Miscellaneous
DIFFUSE BREAST CHANGES
Changes that affect the breast diffusely can be difficult to perceive mammographically, particularly if the process is bilateral and evolving slowly. Comparison with prior films can be helpful if studies are viewed in sequence. These changes are characterized by increases in the overall density of the breast parenchyma, thickening of the trabecular pattern (Kerley B lines) and thickening of the skin. In some women, increases or decreases (shrinking) in the perceived size of the breast accompany these changes. The overall compressibility of the breast may be decreased, and the techniques needed to penetrate the tissue and thickened skin increase. As the kilovoltage is increased to penetrate the tissue adequately, contrast decreases.
Diffuse breast changes include increases and decreases in the perceived size of the breast and are often reflected by differences in the technique needed for adequate exposure.
Ultrasonographically, skin thickening is appreciated readily, although it may require use of the standoff pad: the hypoechoic central band of the skin increases in width. The hyperechoic stripes superficial and deep to the hypoechoic band do not change in thickness. Skin thickening may be associated with dilated, anastomosing lymphatic channels seen as hypoechoic to anechoic, thin tubular structures just deep to the deep hyperechoic stripe of the skin. No flow is seen in these structures with Doppler. These changes may be associated with disruption of the normal breast architecture, increases in tissue echogenicity, and in some patients, focal findings. During real-time scanning, changes of pitting edema can be seen from the pressure applied on the breast with the transducer. Some benign causes of diffuse breast changes are listed in Box 8.1.
On physical examination, peau d’orange changes reflecting edema may be apparent diffusely involving the breast or, less commonly, localized to the dependent portion of the breast. Depending on the underlying cause of the diffuse change, additional findings may be apparent on physical examination.
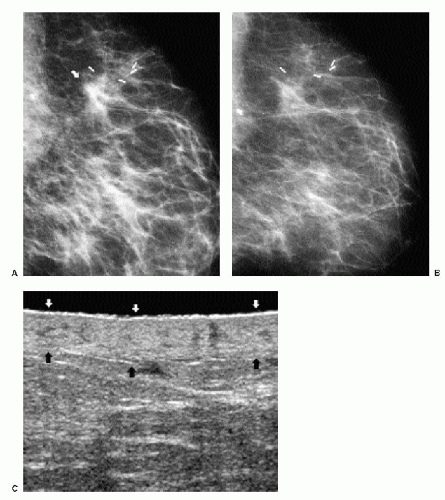
Radiation therapy is probably one of the most common benign causes of diffuse breast changes. It is typically unilateral, limited to the treated breast. On physical examination, the breast is “tanned”; there may be associated tenderness, and surgical changes are present at the lumpectomy site and, commonly, the axilla. Distortion, spiculation, and metallic clips at the lumpectomy site (Figure 8.1) accompany the skin and trabecular thickening. Diffuse changes are typically seen in the acute setting and slowly resolve over the first 2 years following completion of therapy. Residual skin thickening is seen in 20% to 40% of patients 2 years after the lumpectomy (1,2). Increases in density, combined with trabecular and skin thickening, that develop after the first 2 years following radiation therapy need to be evaluated carefully and may warrant a biopsy to exclude recurrent disease.
Box 8.1: Benign Causes of Diffuse Breast Changes
Radiation therapy
Congestive heart failure
Superior vena cava (SVC) obstruction (SVC syndrome)
Axillary adenopathy with lymphatic obstruction
Trauma
Mastitis
Granulomatous mastitis (rare)
Giant cell arteritis (rare)
Scleroderma (rare)
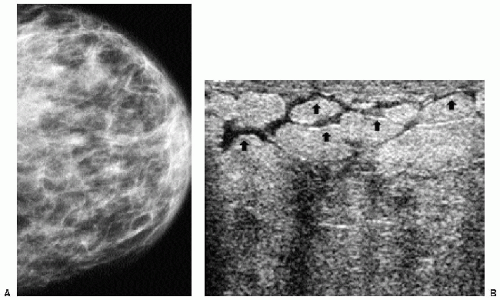
Patients with congestive heart failure can present with unilateral (Figure 8.2) or, more commonly, bilateral (Figure 8.3) diffuse breast changes, findings of peripheral edema, and shortness of breath. Obtaining technically acceptable images with no blurring is made even more difficult in these patients because of the shortness of breath. The breast is not usually very tender on exam. With successful treatment of the congestive heart failure and peripheral edema, the changes noted in the breast can resolve rapidly. If the patient is lying preferentially on one side for long periods of time, the edema may be more pronounced or limited to the dependent breast. With significant congestive heart failure, the periareolar region can become quite dense on the mammogram (Figure 8.3D); this is a finding we have not seen with many other conditions.
In more than 80% of patients, complete or partial obstruction of the superior vena cava is caused by superior mediastinal tumors, including adenocarcinoma of the lung, lymphoma, thyroid carcinoma, thymomas, and teratomas. Less common causes include chronic fibrotic mediastinitis that is idiopathic or secondary to tuberculosis, histoplasmosis, or drugs (e.g., methysergide); thrombophlebitis related to indwelling central venous catheters or pacemaker wires; aortic arch aneurysms; and constrictive pericarditis. Symptoms include swelling of the neck and face, headaches, visual disturbances, and obstructive venous drainage of the head, neck, and upper extremities. Facial flushing and dilation of anterior chest wall veins secondary to collateral flow may develop. Diffuse breast changes and dilated venous structures may be seen mammographically in these patients, more commonly involving the right breast; however, it can be a bilateral process. With a similar mechanism, axillary adenopathy with lymphatic obstruction can lead to diffuse breast changes limited to the ipsilateral breast.
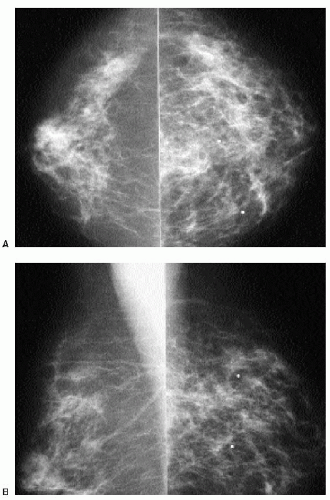
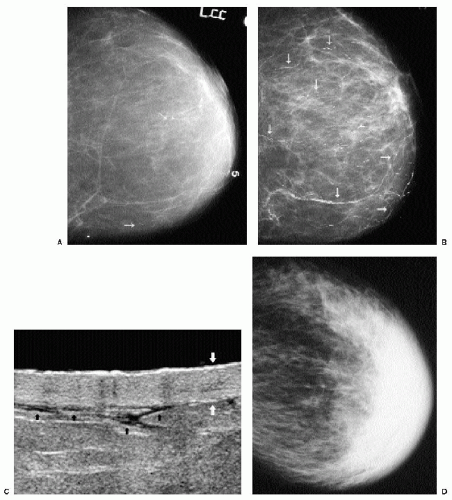 Figure 8.3 Congestive heart failure, bilateral. A. Left craniocaudal view shows a predominantly fatty pattern with some scattered, benign, large, rodlike calcifications (arrows) and no vascular calcification. The cassette number (5) can be seen on this view. B. Left craniocaudal view 4 years after image in part A. The patient presents with shortness of breath. Trabecular pattern is prominent compared with prior study, and extensive vascular calcification (arrows mark some of the calcified vessels) is now seen. No additional rodlike calcifications have developed. Although the right films are not shown, this is a bilateral process. C. A standoff pad is used to evaluate skin and subcutaneous tissue. Ultrasound demonstrates skin thickening (white arrows). Hypoechoic band is thickened. Superficial and deep hyperechoic stripes seen at the tip of the white arrows are unchanged. Anastomosing lymphatic channels (black arrows) are seen just deep to skin. D. Different patient. This 89-year-old patient presented with left breast swelling. Increased density, diffuse trabecular thickening, and marked thickness and density are noted in the periareolar region and anterior portion of the breast. Findings are bilateral, although less pronounced on the right (not shown). |
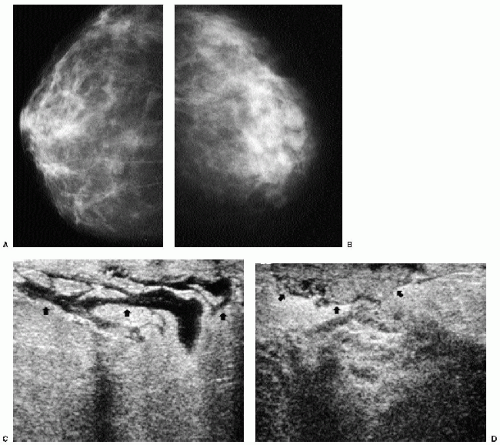
Patients with acute bacterial mastitis present with diffuse breast tenderness that may preclude an adequate mammogram because the patient is unable to tolerate significant compression. Diffuse changes may be present (Figure 8.4). On physical examination, the breast is erythematous and warmer than the contralateral breast. On ultrasound, skin thickening may not be a prominent feature; however, dilated lymphatics and disruption of
the normal breast architecture with areas of hyperechogenicity and hypoechogenicity may be seen. Although mastitis is more commonly seen in patients who are lactating, it can be seen in women of all ages. An antibiotic that covers aerobic and anaerobic organisms is used in patients who are not lactating. We follow these patients closely to ensure that an abscess requiring drainage does not develop and that there is complete resolution of the symptoms and findings after antibiotic therapy. Some patients require two courses of antibiotics for complete resolution.
the normal breast architecture with areas of hyperechogenicity and hypoechogenicity may be seen. Although mastitis is more commonly seen in patients who are lactating, it can be seen in women of all ages. An antibiotic that covers aerobic and anaerobic organisms is used in patients who are not lactating. We follow these patients closely to ensure that an abscess requiring drainage does not develop and that there is complete resolution of the symptoms and findings after antibiotic therapy. Some patients require two courses of antibiotics for complete resolution.
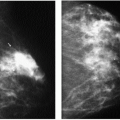
Granulomatous mastitis is an uncommon cause of diffuse breast changes (Figure 8.5) and is usually unilateral. Clinically, patients present with a mass that may be tender or, less commonly, with diffuse breast tenderness in the absence of focal findings. Patients are relatively young, and in many, the disease presents within 6 years of pregnancy. The etiology
is unknown; however, some have suggested an autoimmune reaction, undetected organisms, or the use of oral contraceptives. Histologically, granulomatous mastitis is characterized by noncaseating granulomas limited to the perilobular regions; no microorganisms are identified in the tissue. In addition to diffuse breast changes, other reported mammographic findings include one or multiple masses and large, focal areas of asymmetry. On ultrasound, findings in granulomatous mastitis include multiple, relatively circumscribed lesions with a tubular configuration or irregular hypoechoic lesions with shadowing (3).
is unknown; however, some have suggested an autoimmune reaction, undetected organisms, or the use of oral contraceptives. Histologically, granulomatous mastitis is characterized by noncaseating granulomas limited to the perilobular regions; no microorganisms are identified in the tissue. In addition to diffuse breast changes, other reported mammographic findings include one or multiple masses and large, focal areas of asymmetry. On ultrasound, findings in granulomatous mastitis include multiple, relatively circumscribed lesions with a tubular configuration or irregular hypoechoic lesions with shadowing (3).
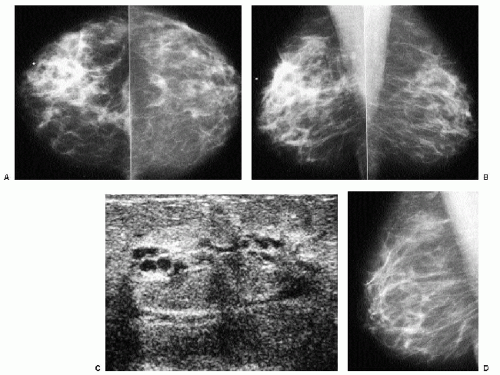
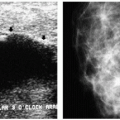
Giant cell or temporal arteritis is another rare cause of diffuse breast changes (Figure 8.6). It may be a unilateral or bilateral process, and biopsy usually demonstrates granulomatous inflammatory changes surrounding the arteries (4). This is a systemic panarteritis involving medium and large vessels in patients older than 50 years of age. The temporal arteries and other extracranial branches of the carotid artery are usually involved. Patients present with headaches, scalp tenderness, visual symptoms, jaw claudication, throat pain,
and asymmetry of arm pulses. If blindness occurs, it is often irreversible. Patients have an elevated sedimentation rate with a normal white blood cell count, and about half have associated polymyalgia rheumatica. Elevated doses of prednisone are used in the treatment of symptoms and are helpful in minimizing visual disturbances.
and asymmetry of arm pulses. If blindness occurs, it is often irreversible. Patients have an elevated sedimentation rate with a normal white blood cell count, and about half have associated polymyalgia rheumatica. Elevated doses of prednisone are used in the treatment of symptoms and are helpful in minimizing visual disturbances.
Box 8.2: Malignant Causes of Diffuse Breast Changes
Inflammatory carcinoma (infiltrating ductal carcinoma)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree