Case presentation
A 4-year-old female presents with 1 week of left-sided abdominal and hip pain. She was evaluated at an outside facility 5 days ago, had plain abdominal radiography, and was diagnosed with constipation. She then returned 2 days later with continued fever but was noted to have difficulty ambulating and reported generalized back pain. She had a urinalysis done that was reportedly concerning for a urinary tract infection. She was prescribed antibiotics but continued to have fever and back pain. She was then evaluated by her primary provider, who noted that the child was not toxic-appearing but did have difficulty ambulating secondary to pain, which she apparently localized to her left hip and lower back. The physician obtained plain radiographs of the lumbar spine and a one-view image of the pelvis. A diagnosis of toxic synovitis was made and scheduled ibuprofen was recommended.
Despite scheduled ibuprofen, the child continued to have intermittent febrile episodes and pain, prompting a visit to the emergency department. On examination, she is well appearing and in no acute distress. Her temperature is 98 degrees Fahrenheit, heart rate is 130 beats per minute, respiratory rate is 22 breaths per minute, and blood pressure is 102/75 mm Hg. She has no abnormal abdominal findings. Her musculoskeletal examination shows no signs of trauma, swelling, or erythema. She has good range of motion of all her extremities, including the lower ones, and there is no tenderness to palpation of the extremity or the joints. She has no spinal tenderness. When you ask the child to walk, she refuses at first but then walks several steps and stops, complaining of lower back and left hip pain.
The mother states that the child has been in good health and denies prior illness or trauma. There is no report of dysuria, incontinence, weakness, numbness, or difficulty with balance.
Imaging considerations
Plain radiography
Plain radiography is often obtained as a first-line imaging modality for patients with back pain and difficulty ambulating. However, it is not useful in the detection of a spinal epidural abscess. If there is associated osteomyelitis, cortical changes to the bone may be seen 2–3 weeks after the onset of illness. , The disc space may be narrowed on plain radiography, but this is not sensitive or specific for a spinal epidural abscess. ,
Computed tomography (CT)
CT is not a first-line imaging modality in patients with a suspected infectious spinal process, such as a spinal epidural abscess. However, if magnetic resonance imaging (MRI) is not available, CT may be an alternative and is often obtained when another process is being considered, such as appendicitis or another intra-abdominal condition, that may make ambulation difficult. CT may be able to visualize a spinal abnormality due to infection, but it lacks sensitivity and specificity. , CT may be used to guide abscess drainage. ,
Magnetic resonance imaging
Gadolinium-enhanced MRI is the modality of choice for patients with suspected spinal epidural abscess and has a reported sensitivity and specificity of greater than 90%. A spinal epidural abscess appears as an isointense or hypointense collection on T1-weighted images and hyperintense on T2-weighted images.
Ultrasound
This modality is not recommended for the evaluation and detection of a spinal epidural abscess.
Radionucleotide scanning (bone scan)
This modality is not a first-line imaging test, having been replaced by MRI, and has little role in the diagnosis of an epidural abscess. However, a bone scan may be indicated in cases where there is clinical suspicion of distantly located osteomyelitis. Some authors have advocated obtaining a bone scan if there is abscess-associated osteomyelitis, given the anatomic field limitations of MRI. ,
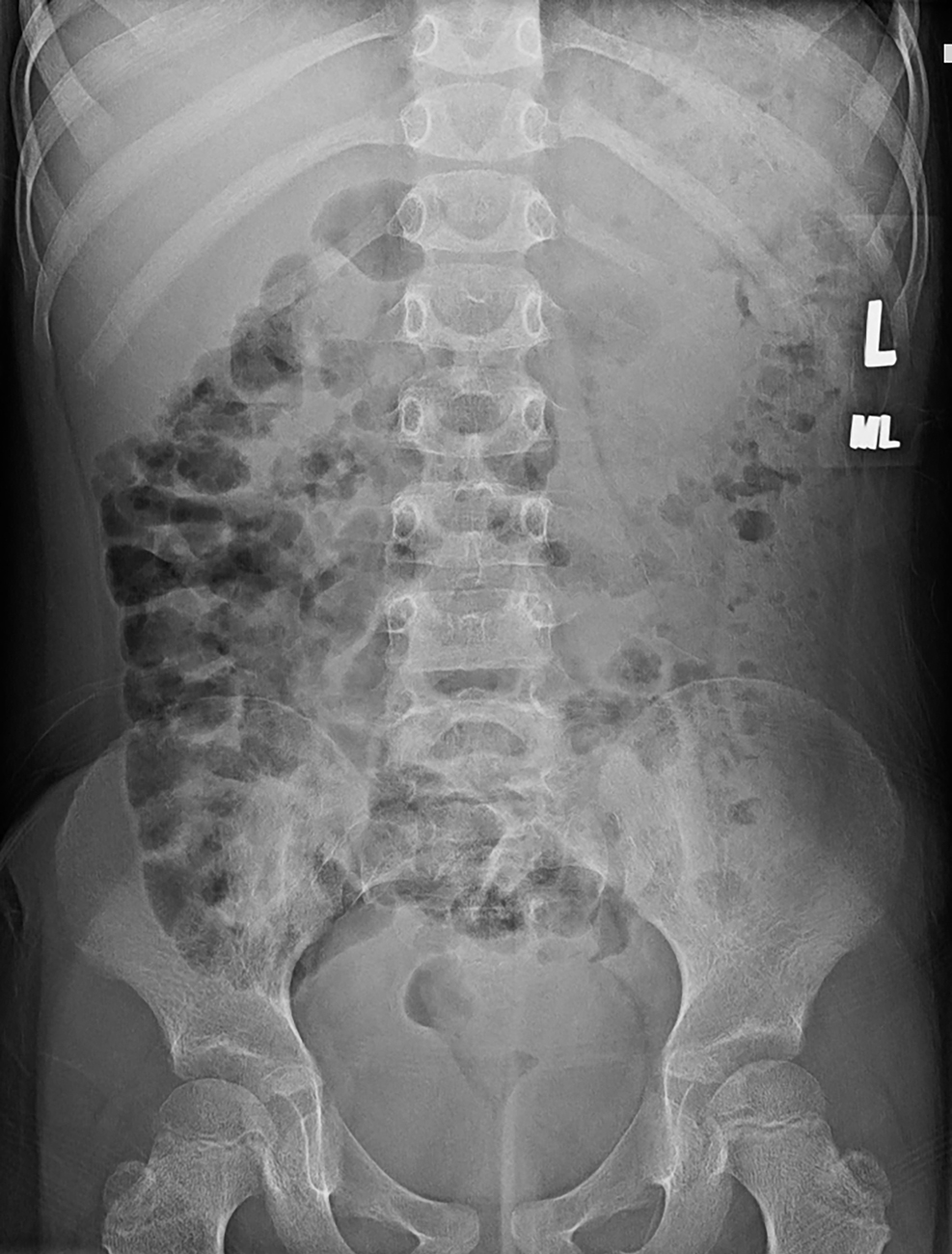
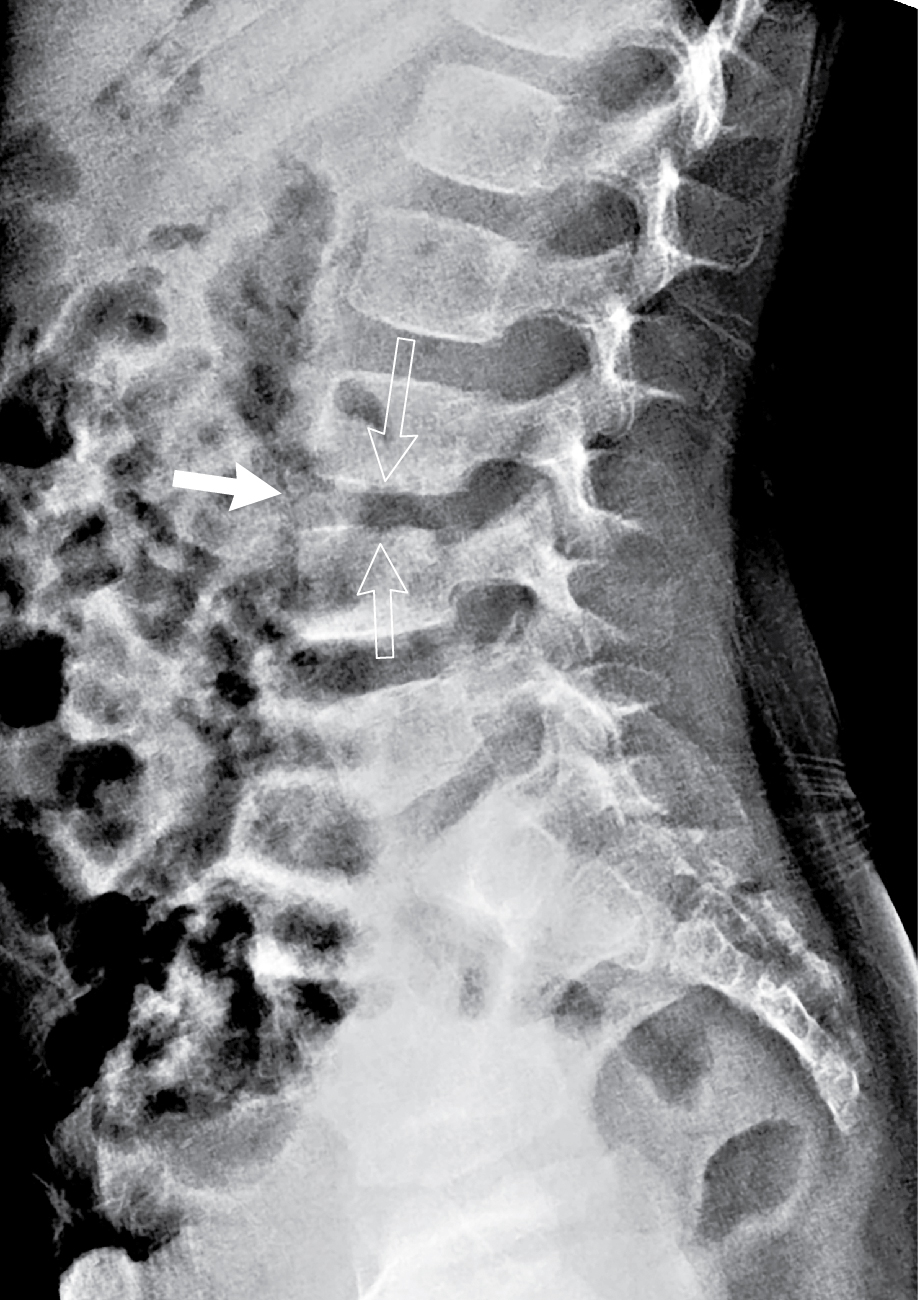
Imaging findings
The initial imaging studies obtained by the primary care physician were reviewed. These images are presented here: one view of the pelvis and two views of the lumbar spine ( Figs. 75.1–75.3 ). These images reveal no acute fracture or dislocation and normal bony alignment; however, there is subtle disc space narrowing at L3–4, better appreciated after the MRI examination is reviewed. There is a normal bowel gas pattern.


Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








