Despite the prevalence of the mood disorders, the underlying neuropathology is still poorly understood. This article describes abnormalities in brain activation that have been reported in neuroimaging studies of patients with depression and bipolar illness. Functional changes have been identified in regions important for neural networks underlying emotional processing, including frontal, subcortical, and limbic regions. The interpretation of neuroimaging studies in mood disorders is limited by potential confounding factors including medication effects, duration of illness, comorbidity, and gender.
Despite the prevalence of mood disorders, the underlying neuropathology is still poorly understood. The past decade has witnessed a substantial reappraisal of theoretical accounts of the neural underpinnings of these disorders, driven in part by the application of novel neuroimaging methods, which have allowed for the identification of both pathophysiologic factors and treatment effects in psychiatric patients. While neuroimaging research investigating major depression and bipolar disorder compared with nonpsychiatric populations shows significant regional activation differences, the reliability and sensitivity of the brain responses identified thus far limit the ability of imaging as a clinical tool. The pattern of brain changes documented in these disorders suggests that altered functional systems may play an important role in the manifestation of mood disorders.
The category of mood disorders includes a range of symptoms and syndromes; however, it is widely held that bipolar and unipolar affective disorders are the most prevalent and debilitating neuropsychiatric illnesses, and are among the leading causes of disability worldwide. Altered neurocognitive and affective functioning have consistently been documented in patients with these illnesses . Both disorders are usually recurrent and sometimes chronic; multiple episodes or prolonged periods of impaired functioning are the rule rather than the exception. Depressed individuals report recurrent feelings of deep despair and show a decrease in focused attention and goal-directed or motivated behavior across multiple areas of functioning, often resulting in social isolation and reduced work productivity . The hallmark of bipolar disorder is intense, repetitive cycling of mood states, such as depression, mania, hypomania, and mixed states. A manic episode is characterized by elevated, expansive, or irritable mood, and is usually accompanied by altered cognitive processing, heightened energy levels, higher sex drive, increased activity level, pressured thought and speech, and distractibility. Unlike depressed individuals, manic patients show increased interest in pleasurable activities and a resultant increase in reward-directed behavior. Thus, manic and depressive episodes involve a complex mix and interplay of mood and motivational, cognitive, somatic, and behavioral symptoms .
There are multiple factors (ie, genetic, developmental, and environmental) that can have synergistic actions and can contribute to the etiology of mood disorders. The involvement of limbic brain regions has been posited for over a century; nevertheless, contemporary models implicate more widespread functional interactions among neocortical, limbic, and subcortical brain regions in the pathogenesis of affective illness . While neuroimaging investigations of patients with affective disorders have reported regional activation differences when compared with control subjects, the number of empirical studies remains limited. Further, the identification of specific locations and direction of the activation changes in these patients has been inconsistent. The application of multiple image modalities and the heterogeneity of patient groups have contributed to the conflicting findings in mood disorders.
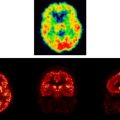
A number of seminal neuroimaging studies on patients with affective disorders employed single-photon emission computed tomography (SPECT) and positron emission tomography (PET) investigations. Many of these studies have examined brain function in subjects during a resting state, rather than during the completion of challenge paradigms, which measure brain activation and response to specific tasks. Nevertheless, findings from these studies have implicated specific cortical regions in the pathophysiology of affective disorders and provide a basis for more focused investigation. Magnetic resonance (MR) imaging methods including functional (fMRI) imaging and diffusion tensor imaging (DTI) have become the preferred modality for psychiatric research applications for several reasons. Compared to other techniques, MR imaging provides much higher spatial resolution, superior contrast and soft tissue imaging capability, fine gray-white matter distinctions, and clear distinction of white matter pathology than other techniques . As it uses no ionizing radiation, MR techniques are well suited for repeated studies of patients, and are safe to use in children and adolescents. Additionally, MR techniques allow the flexibility of imaging in multiple anatomical planes without having to physically reposition a subject, and therefore have been used to verify and expand initial findings from other neuroimaging investigations that involved exposure to radiation. The application of fMRI protocols in combination with challenge paradigms provides a safe and effective means by which to observe regionally specific effects in the brain. One notable advantage of this method is the precise functional localization as a result of increased image quality and the minimization of error due to interindividual anatomic variability. Intrasubject averaging of data can also be used to increase the signal-to-noise ratio and improve test sensitivity to illness or treatment-related differences.
It is beyond the scope of this article to review all neuroimaging studies or biological measures that have been reported in relevant areas of investigation. For example, considerable work has been completed on the physiology of mood induction, the effects of sleep deprivation, and the parsing of cognitive processes associated with mood change. These areas of study have made important contributions to our understanding of affective illness. However, the focus of this chapter will be on recent fMRI findings in the two most prominent affective disorders, major depression and bipolar disorder, with a special emphasis on brain areas and neural networks that contribute to emotional processing deficits related to mood disorders.
Models of affective illness
The interpretation of neuroimaging data from patients with affective illness is dependent on the model within which it is viewed. A number of conceptual models have been hypothesized to describe the neurobiology of depression. One important theoretical approach has been to examine the association between stress and depressive symptoms. Clinical investigators have demonstrated that patients suffering from major depression have elevated cortisol levels and abnormalities of the hypothalamic-pituitary-adrenal (HPA) axis. Sustained elevated glucocorticoid levels associated with chronic stress have been shown to damage hippocampal neurons, significantly reducing dendritic branching and spines of pyramidal neurons in the CA3 area . These data are consistent with the observations that depressed individuals frequently display memory impairments. Moreover, alterations in hippocampal function may lead to decreased hippocampal inhibition over the HPA system, which in turn would further increase glucocorticoid levels and hippocampal damage. The effects of stress are only partly mediated by glucocorticoids, and stress-related changes in the corticotropin-releasing factor and brain-derived neurotrophic factor (BDNF) likely contribute additive effects in generating symptoms of depression (also, see reference for review). These findings are of particular interest, given that reduced hippocampal volumes have been shown in patients with depression . While the mechanism for hippocampal shrinkage in depression is not fully understood, changes in glial and neuronal morphology, as well as reduced neurogenesis and increased apoptosis could all contribute to hippocampal volume reduction . These findings provide a context for understanding human neuroimaging studies of depressed patients showing deficits in hippocampal function and increased activation of the amygdala .
A second, complementary approach to conceptualizing mood disorders is to view them as the result of a disruption in brain reward circuitry. In this model, key nodes in the circuitry include the nucleus accumbens (NAcc), ventral tegmental area (VTA), hypothalamus, and amygdala. The NAcc and the VTA are part of the mesolimbic dopaminergic pathway and project to the ventral pallidum (VP), an output nucleus of the striatum. VTA neurons also project to amygdala and areas of the prefrontal cortex (PFC).
The NAcc and the mesolimbic dopaminergic pathway have been implicated in mediating rewarding characteristics of stimuli . The dopamine hypothesis originally emphasized the role of dopamine in reward processes and in the mediation of primary motivational characteristics of natural stimuli . Subsequent investigations focused on emotional (“anhedonia”) and motivational aspects of disrupted dopaminergic transmission ; however, recent animal studies indicate that interference with dopamine transmission does not affect fundamental aspects of primary motivation . Rather, the dopaminergic transmission in the NAcc, which is part of a forebrain circuitry that also includes the basolateral amygdala and anterior cingulate cortex, has been shown to be involved in motivation-mediated behavioral activation, effort-related processes, and instrumental learning processes related to reinforcement acquisition .
Human research also suggests that NAcc is related to an array of emotional and motivational stimuli . Using event-related fMRI, Knutson and colleagues showed that the anticipation of reward but not the delivery of reward activated the NAcc in healthy subjects. Similarly, anticipation of a pleasant taste but not the actual reward produced activation in dopaminergic midbrain, striatum, and posterior dorsal amygdala . Activation of NAcc/striatum was also reported in anticipation of an aversive stimulus . Therefore, human studies produced findings similar to those from animal research, suggesting that ventral striatal mechanisms are related to the anticipatory and activating effects of stimuli .
In contrast to the imaging findings in healthy subjects, responses in the mesolimbic dopaminergic circuitry appear to be altered in depression. For example, ventral striatal activation is not seen in response to pleasant visual stimuli in patients with depression , but activation of the ventral striatum/pallidostriatum has been reported in patients with unipolar depression attending to pictures of sad facial affect . Brain activity increased in a linear fashion in response to increasingly intense sad faces , and pharmacologic treatment reversed the changes seen in depressive patients . Moreover, amygdalar and ventral striatal activation correlated with measures of anhedonia .
In an effort to conceptualize mood alterations in both manic and depressed states, recent models have suggested that two major groups of brain regions—a “dorsal” and a “ventral” network—account for the formation and modulation of the varied symptoms of affective illness. Within this framework, depression is hypothesized to involve both hypoactivation of dorsal prefrontal regions and hyperactivation of ventral prefrontal regions, particularly in the left hemisphere . Manic states are thought to be characterized by lower activation on the right side than on the left, and greater ventral cingulate cortex activation than dorsal cingulate cortex activation . Mood stabilization for both clinical states may require augmentation of hypoactive dorsal brain regions as well as increased control of hyperactive ventral areas. Because the dorsal cortical and ventral limbic compartments are reciprocally connected, treatments that target either system would be expected to result in clinical improvement. Furthermore, treatments that affect other cortical or subcortical brain regions that project to both the dorsal and ventral systems could also lead to compensatory normalization in the overall circuitry. In line with this perspective, the rostral subdivision of the cingulate cortex has been hypothesized to play a critical role in treatment response because of its reciprocal connectivity and putative regulatory relationship with the dorsal and ventral networks . In summary, a disrupted balance between the dorsal/ventral circuitry as well as hemispheric laterality have been hypothesized to underlie affective disorders, and have been examined using neuroimaging techniques.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree