, Carlos Capuñay1, Carlos E. Sueldo2 and Juan Mariano Baronio3
(1)
Diagnóstico Maipú, Buenos Aires, Argentina
(2)
University of California, San Francisco, CA, USA
(3)
CEGYR, Buenos Aires, Argentina
In each virtual hysterosalpingography (VHSG) study there is a potential risk of carrying out an incorrect diagnosis. The VHSG has shown sensibility and specificity results similar to those of the conventional hysterosalpingography study [1, 2]. Nevertheless, a great number of false interpretations can affect the general validity of the method; the most efficient strategy to prevent the pitfalls is to appropriately solve the diagnostic errors which arise from false positives and negatives.
Anyhow, a considerable number of false diagnoses can be prevented, but not all of them. The perform of the diagnostic studies with an adequate preparation and an appropriate technical procedure is important for limiting the factors which entail errors [3]. It is also essential that the radiologist be familiarized with the spectrum of normal and pathological findings for a correct interpretation of the VHSG exams.
On occasions the false interpretations imply some clinical significance [4]. The false positive diagnosis is a perceptive error which occurs when a lesion is detected where in fact no such abnormality exists [5]. In the VHSG studies, in general, it occurs when elevated images of the uterine cavity exist which may suggest polipoid lesions or when, in the lack of opacification of the uterine tubes, they are interpreted as being obstructed. One false positive finding can lead to the execution of an unnecessary complementary study, with the added preoccupations, associated costs and risks that this entails. Even a wrong diagnosis can determine a change in the therapeutic conduct. Furthermore, false positives affect the specificity and positive predictive value when the validity of the method is evaluated [6].
A false negative diagnosis is an error that occurs when a lesion that in reality exists is not able to be identified. The experience of these false interpretations was acquired with research protocols along the years in our institution for the validation of the method. When one is aware of the existence of these potential errors, and applies the solutions to avoid them, they rarely occur [7]. A VHSG study in optimal technical conditions is considered an exam with few false negatives and, therefore, with a high negative predictive value. This way, the validity of the study also considerably depends on the occurrence of false negatives.
False Positives
Seudopolyps
In VHSG studies, elevated lesions can be characterized correctly in most of the cases. Even the detection of small lesions is possible thanks to the larger spacial resolution of studies performed with multislice tomography [8]. However, a variety of findings that can simulate polyps exist. To help minimize this situation, it is fundamental to implement a rigorous preparation and a standardized procedure. One of the frequent causes of errors is the persistence of endoluminal mucosa secretions (Fig. 12.1). They usually present themselves as free linear structures with one extremity leaning on the endometrial surface. In other occasions, they are well adhered to the wall and acquire a rounded aspect, simulating real sessile polyps (Fig. 12.2). To avoid the presence of residual secretions it is recommended to always perform the studies once finished the menstrual period. Also, in the event of diagnostic doubt, a second acquisition of images can be obtained, where the mucosa secretion usually modifies their position and morphology with respect to the first acquisition (Fig. 12.3), while, on the other hand, a polyp remains fixed and with the same shape it was before. The linear secretions can also be confused with synechiae when they are firmly adhered to the uterine wall on both extremes. In these cases, history of invasive procedures and gynecologic infectious processes, as well as the fibrous and irregular appearance of adhesions help perform the differential diagnosis.
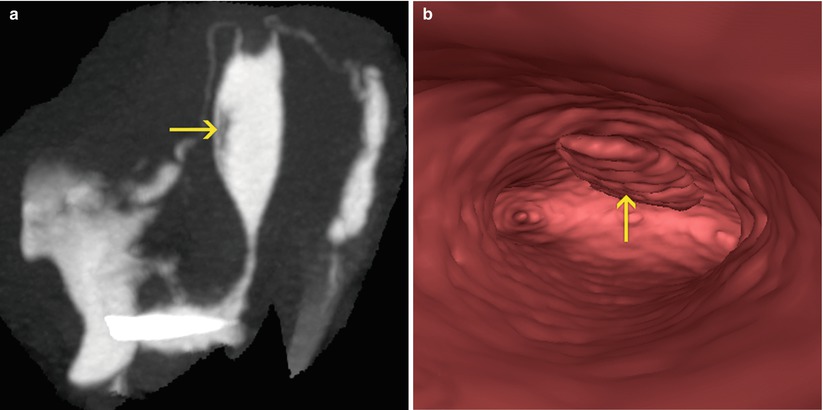
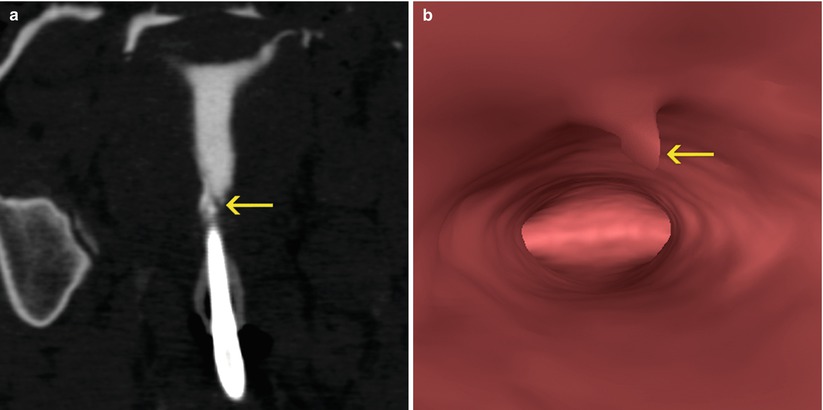
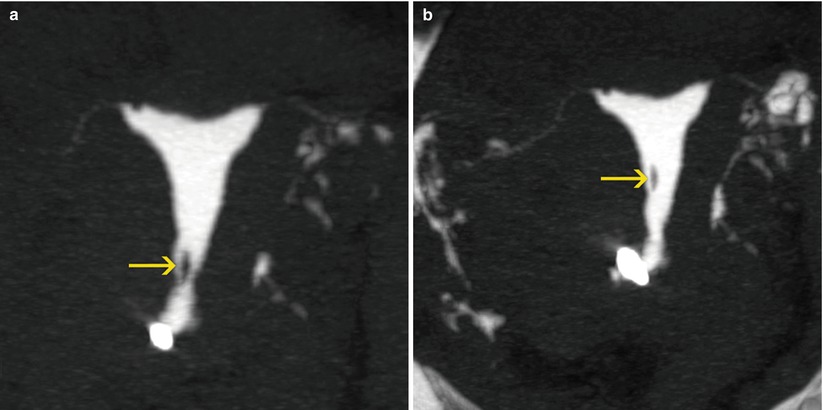
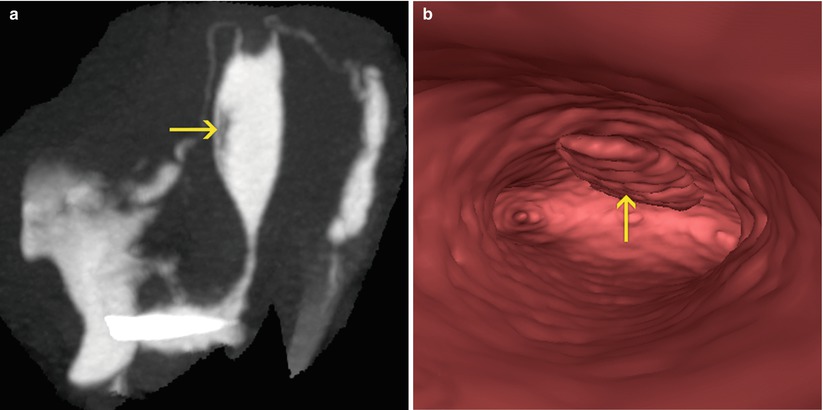
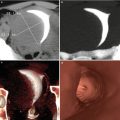
Fig. 12.1
Mucous secretions: (a) Maximum intensity projection image where a lineal filling defect is visualized adjacent to the anterior uterine wall (arrow), corresponding to secretions. (b) Virtual endoscopy image showing the mucous secretions (arrow)
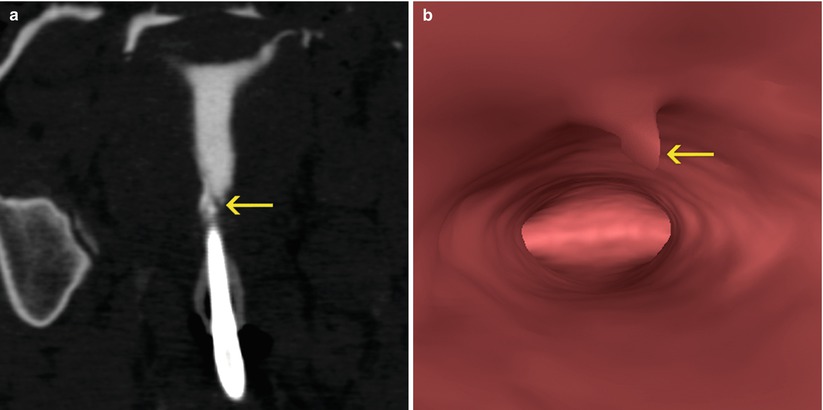
Fig. 12.2
Mucous secretions: (a) Coronal multiplanar reconstruction image showing a small lineal filling defect on the left anterolateral wall in the lower endometrial cavity (arrow). (b) Virtual endoscopy image showing the mucous secretion that acquires a polypoid appearance (arrow)
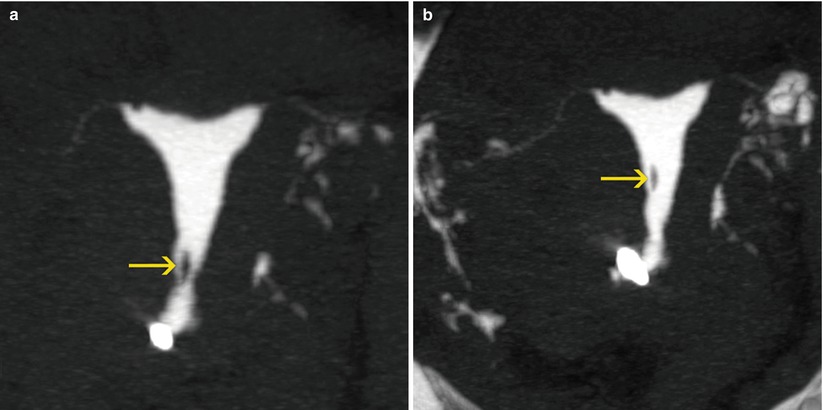
Fig. 12.3
Mucous secretions: (a) Coronal maximum intensity projection (MIP) image showing a lineal filling defect in the isthmic region of the endometrial cavity (arrow). (b) Delayed coronal MIP image demonstrating a change in the position of the filling defect, interpreted as a mobile mucous secretion (arrow)
Another case of misinterpretation is when the uterine folds are prominent and simulate elevated lesions in the endocervix as well as in the endometrium (Fig. 12.4). The prominent folds are of unknown etiology, and could be formed by the arrangement of longitudinal muscle bundle on the uterine wall. Likewise it has been reported that they correspond to remnants of the fusion of the Müllerian ducts [9]. In most cases they are easily distinguished due to the fact that they are elongated, parallel to the uterine longitudinal axis and their regular morphology (Fig. 12.5). A situation that favors their visualization is presented when an optimum distention of the cavity is not achieved. On occasions, the prominent folds may generate confusion when the protrusion is more focused and bulbous than linear (Fig. 12.6).
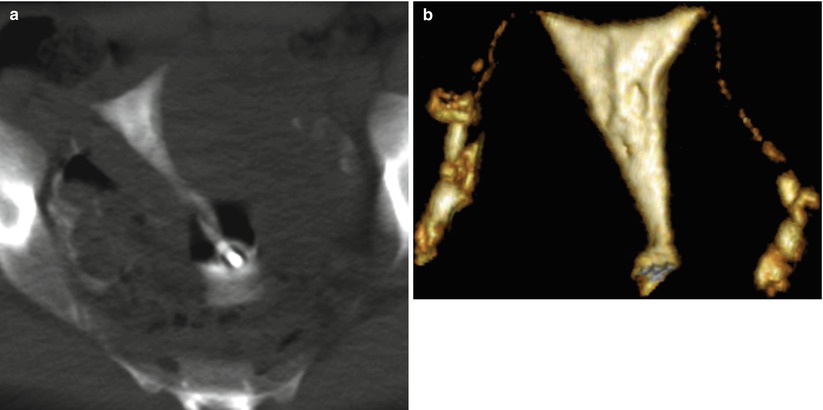
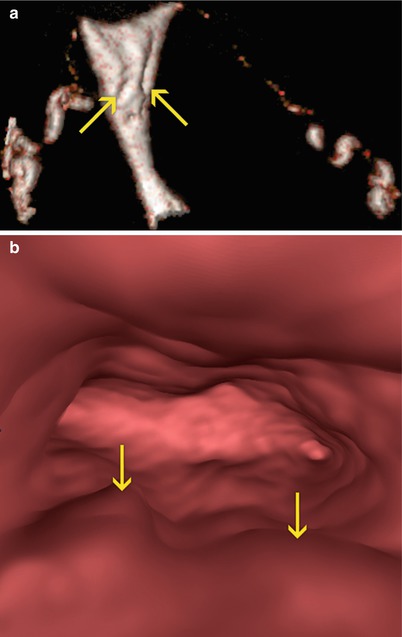
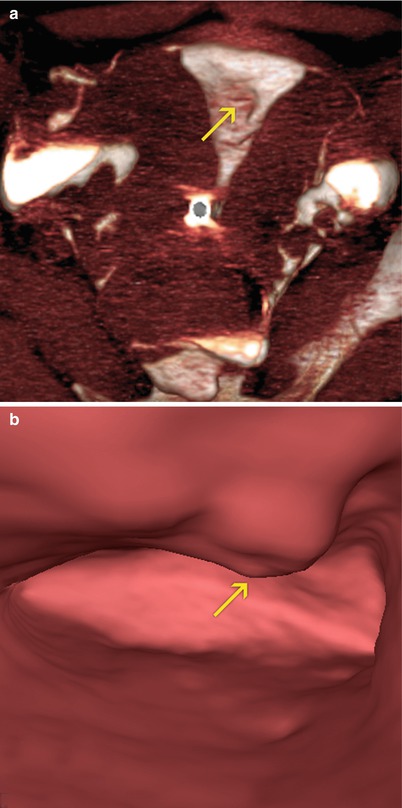
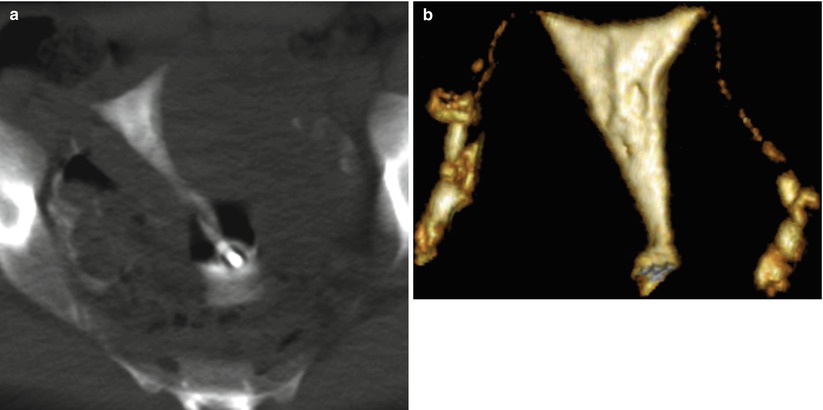
Fig. 12.4
Uterine folds. Lineal filling defects are visualized parallel to the uterus’ axis, corresponding to prominent uterine myometrial folds. (a) Coronal multiplanar reconstruction image. (b) Coronal 3D volume rendering image
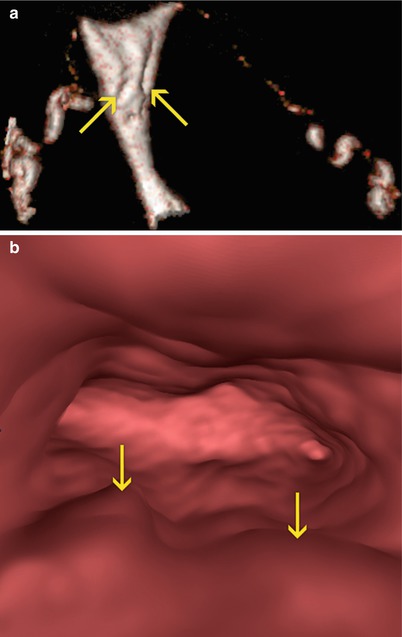
Fig. 12.5
Uterine folds. Linear filling defects are visualized parallel to the uterus’ axis, corresponding to prominent uterine myometrial folds (arrows). (a) Oblique coronal 3D volume rendering image. (b) Virtual endoscopy image
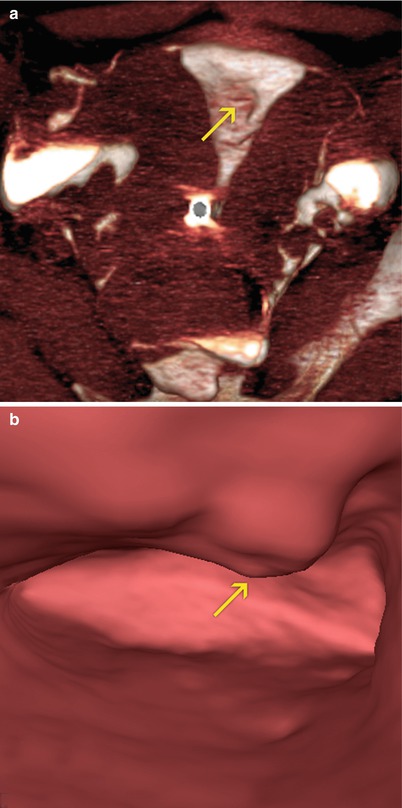
Fig. 12.6
Uterine fold. An indentation on the anterior surface of the uterine cavity is visualized (arrows) corresponding to an enlarged uterine fold simulating a polyp lesion. (a) Axial 3D volume rendering image. (b) Virtual endoscopy image
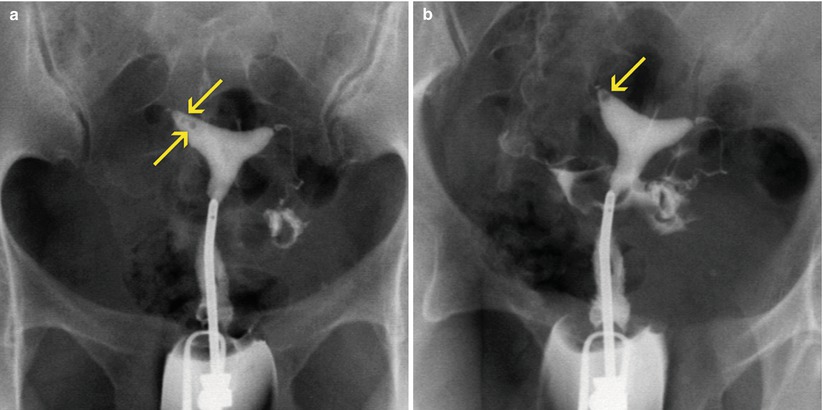
A frequent cause of error in HSG studies occurs when air bubbles get into the uterine cavity through the cannula during the procedure. The bubbles can be mistaken for filling defects lesions on hysterosalpingograms (Fig. 12.7). This scenario does not repeat itself in VHSG due to the fact that air density is easily distinguished on bidimensional images (Fig. 12.8). They only can simulate a polyp on tridimensional and virtual navigation views (Fig. 12.9); hence the importance of use all analysis tools for an appropriate interpretation of the findings.