURE 11-3. CTV1, CTV2, and CTV3 delineation in a patient with unknown head and neck primary cancer with right neck mass TxN2bM0 who received definitive IMRT.
1. INTRODUCTION
• Neck node metastasis of unknown primary comprises 3% to 9% of head and neck malignancies. Jugulodigastric and midjugular lymph nodes are the most frequent sites.1
• The most common histology is squamous cell carcinoma (SCC), representing 75% of cases, followed by undifferentiated carcinoma and adenocarcinoma.1,2
• The possible site of origin can be estimated from the histology of the neck node, although the biopsy often reveals a poorly differentiated neoplasm. Lymphoma should also be excluded by proper immunohistochemical staining.
• A solitary upper jugular chain is the most common site because most head and neck cancers spread to this area first. This metastasis site is uncommon for tumors below the clavicle.3
• A mass between the angle of the mandible and the tip of the mastoid suggests origin in the nasopharynx, oropharynx, parotid, occasionally malignant melanoma, or other skin cancers.
• The oral cavity, larynx, and hypopharynx should be included as likely sites for the mass in the subdigastric region.
• Bilateral upper neck nodes usually originate from the nasopharynx, base of tongue, soft palate, supraglottic larynx, and pyriform sinus.
• A solitary submandibular mass suggests a primary site of origin in the oral cavity, lip, or nasal vestibule, or a primary submandibular salivary gland tumor. A solitary submental node is rare.
• A mass in the mid-neck region suggests a primary site from the larynx or hypopharynx or, less commonly, from the thyroid or cervical esophagus, or a tumor originating below the clavicle.
• A solitary lower neck mass is commonly metastatic from the chest or abdomen. A solitary spinal accessory mass suggests a nasopharyngeal site. Squamous cell carcinoma in the parotid lymph nodes is always from a skin or parotid gland cancer.
2. DIAGNOSIS AND STAGING SYSTEM
• Physical examination and assessment under anesthesia conducted by an experienced otolaryngologist can elucidate a primary site in more than 50% of patients with cervical lymph node metastasis.4,5 In the absence of physical or radiographic suspicion, pan-endoscopy with biopsies yields a 17% detection rate.5
• Mendenhall et al.4 reported that the sites of primary tumor found through this process were at the tonsillar fossa and base of tongue in 82% of patients. Repeat pan-endoscopy did not seem to increase the detection rate.
2.1. Imaging
• Repeated examinations and contrast-enhanced computed tomography (CT) or magnetic resonance imaging (MRI) scans are essential for finding primary lesions. CT or MRI to look for a possible primary site follows a diagnosis of squamous cell carcinoma. If the biopsy is not definitive, CT or MRI may redirect the workup.
• The CT or MRI examination should be performed with at least 3-mm sections from the nasopharynx through the entire neck. MRI is used as a supplement for focused evaluation of suspicious regions, but not necessarily when the CT results are positive or normal.
• With negative routine clinical examination and CT, positron emission tomography (PET) detects carcinoma in 5% to 25% of patients, whereas ipsilateral tonsillectomy detects carcinoma in approximately 25% of patients. Laser-induced fluorescence imaging with pan-endoscopy and directed biopsies shows encouraging results but requires further investigation. PET has an overall staging accuracy of 69%.6
• The use of FDG-PET in the detection and radiotherapy planning for treatment of squamous cell carcinoma and other malignancies of unknown origin in the head and neck have recently been reviewed.7–10 This has also involved the use of PET/CT imaging which gives a higher positive detection rate.11 Kwee et al.7 advise a confirming biopsy in the case of a PET/CT positive lesion.
2.2. Biopsies
• If thorough clinical and radiological exams are unable to detect a primary, patients should undergo direct laryngoscopy and exam under anesthesia. Directed biopsies should be performed including those of nasopharynx, base of tongue, supraglottic larynx, and pyriform sinuses, in addition to a bilateral tonsillectomy.
• In a study of 87 patients who presented with cervical node metastases from an unknown primary, 26% of patients were found to have tonsil primaries diagnosed with tonsillectomy.12 Tonsillectomy is particularly important in patients with biopsy samples positive for p16 due to the association of human papillomavirus (HPV) with oropharyngeal cancers.13
• Molecular markers are increasingly being used to assist in the identification of the origin of the disease. A recent study14 examined a wide panel of proteins related to carcinogenesis and tumor environment to assist in determining the origin of unknown primary cancers.
2.3. Staging
• In 2010, the American Joint Committee on Cancer issued its new (7th edition) TNM staging guidelines.15 The nodal staging for neck metastases are substantially similar to the previous (6th edition) guidelines. Readers are urged to consult the new guidelines for details.
3. GENERAL MANAGEMENT
3.1. Surgical Management
• Data from surgery alone series revealed a median nodal recurrence rate of approximately 34% and a 5-year overall survival rate of approximately 66%.5,16–18 The crude mucosal carcinoma emergence rate was approximately 25% (30/121 patients).
• Selected patients, especially those with pathologic N1 disease with no extracapsular extension, can be treated adequately with surgery alone.17
3.2. Irradiation Alone
• Grau et al.5 reported a group of 213 patients treated with radiation alone. The 5-year actuarial mucosal carcinoma emergence rate was 16%, the nodal relapse rate was 50%, and the survival rate was 37%. It should be noted that series using radiation alone have more unfavorable prognostic factors.
3.3. Surgery and Irradiation
• Colletier et al.19 reported a series of 136 patients who received radiotherapy after nodal excision or neck dissection. The mucosal carcinoma emergence rate was 10%, the nodal failure rate was 9%, and the 5-year overall survival rate was 60%.
3.4. Radiotherapy to Ipsilateral Neck
• Weir et al.20
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree