, Carlos Capuñay1, Carlos E. Sueldo2 and Juan Mariano Baronio3
(1)
Diagnóstico Maipú, Buenos Aires, Argentina
(2)
University of California, San Francisco, CA, USA
(3)
CEGYR, Buenos Aires, Argentina
The uterine silhouette is a settling place for different malformations and pathological processes, some of which can require surgical treatment, may it be via the abdomen (laparotomy, laparoscopy) or the vagina (hysteroscopy, laparoscopy) [1–3]. In certain opportunities one can also turn to endovascular treatment, as is the case of the chemoembolization of uterine myomas [4–6].
These procedures on the uterus can generate morphological changes that are visible in virtual hysterosalpingography (VHSG) studies. Different are the motives to carry out these therapeutic measures, among them is found the resection of myomas, the reparation of uterine anomalies, the removal of synechiae and the cesarean section [7, 8].
In this chapter the cases related to diverse therapeutic procedures their sequels and/or complications will be shown.
Myomas
The uterine myomatosis is a frequent entity in women older than 30 [9, 10]. The myomas can be intramural, submucosal and subserous. Their relation with fertility is controversial, with different opinions on when and in what level do the myomas influence in the success of the pregnancy [11–15].
Different are also the therapeutic strategies, depending on the number, size, maternity wishes and age of the patient. Submucosal myomas can be dried with hysteroscopy; subserosal or intramural myomas removed through laparotomy or preferably through laparoscopic surgery [1, 2, 16, 17]. The surgical drying of these tumors can generate significant changes in the morphology of the uterus according to the size, location and number of removed myomas. In the case of small intramural or subserous fibroids, the uterine cavity does not generally present any changes. However, the removal of submucosal or intramural myomas of larger size can deform the cavity after the myomectomy [7, 8].
Currently, another therapeutic option that has earned a place amid the different variants of available treatments is the chemoembolization [4–6]. This procedure provides also changes at the level of the uterus and/or of the cavity that can be appreciated in imaging studies.
Case 1
A 34-year old patient, G0P0, with primary infertility. The VHSG shows the presence of a subserous myoma on the left lateral and anterior wall of 5 × 5.5 × 8 cm that deforms the uterine silhouette, and a uterine cavity of normal morphology and regular outlines (Fig. 10.1). Its surgical removal is decided prior the start of the infertility treatment. The control VHSG carried out 2 months after the surgery shows a uterus of conservative size and normal morphology (Fig. 10.2).
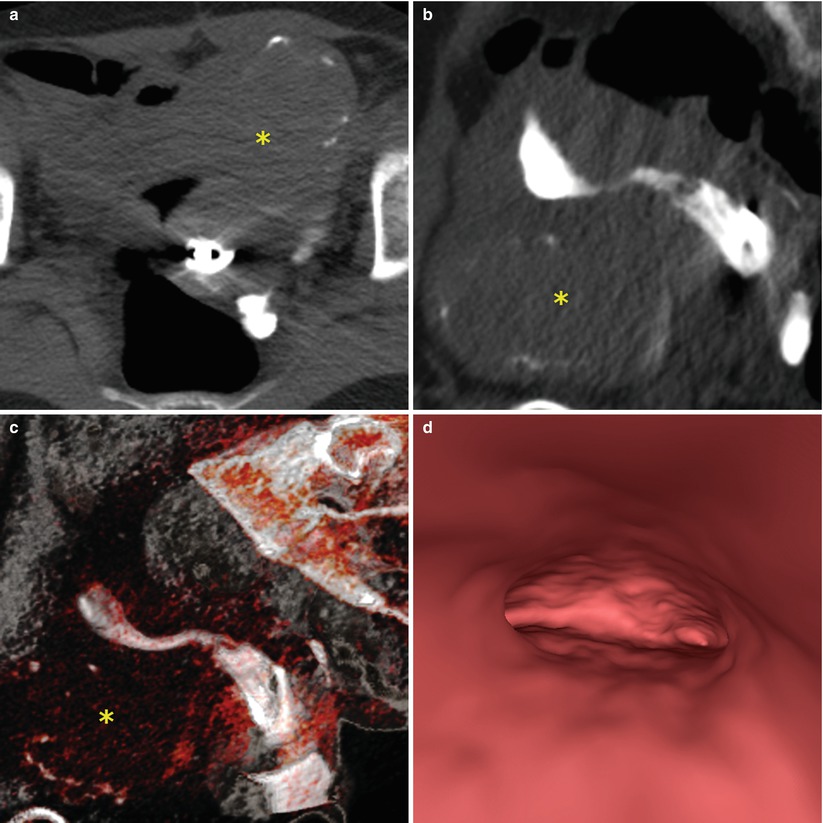
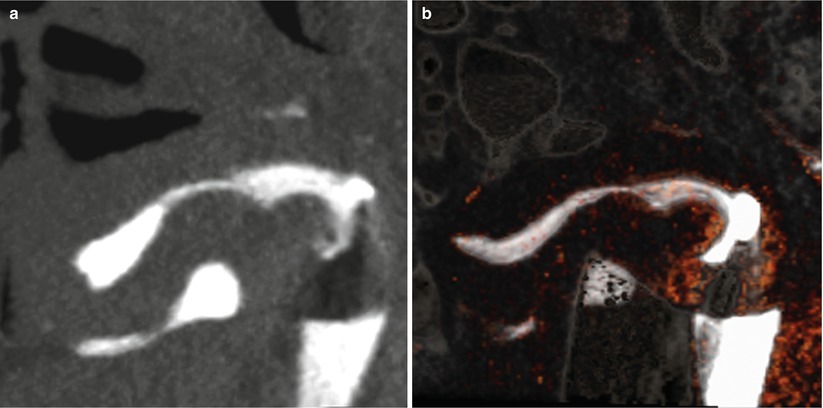
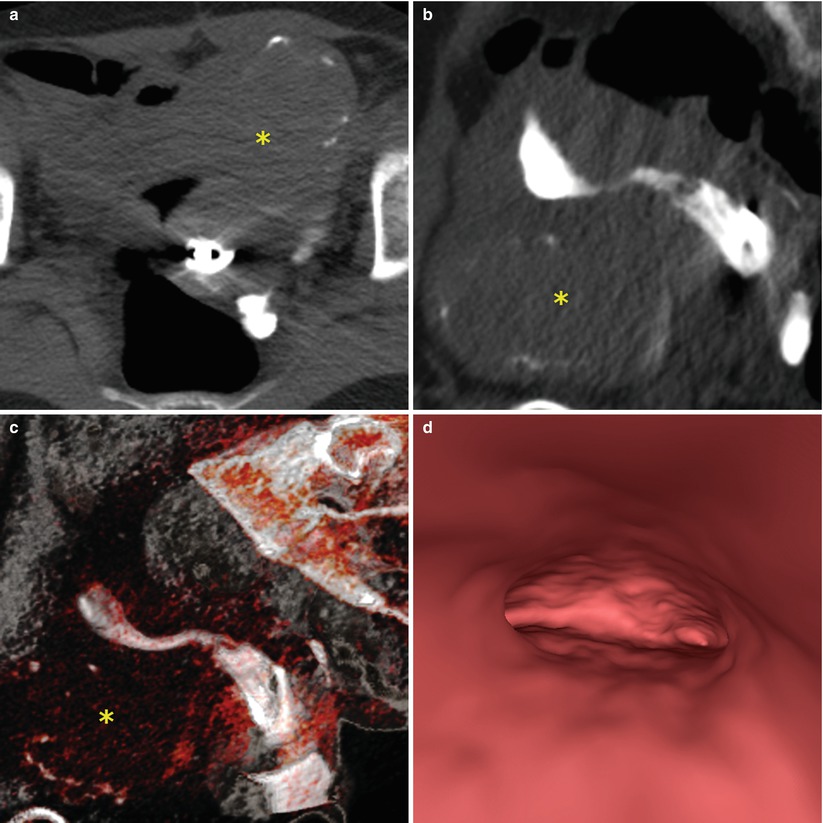
Fig. 10.1
VHSG study showing an anteverted uterus increased in size with the presence of an anterior subserosal myoma, with fine peripheral calcifications (asterisk). (a) Axial maximum intensity projection (MIP) image. (b) Sagittal MIP image. (c) Sagittal 3D volume rendering image. (d) Virtual endoscopy image showing a normal endometrial cavity
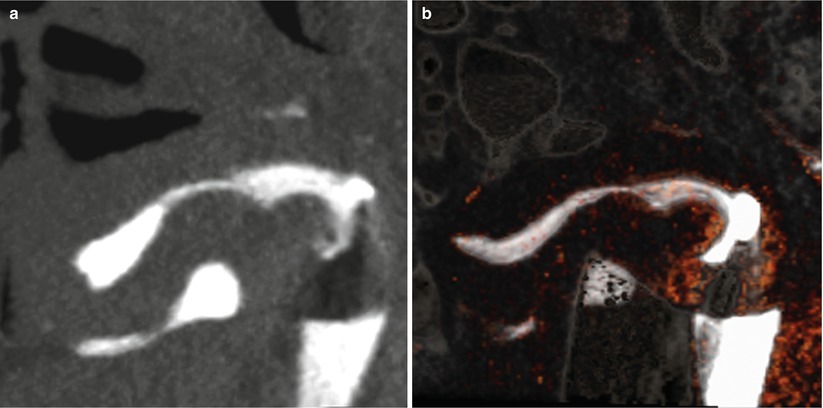
Fig. 10.2
Post-surgery VHSG study showing an anteverted uterus of normal size. (a) Sagittal maximum intensity projection image. (b) Sagittal 3D volume rendering image
Case 2
A 29-year old patient, G1P1, with secondary infertility of 18 months. The VHSG exam shows a deformity in the uterine cavity at the level of the fundus, on the right horn, secondary to the presence of a posterior submucosal myoma of medium size (Fig. 10.3). Given these characteristics, and its potential influence in the success of the conception, it is proceeded with its removal via hysteroscopy (Fig. 10.4). The control VHSG after 3 months shows a uterine cavity of normal morphology with regular outlines, with no evidence of postsurgical sequels (Fig. 10.5).
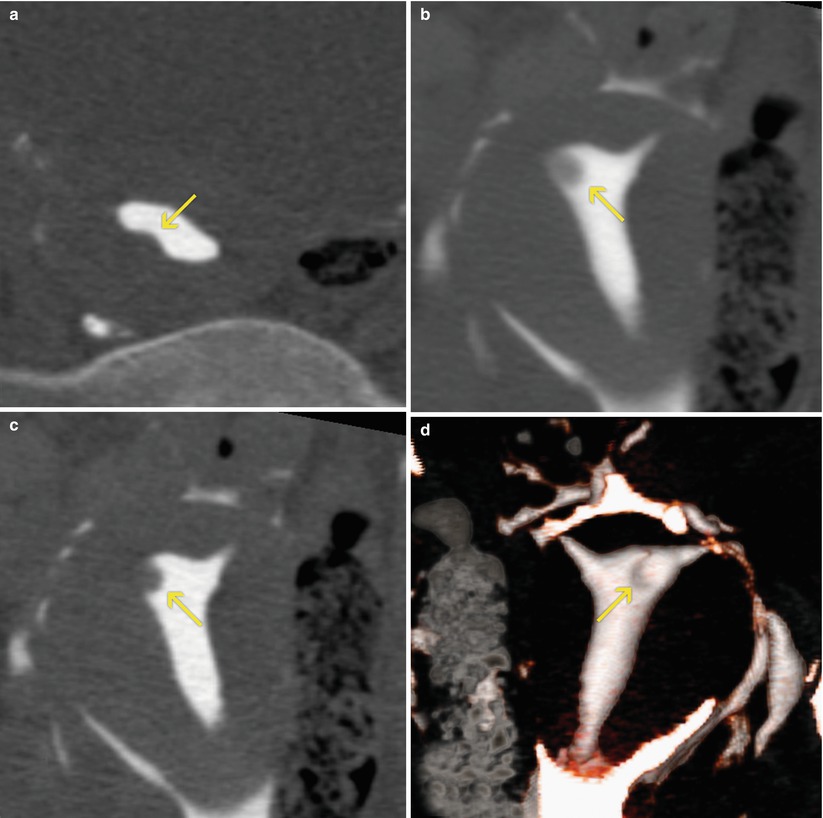
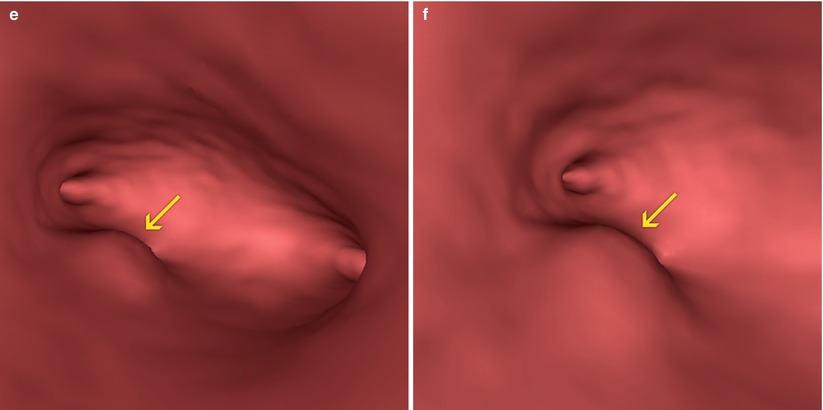
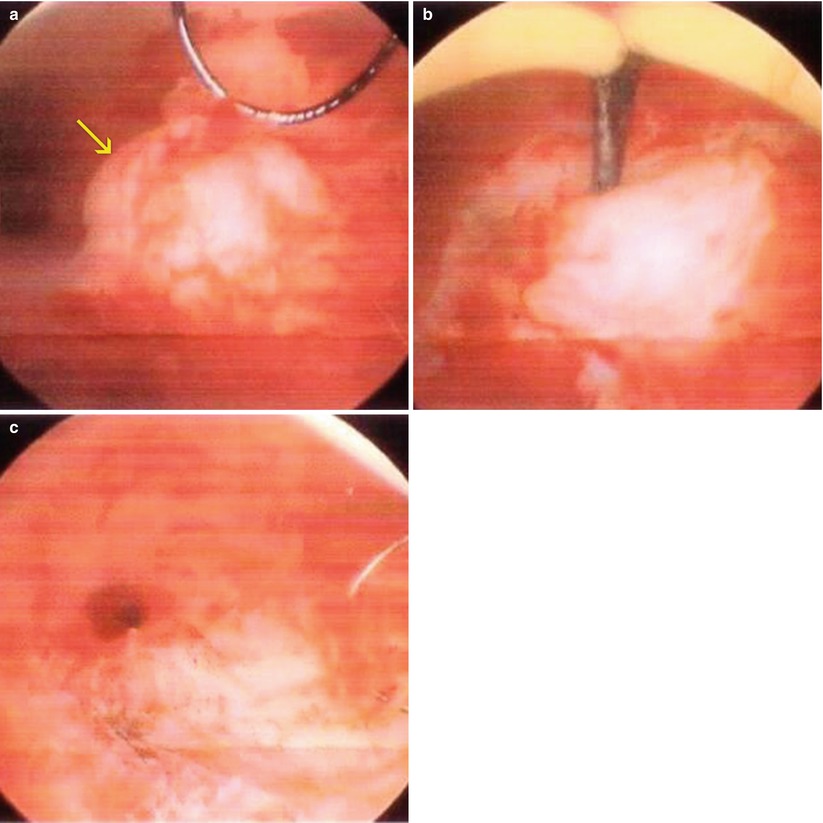
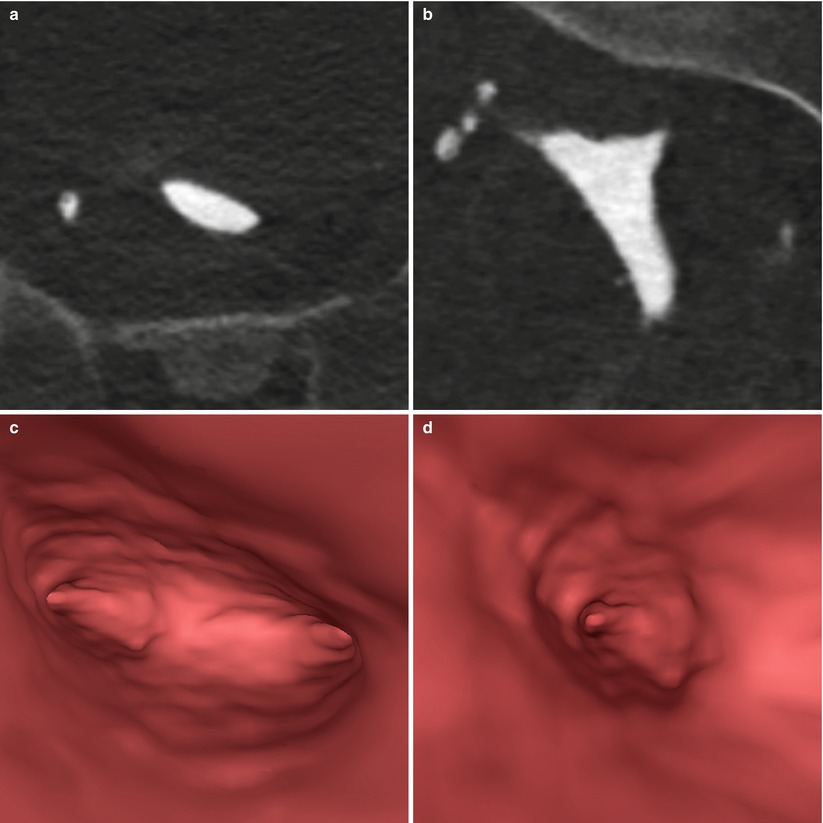
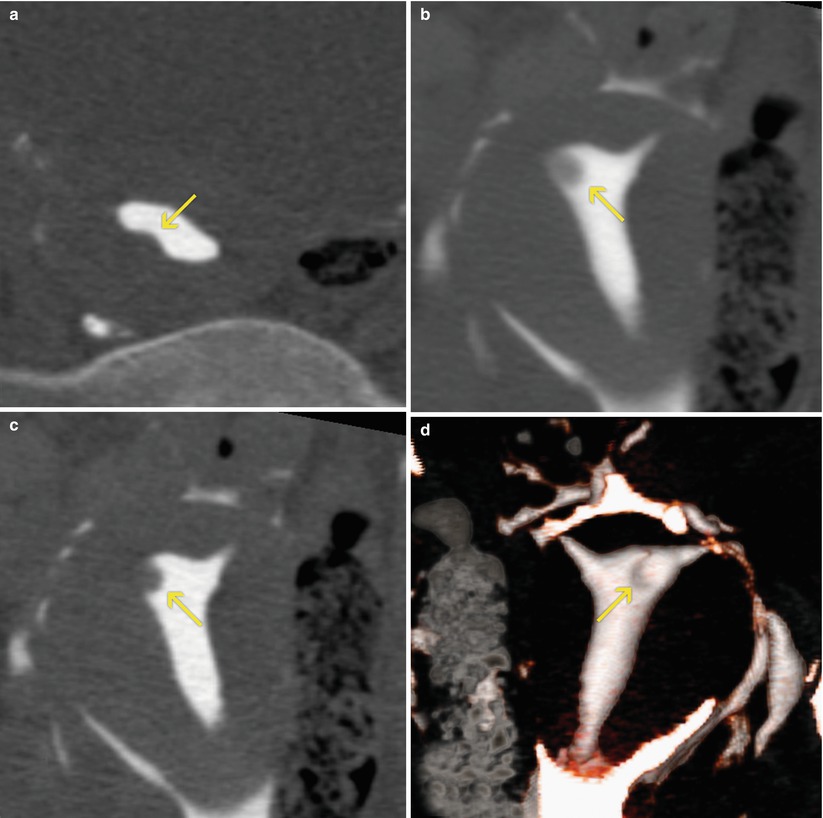
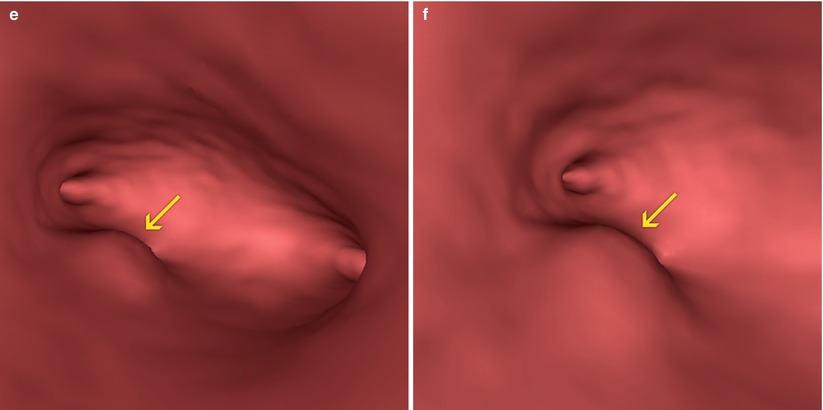
Fig. 10.3
VHSG study which shows an elevated image on the posterior wall of the uterus that protrudes into the endometrial cavity compatible with a submucosal myoma (arrows). (a) Axial maximum intensity projection (MIP) image. (b) 5-mm coronal multiplanar reconstruction image. (c) Coronal MIP image. (d) Coronal 3D volume rendering image, posterior view. (e, f) Virtual endoscopy images
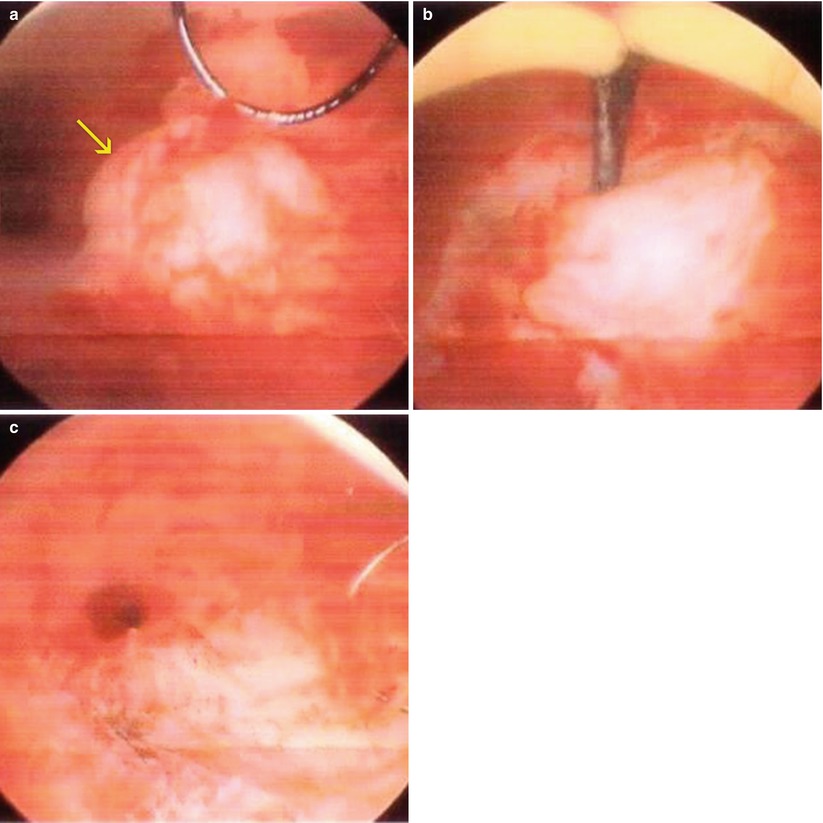
Fig. 10.4
Conventional hysteroscopy images. (a) Submucosal myoma on the posterior wall of the uterine cavity (arrow). (b) Myomectomy. (c) Post-surgical sequelae
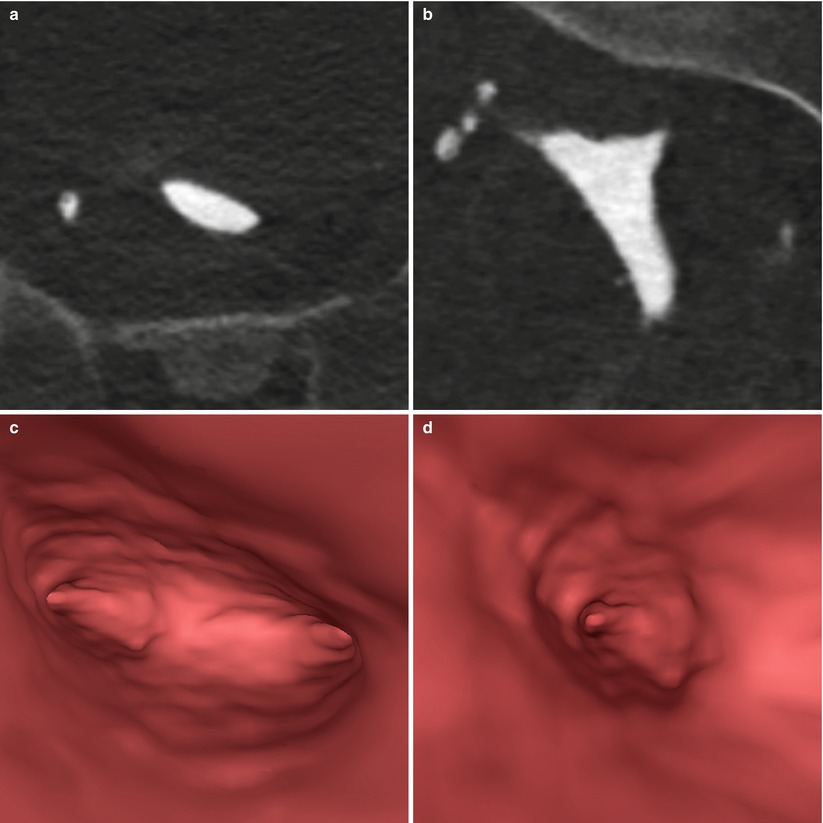
Fig. 10.5
Post-myomectomy VHSG study. An endometrial cavity without endoluminal lesion is observed. (a) Axial maximum intensity projection (MIP) image. (b) Coronal MIP image. (c, d) Virtual endoscopy images
Case 3
A 36-year old patient, G0P0, with primary infertility and multiple symptomatic uterine myomatosis of 7 years of evolution. The presence of an intramural myoma on the right lateral uterine wall of 44 × 42 × 41 mm stands out, with an approximate volume of 39 cm3 (Fig. 10.6). The patient carried out medical treatment with agonists of the GnRh for 6 months, previous to the uterine embolization treatment, taking part of an immediate post-procedure without complications. A year later she returns for a reevaluation for her primary infertility. A control transvaginal ecography is done, identifying iso-hipoecogenic areas on the right myometrial wall in the location of the treated myoma, with thickening and endometrial liquid. Upon the 10th day, a conventional X-ray hysterosalpingography is done that shows passage of the instilled contrast through the external cervical os towards a pseudocavity located on the right uterine wall (Fig. 10.7). The exam is completed with the realization of a VHSG to value with higher precision the state of the endometrial cavity and plan the next procedure of assisted fertilization. The study shows the presence of fistula between the endometrial cavity and the residual post-embolization cavity, allowing the clear visualization of the diameter and length of the fistula trajectory, the parietal thickness of the residual pseudocavity and the absence of perforation towards the peritoneal cavity (Fig. 10.8).
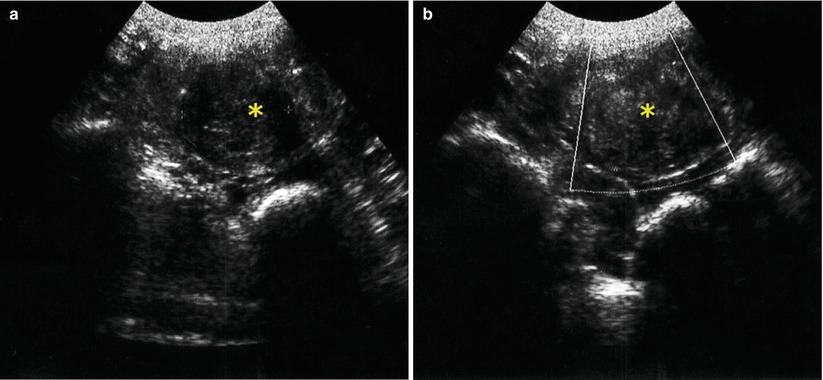
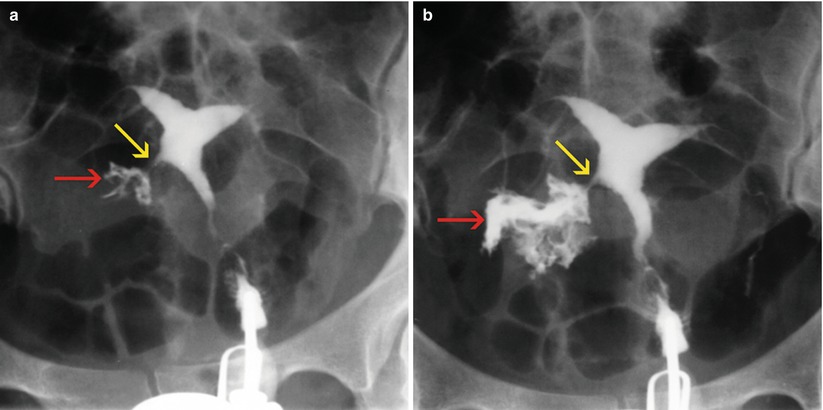
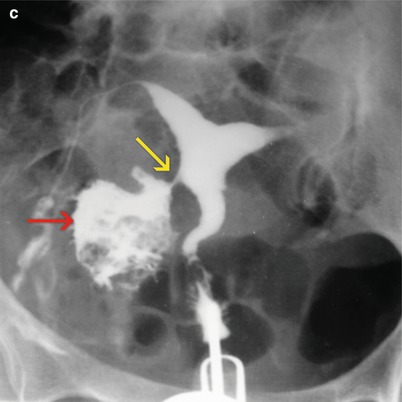
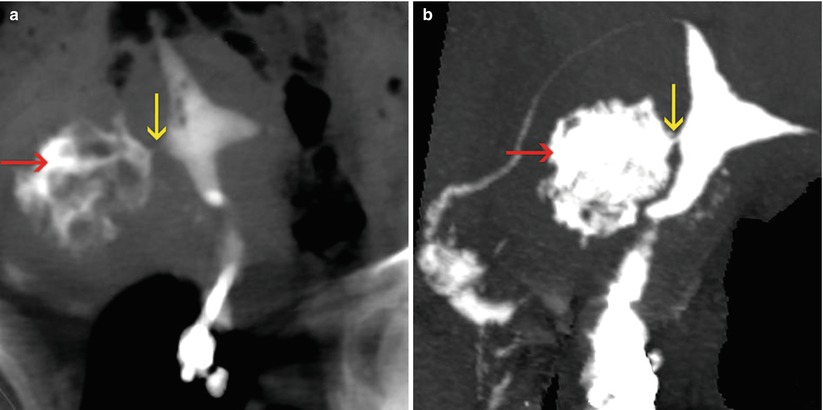
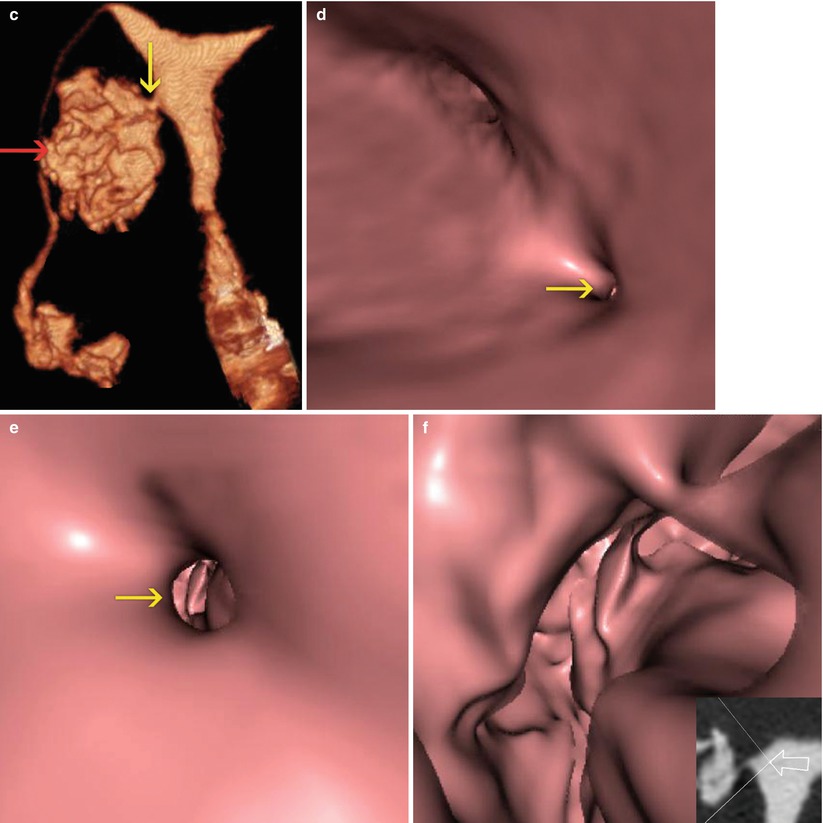
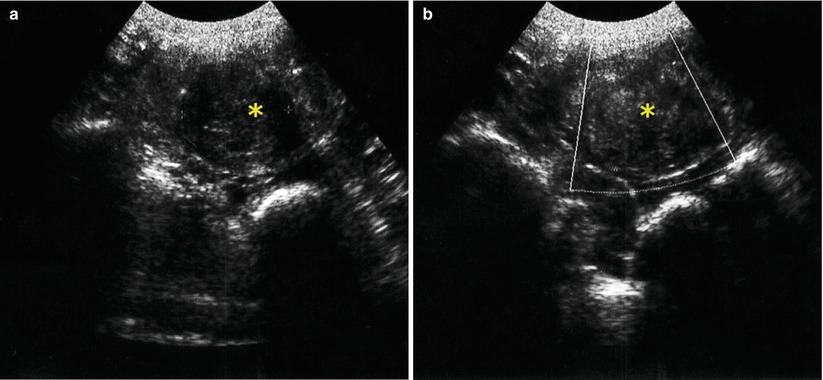
Fig. 10.6
Transvaginal ultrasound. Presence of intramural myoma on the right lateral uterine wall, of 44 × 42 × 41 mm in size, with a volume of 39 cm3 (asterisk). (a) Transverse image (b) Transverse image with Doppler
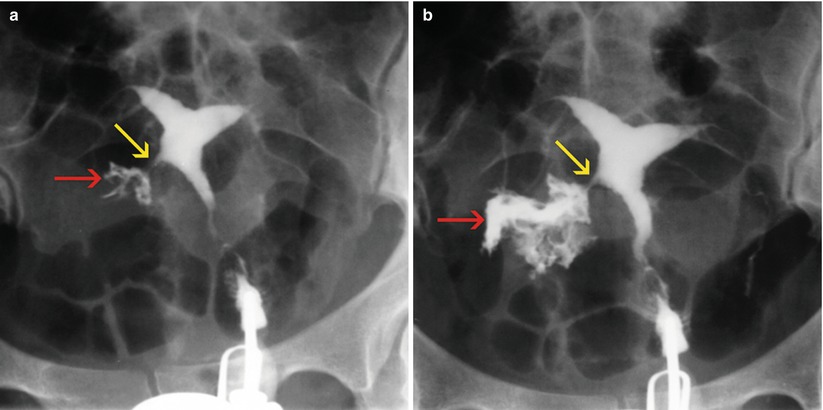
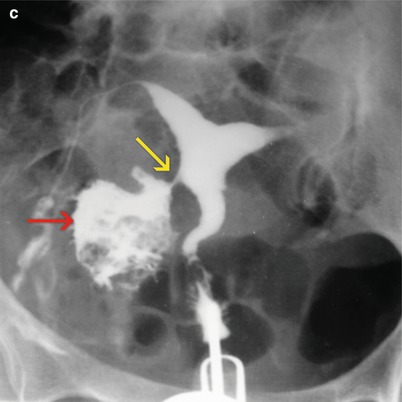
Fig. 10.7
(a–c) HSG images post embolization treatment. A progressive filling of an irregular cavity is appreciated on the right uterine wall (red arrows). The presence of a fistulous tract (yellow arrows) between the endometrial cavity and the uterine wall cavity is demonstrated
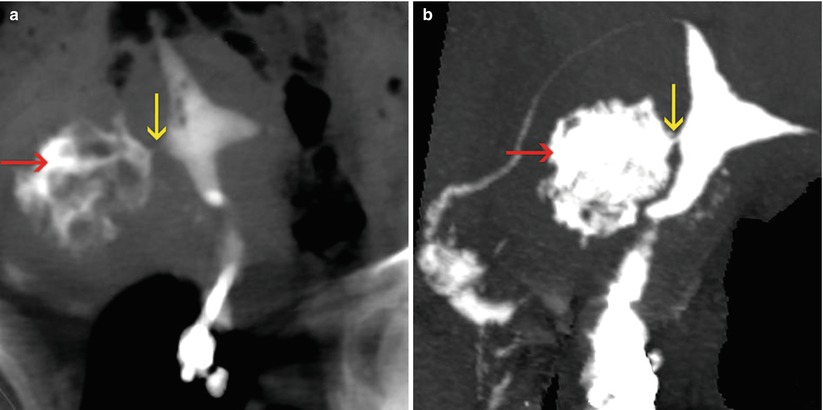
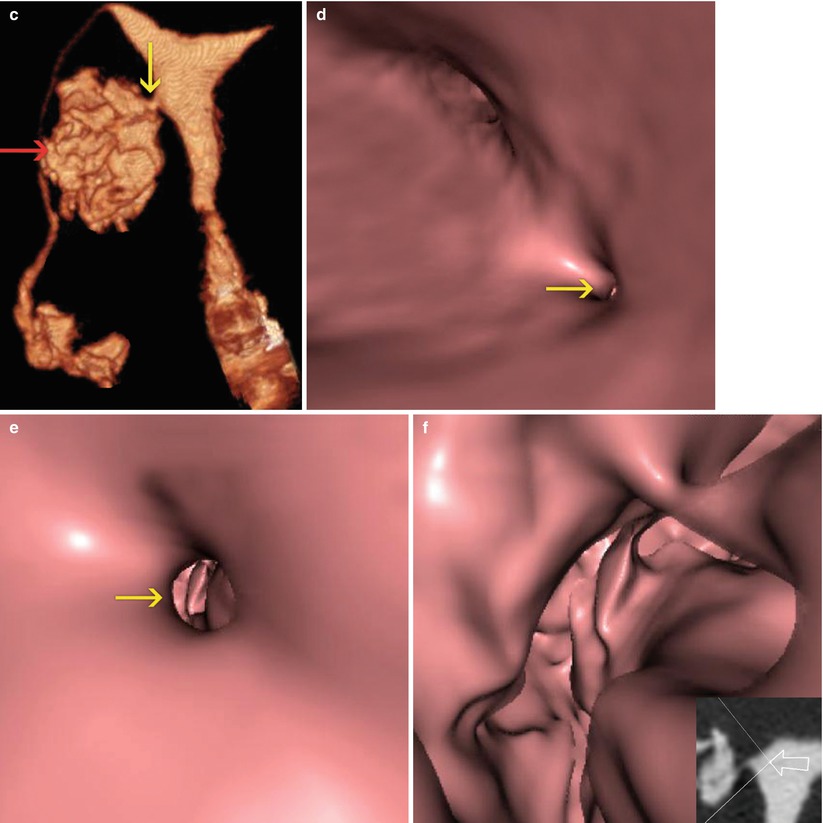
Fig. 10.8
VHSG study post embolization treatment. A progressive filling of an irregular cavity is appreciated on the right uterine wall (red arrows), with the presence of a fistulous tract to the endometrial cavity (yellow arrows). (a) 5-mm coronal multiplanar reconstruction image. (b) Coronal maximum intensity projection image. (c) Coronal 3D volume rendering image. (d) Virtual endoscopy image which shows the orifice of the fistula in the right wall of the endometrial cavity. (e) Virtual endoscopy image at the level of the fistulous tract. (f) Virtual endoscopy image of the residual post-embolization cavity on the right uterine wall
Uterine Malformations
The plastic and reconstructive uterus operations in patients with uterine anomalies, whether it is a septated or bicornuate uterus, are an alternative for those women who want to achieve a successful pregnancy [3, 13]. In patients with a septated uterus, the removal of the uterine septum via hysteroscopy is a surgical technique of growing application in the treatment of this uterine anomaly. Among the complications of this technique, an incomplete removal of the uterine septum and the formation of adherences or intrauterine synechiae are included [18, 19].
Case 4
A 24-year old patient, G3P0A3, with a history of spontaneous abortions during the first trimester. A diagnosis of a partial septated uterus is done (Fig. 10.9). As a therapeutic strategy, the removal via hysteroscopy of the uterine septum is decided. The VHSG study post-treatment shows a more ample uterine cavity, with a small indentation at the level of the fundus corresponding to the normal postsurgical remnant (Fig. 10.10).
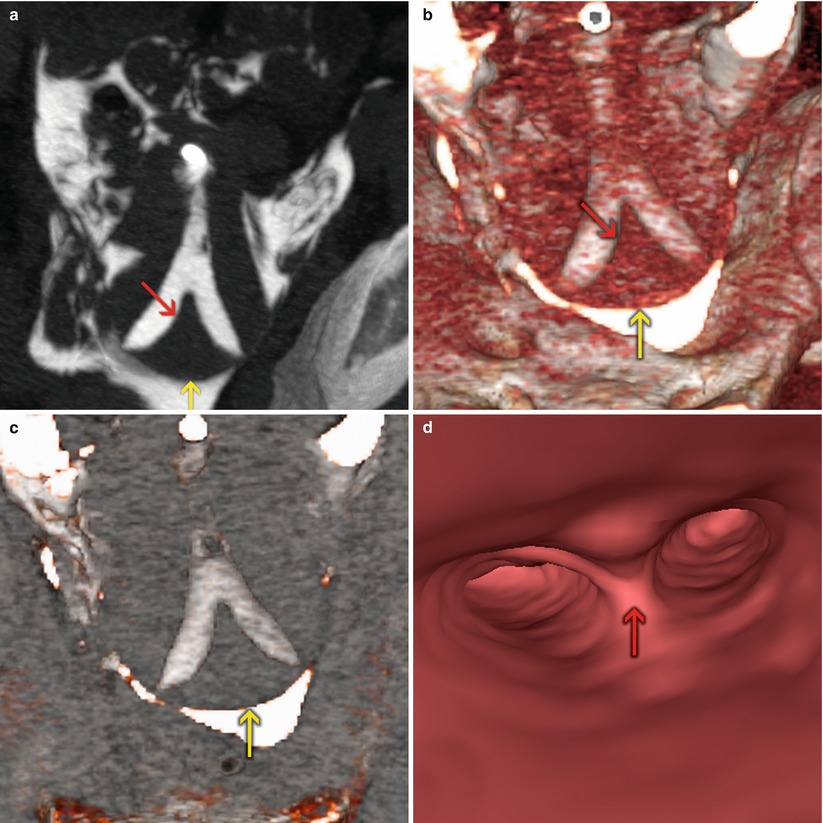
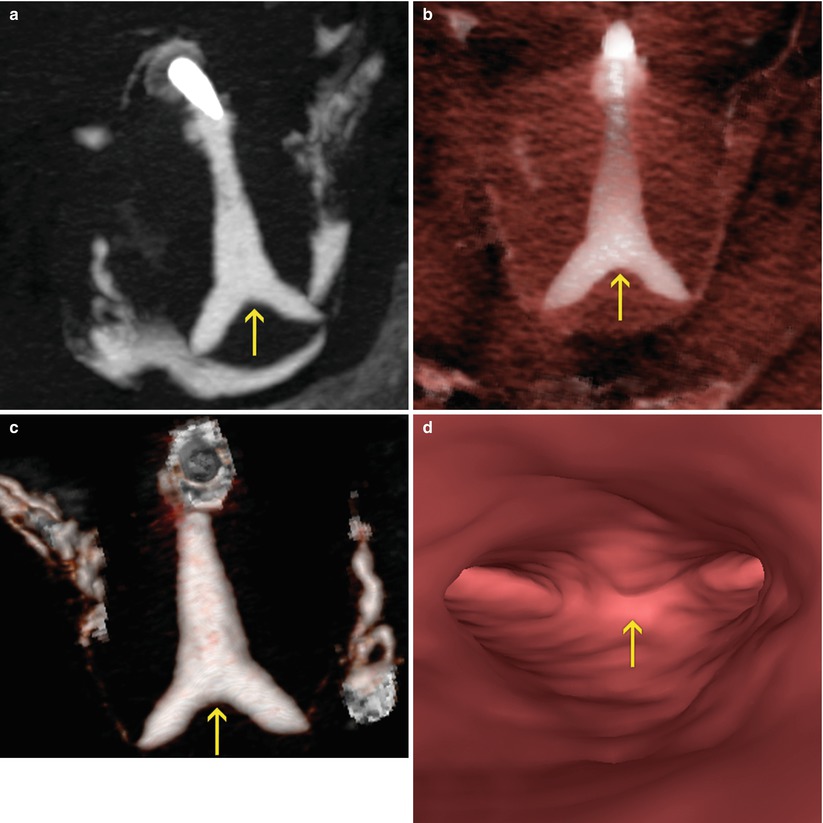
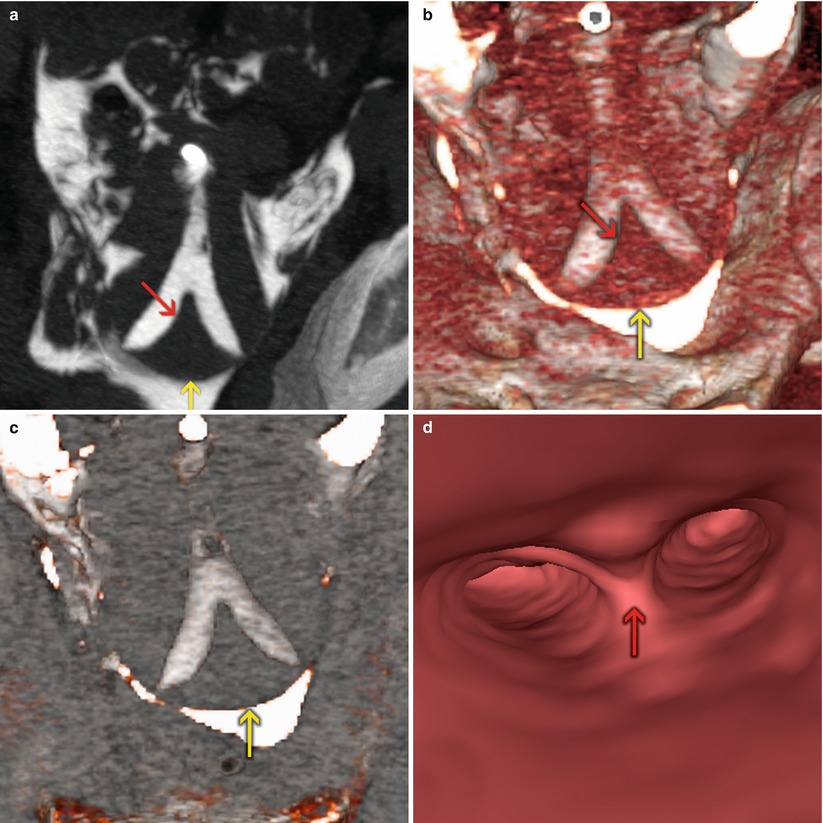
Fig. 10.9
VHSG study showing a partial septate retroverted uterus. A normal external configuration of the uterus is appreciated (yellow arrows) as well as the septum which divides the endometrial cavity (red arrows). (a) Coronal maximum intensity projection image. (b, c) Coronal 3D volume rendering images. (d) Virtual endoscopy image
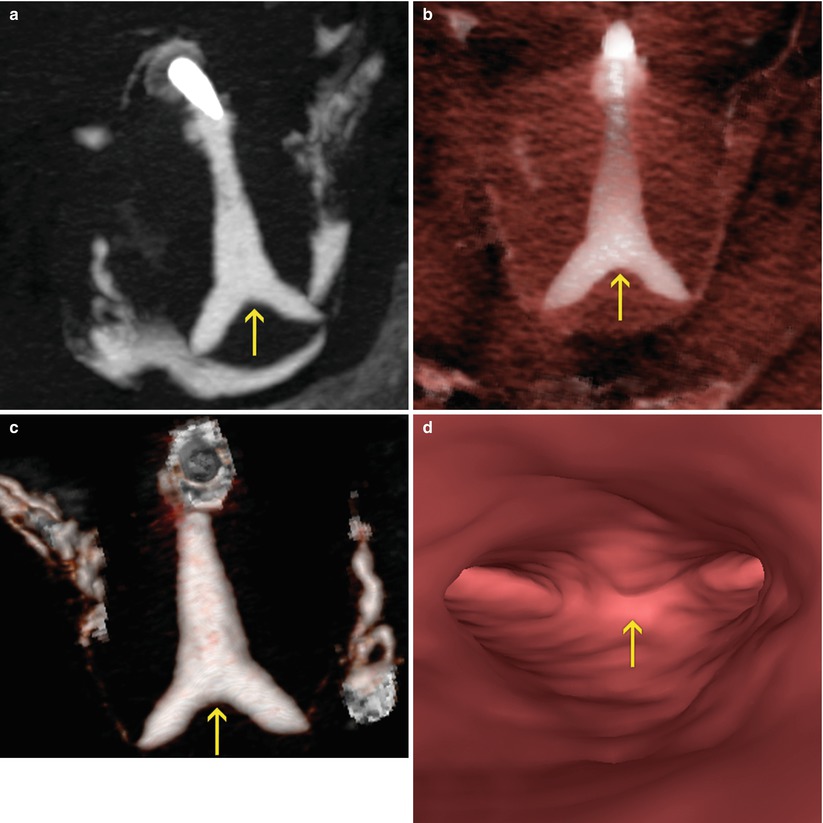
Fig. 10.10
Control VHSG study after the hysteroscopy treatment. The removal of the uterine septum and the presence of a small indentation at the level of the fundus, which corresponds to the normal post-surgical septum remnant can be appreciated (arrows). (a) Coronal maximum intensity projection image. (b, c) Coronal 3D volume rendering images. (d) Virtual endoscopy image
Case 5
A 25-year old patient, G2P0A2, with diagnosis of bicornuate uterus (Fig. 10.11). The patient is subject to a Strassman surgery as the reparation technique. In the post-treatment VHSG study carried out on the third month, a larger endometrial cavity could be appreciated, with a slight deformity at the level of the fundus, of regular margins and with no filling defects (Fig. 10.12).
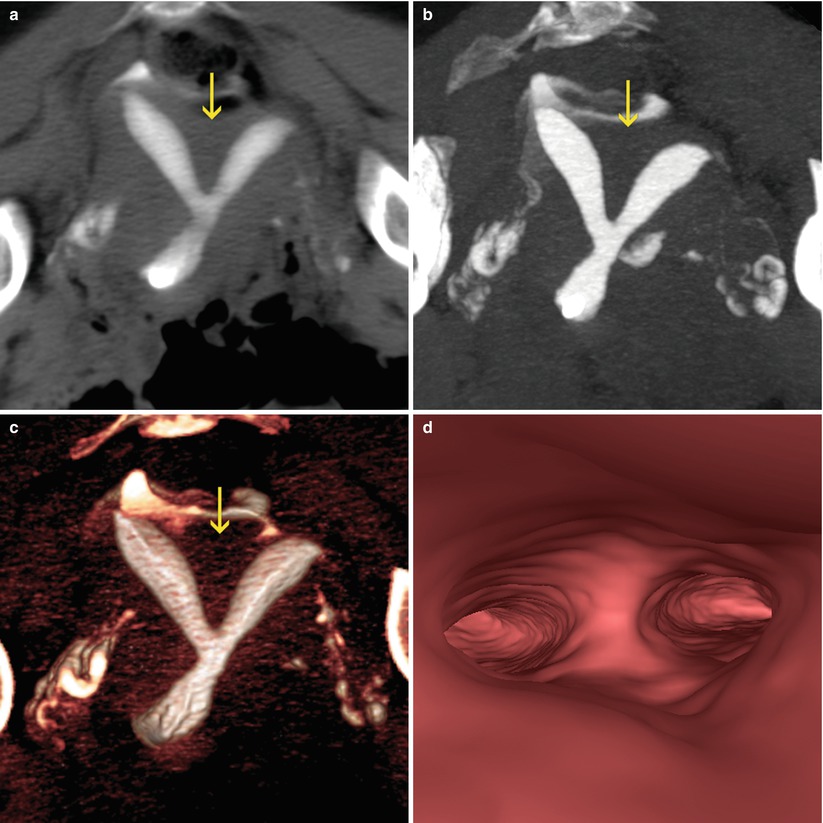
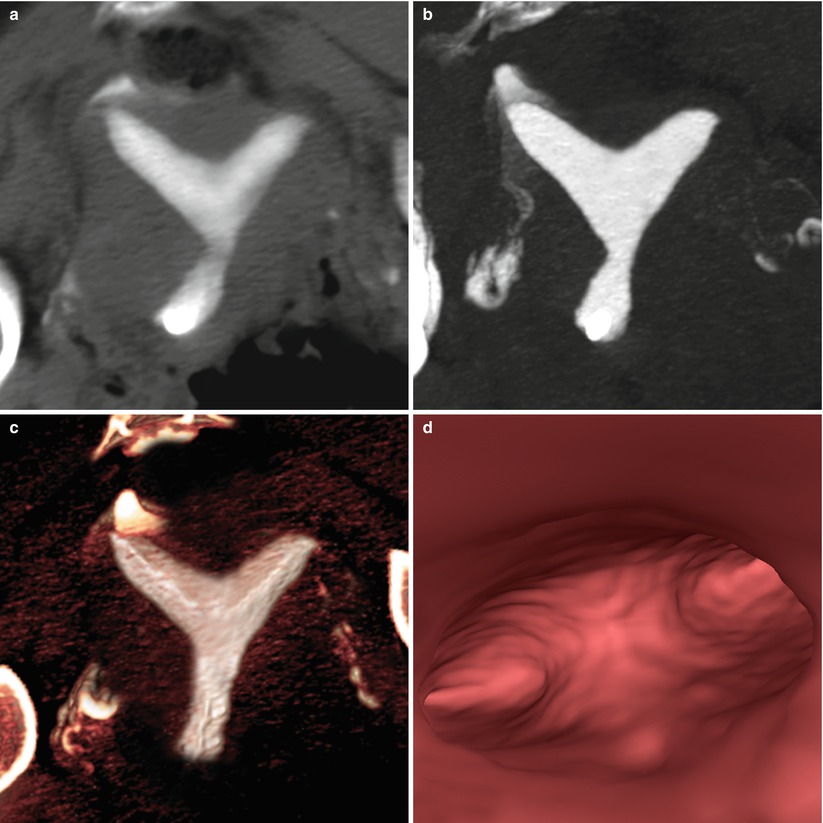
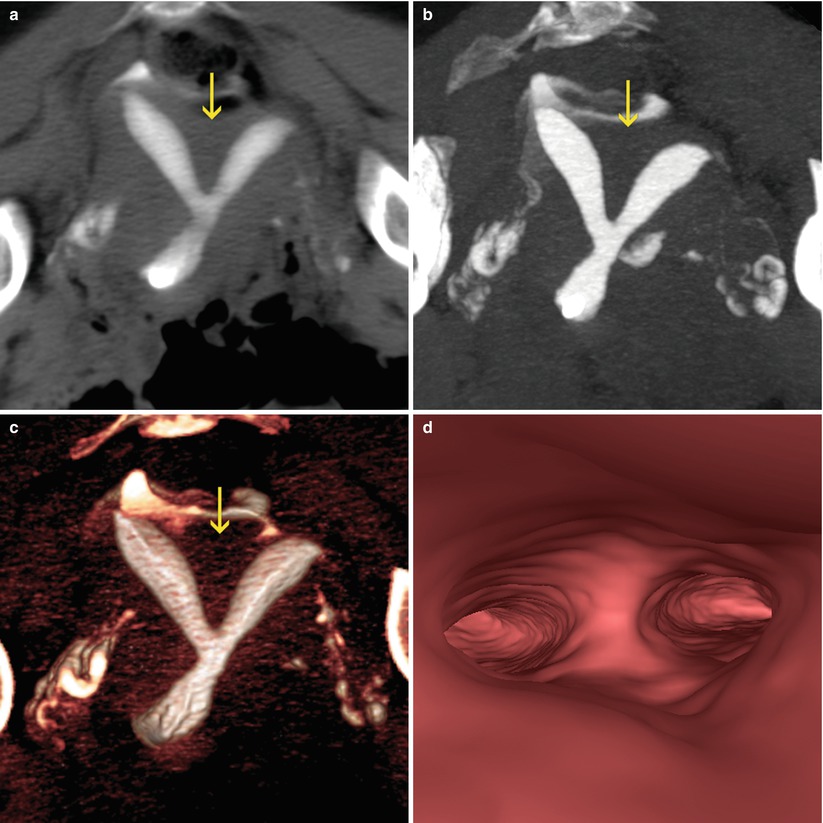
Fig. 10.11
VHSG study showing a retroverted bicornuate uterus. The concave external configuration (arrows) and the divergence of the uterine horns can be appreciated. (a) 5-mm coronal multiplanar reconstruction image. (b) Coronal maximum intensity projection image. (c) Coronal 3D volume rendering image. (d) Virtual endoscopy image
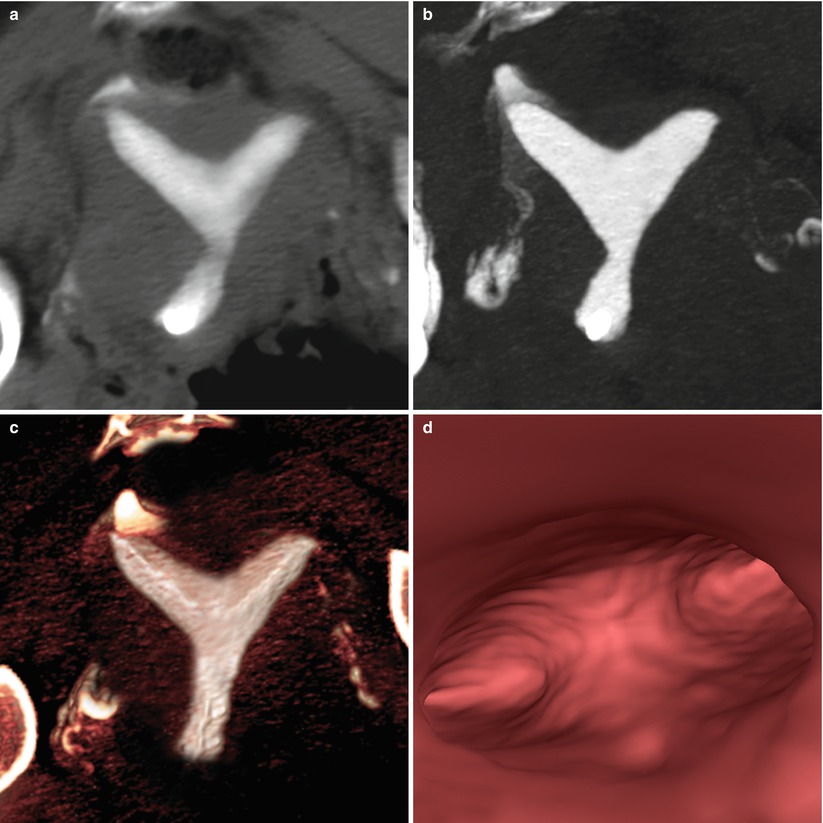
Fig. 10.12
Control VHSG study after uterine repair of a bicornuate uterus. A broader endometrial cavity can be appreciated. (a) 5-mm coronal multiplanar reconstruction image. (b) Coronal maximum intensity projection image. (c) Coronal 3D volume rendering image. (d) Virtual endoscopy image
Synechiae
The intrauterine adherences represent scars in the uterine cavity result of an infection or trauma. The removal via hysteroscopy is today the most utilized procedure and considered of reference for the diagnosis and treatment [20, 21]. The most secure, less traumatic and most precise technique consists in the adhesiolisis, through the combination of surgical dissection and electrosurgery, and the postsurgical administration of high doses of estrogens, and/or progestogens and antibiotics, important in the prevention of the recurrence. The use of intrauterine contraceptive devices after the resection of the synechiae is considered useful by some groups, while other propose the use of hyaluronic acid as an alternative [22–24].
Case 6
A 29-year old patient, G2P0A2, with secondary infertility of 3 years of evolution, and a history of abortions with uterine curettage. As part of the diagnostic algorithm, the patient carries out a VHSG that demonstrates the presence of an irregular endometrial cavity, with lineal, irregular and thick filling defects that correspond to synechiae. The presence of a subserous myoma is also appreciated (Fig. 10.13). Treatment consists in the hysteroscopic removal of the synechiae and the laparoscopic resection of the myoma. The VHSG control carried out after 3 months shows the incomplete removal of the adherences, with a residual synechia around the right uterine horn. The subserosal myoma cannot be appreciated (Fig. 10.14).
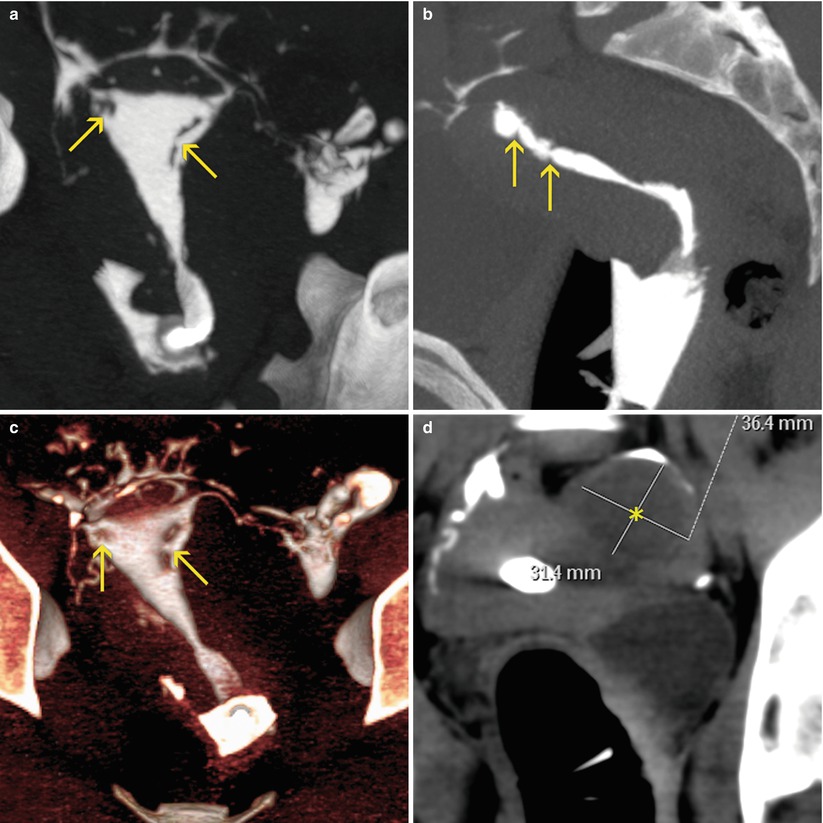
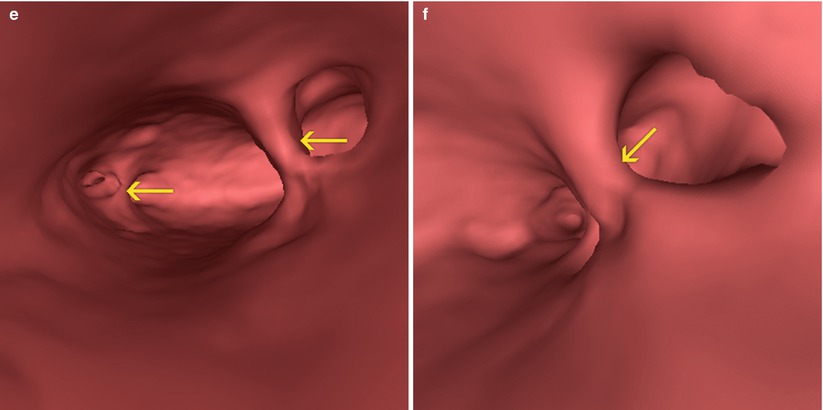
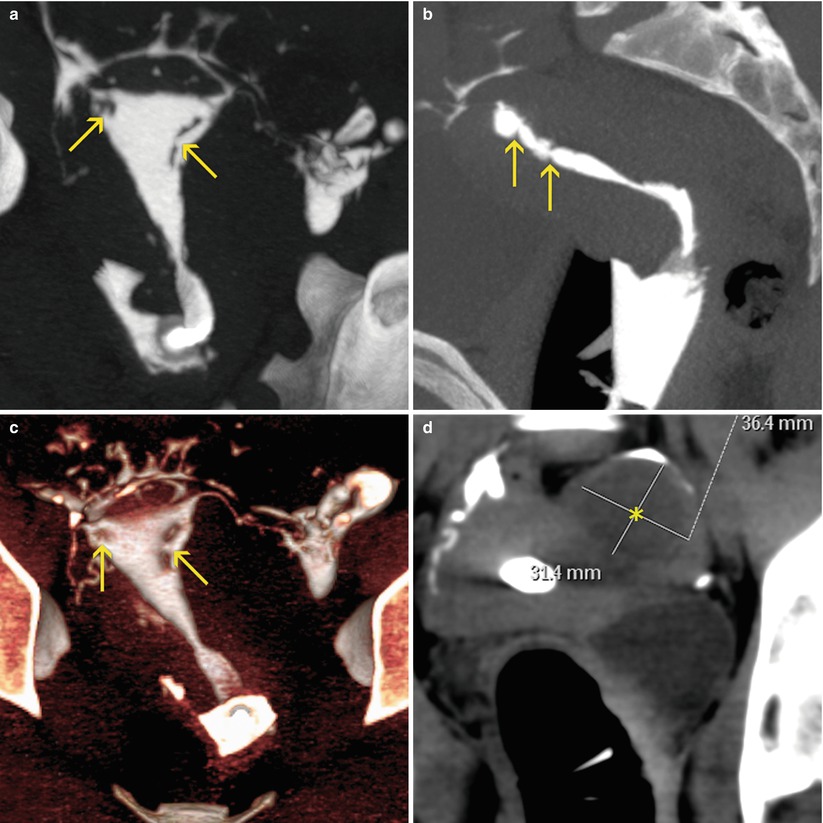
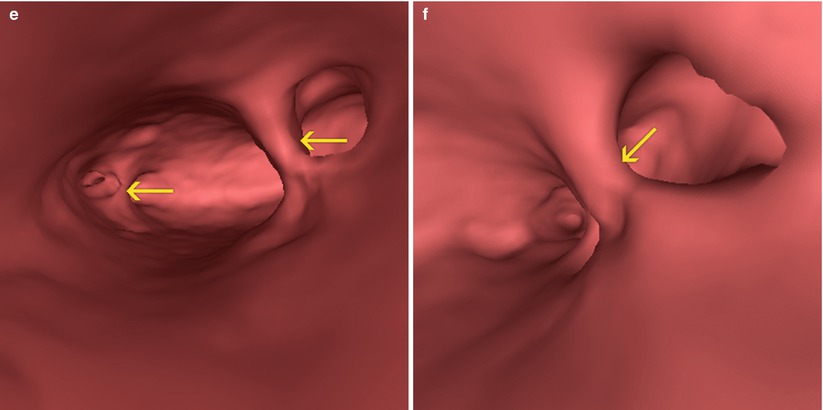
Fig. 10.13




VHSG study showing the presence uterine synechiae (arrows). A subserosal myoma on the left lateral wall can also be appreciated (asterisk). (a) Coronal maximum intensity projection (MIP) image. (b) Sagittal MIP image. (c) Coronal 3D volume rendering image. (d) Axial MIP image. (e, f) Virtual endoscopy images
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree