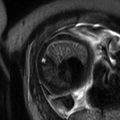
Fig. 12.1
Thick slab magnetic resonance imaging (MRI). Sonographic assessment of the head of the left twin is difficult due to his position and the position of the right twin who covers his head. This difficulty can be overcome on MRI
Fig. 12.2
Twenty-one gestational weeks. Thick slab MRI (a) shows why the assessment of the back of the left twin is difficult for the sonographer. In SSFSE sequence, T2WI, axial plane, one can clearly see the meningocele (MC) in the lumbar-sacral part of the vertebral column (b) and features of Chiari II malformation in the posterior cranial fossa (c)
Search for the existing literature in PubMed does not bring any results as far as triplet and higher number multiple pregnancies are concerned in terms of the use of MRI to assess the fetuses. The author’s personal experience also concerns only twin pregnancies, and these will be the subject of further considerations.
The sequences of MR examination are exactly the same when imaging a twin pregnancy. There is one major technical problem in this case, i.e., that it is more time consuming: first, because there are two fetuses to be examined and evaluated and secondly, because twins are much more mobile than singletons, especially in earlier gestation (Fig. 12.3), and this makes imaging more difficult and longer [6]. The time of the study cannot be too long as it is uncomfortable for the mother, so imaging twins is a challenge to radiologists and radiographers.
Fig. 12.3
Twin pregnancy examined at 21 gestational weeks in SSFSE sequence, T2WI (a, b). Note the artifacts resulting from movement of the fetuses and of the amniotic fluid (white and black fluid). The contents of the (en)cephalocele sac are difficult to assess. Second fetal MRI (SSFSE/T2WI) at the gestational age of 33 weeks with significantly reduced movements and artifacts (c–e) and postnatal imaging (f – FSE/T2WI, g – SE/T1WI post Gad) allows diagnosis of atretic cephalocele containing the meninges, fibrous tissue, and – possibly – some altered brain tissue
12.4 Developmental Anatomical Differences Between Singletons and Multiples
Twins are not the same as two single fetuses – for example, it has been shown in the study of cortical folding that the normal development of the brains of twins differs from that in singleton pregnancies. The cortical thickness, surface, and volume are significantly reduced at birth in twins as compared to singletons [7]. The entire volume of cerebrospinal fluid is greater in twins than in singletons, while the ventricle volumes do not differ between these two groups [8]. The cortical maturation and gyrification are delayed in twins, and the same applies to body maturation [7], e.g., twins are usually underweight for dates. Abdominal circumference is decreased in twins as compared to singletons [9]. This has to be taken into consideration when interpreting the findings and comparing them to the existing atlases or other sources of normal images and measurements’ values.
At the same time, general maturation of fetuses in multiple pregnancies in terms of neurological performance can be accelerated by 3–4 weeks or even more in small for gestational age (SGA) twins as compared to the appropriately grown infants of the same gestational age. The accelerated brain and lung maturation reflects an adaptation of the fetus to early extrauterine life [10]. Therefore, even “term” means something else in case of multiples as compared to singletons – it occurs earlier in twins who are ready to be born earlier; they do not grow any more after 38th gestational week while singletons do [11].
12.5 Congenital Anomalies Unrelated to Plurality
Congenital malformations occur more frequently in multifetal gestations because of the larger number of fetuses and the increased risk of anomalies in monozygotic pregnancies. But also, one fetus of a dizygotic twin pregnancy is twice more likely to have a chromosomal abnormality than a single one [4, 12].
In general, irrespective of zygosity, chorionicity, and amnionicity, in most cases of twin pregnancies (80–90 %), only one fetus has a defect, but in 10–20 %, both babies are affected (Fig. 12.4) [3]. The latter concerns mainly monozygotic twins that have the same karyotype except for these situations when genetic discordance is observed. Certain abnormalities occur more frequently in monozygotic twins, and they include anencephaly, holoprosencephaly, hydrocephalus, sacrococcygeal teratoma, and cardiac anomalies [3, 9, 12]. Esophageal atresia has been described as more common in twin pregnancies as well [9].
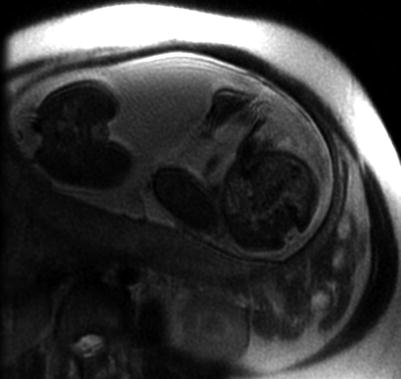
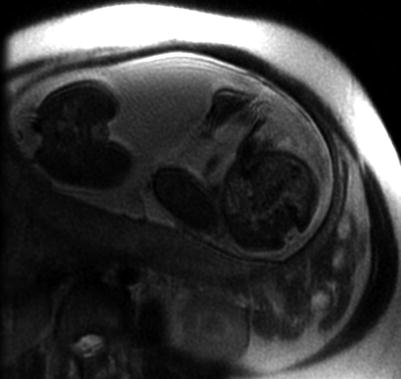
Fig. 12.4
SSFSE sequence, T2WI, axial plane. Axial section through the pelvis of both fetuses is shown in one slice, and spinal dysraphism and myelomeningocele (MMC) can be diagnosed in both twins
Any congenital malformation seen in a singleton pregnancy can occur in multiple gestation, and its imaging characteristics are the same as described in the previous chapters (Fig. 12.5). Few available publications show that in a significant number of cases, MRI brings important new diagnostic information compared with ultrasound also in multifetal gestations (Fig. 12.6) [6, 13, 14].
Fig. 12.5
Fetal MRI in SSFSE sequence, T2WI. In the parasagittal-oblique section through the left twin, gastroschisis was found with herniation of the bowel. Below, one can see a rounded tissue mass (a) which – in view of bladder non-visualization in any sequence and projection – corresponds to bladder exstrophy (b)
Fig. 12.6
In this pair of twins examined at the gestational age of 30 weeks, hydronephrosis and megaureter on the right side and no left kidney were found on US in one fetus. MRI (SSFSE, T2WI) disclosed the ectopic left kidney located between the bladder and the vertebral column in the right twin and confirmed the other findings (a – axial plane, b – coronal plane).
The correct diagnosis influences strongly the management which is somewhat different than in singleton pregnancies – the parents are offered three options:
1.
To continue the pregnancy
2.
To terminate pregnancy as a whole
It is important to know the chorionicity (Sect. 12.6) before offering the third option because of the increased risk of loss of the unaffected fetus in monochorionic gestation.
In most countries, pregnancy termination is allowed up to approximately 24 weeks of gestation, so early diagnosis is necessary to elect this option. If the abnormalities occur or are detected later, there is still place to limit intensive care in neonatal clinic after birth which also requires psychological preparation of the parents.
Selective feticide is also subject to the risk of neurological complications: long-term outcome after selective termination of the affected fetus in MC pregnancy includes neurodevelopmental impairment in 5 % and cerebral palsy in 2 % of cases. It is advisable then to image the surviving fetus after the procedure like after sIUFD (Sect. 12.6.1).
12.6 Complications of Twin Gestations
As stated before, monozygosity carries higher malformation risk, but it is chorionicity that is the main determinant of fetal outcome in twin pregnancies [3] with monochorionic monozygosity as the greatest exposure to anomalies and death [4]. Therefore, it is crucial to know the chorionicity as soon as possible, and it is US that is capable of determining chorionicity and amnionicity and of differentiating mono- and dichorionic twin pregnancies in the first trimester, optimally around the 10th week of gestation, on the basis of:
The presence of chorion between the amniotic membranes forming a thick septum in dichorionic diamniotic pregnancy, known as a “Y” sign, a lambda sign, or a twin peak sign
Two amniotic sacs in monochorionic diamniotic pregnancy with a thin intertwin membrane perpendicular to the placenta (a “T” sign)
Knowing the chorionicity, one can explain the difference in size of the twins: in dichorionic twins, intrauterine growth retardation (IUGR) of the smaller fetus can be diagnosed, while in monochorionic gestation, twin-twin transfusion syndrome (TTTS) should be taken into account (Sect. 12.6.2) although not every discordance in MC twins is TTTS: selective IUGR (sIUGR) should also be kept in mind.
Complications specific for twin gestations include consequences of intrauterine death of one twin to another one, twin-twin transfusion syndrome (TTTS), twin anemia-polycythemia syndrome (TAPS), twin reversed-arterial-perfusion syndrome (TRAPS), and conjoined twinning.
12.6.1 Intrauterine Death of One Twin
Single intrauterine fetal demise (sIUFD) is described here although it should not be considered as a complication specific for twin gestations in every case because it may result from the same problems that cause intrauterine fetal demise in a singleton pregnancy, i.e., structural abnormalities, abruption, placental insufficiency, growth restriction, cord abnormalities, infection, and maternal disease. It is estimated to occur in up to 7 % of twin gestations in the second and third trimester. According to some authors, in more than 20 % of twin pregnancies, first trimester embryonic loss (vanishing twin syndrome) occurs up to 7 weeks of gestation [16].
In DC pregnancy, vanishing twin syndrome is the most frequent complication and may be considered as spontaneous reduction of multiple pregnancy. The vanishing twin is then partially or completely reabsorbed by the co-twin. If the process of fetal resorption fails, the dead fetus is compressed by its growing co-twin to a flattened form called fetus papyraceus which may be seen on imaging (US, MRI) in the second half of pregnancy. In rare cases, it may block the cervix and require a cesarean section to deliver the living co-twin.
In dichorionic pregnancy, the surviving twin is usually normal – its impairment occurs in 1 % of cases. The outcome is significantly worse in case of a survivor in the monochorionic pregnancy with the impairment rate of 18 %. Damage to the central nervous system, gastrointestinal system, kidneys, and lungs is observed in many of these cases [9]. Both ultrasound and MRI were recommended to be performed 3–4 weeks after the death of one twin in order to detect anomalies in the survivor [17]. Nowadays, this delay is not justified anymore – with use of diffusion-weighted imaging (DWI), acute cerebral insult can be detected much earlier: as early as even after 24 h [18].
Co-twin death occurs in approximately 4 % of cases of DC pregnancies and 12 % of MC ones [17].
12.6.2 Twin-Twin Transfusion Syndrome (TTTS)
TTTS occurs in approximately 10 % of MC twins and is defined as severe amniotic fluid discordance.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree