The metatarsophalangeal (MTP) joint complex is a weight-bearing structure important to the biomechanics of the standing position, walking, shoe wearing, and sport participation. Acute dorsiflexion injury of the first MTP joint, “turf toe,” is common among American football and soccer players. The first and lesser MTP joint complexes can be affected by degenerative or inflammatory arthritis, infarct, and infection. These conditions can lead to plantar plate disruption. Imaging studies help physicians to properly diagnose and treat this condition. This article reviews the anatomy, diagnostic imaging, and clinical management of injury and pathology of the first and lesser MTP joint complexes.
Key points
- •
Acute and traumatic injuries are more common at the first MTP joint and degenerative injuries are the main cause of lesser MTP plantar plate tears.
- •
MR imaging is the most powerful imaging tool to evaluate soft tissue and cartilaginous damage related to the turf toe and plantar plate injuries.
- •
Familiarity with typical patterns and classifications of plantar plate tears of the lesser MTP joints enhances detection and characterization of the lesions by the interpreting radiologist.
- •
Lesser metatarsal supination and second metatarsal protrusion may correlate with plantar plate tears.
Introduction
Forefoot pathology is a most challenging orthopedic subject owing to the anatomic complexity, the sophistication of its biomechanics, and the range of pathology, stressors, and injury that may occur over the course of a lifetime. The fine-tuned balance of the human forefoot can be disturbed by subtle forces, repetitive trauma, and degenerative conditions that set off a deleterious chain of events that lead to pain, overload, and, finally, permanent deformities.
Recognition that injuries to the greater and lesser metatarsophalangeal (MTP) joints can be terribly disabling has inspired increased interest in research and treatment of MTP joint pathology. The onset of new and efficient diagnostic and therapeutic alternatives for forefoot pathology must be based on robust knowledge of the regional anatomy, clinical observation, and an understanding of the range of conditions that affect the MTP joints.
Introduction
Forefoot pathology is a most challenging orthopedic subject owing to the anatomic complexity, the sophistication of its biomechanics, and the range of pathology, stressors, and injury that may occur over the course of a lifetime. The fine-tuned balance of the human forefoot can be disturbed by subtle forces, repetitive trauma, and degenerative conditions that set off a deleterious chain of events that lead to pain, overload, and, finally, permanent deformities.
Recognition that injuries to the greater and lesser metatarsophalangeal (MTP) joints can be terribly disabling has inspired increased interest in research and treatment of MTP joint pathology. The onset of new and efficient diagnostic and therapeutic alternatives for forefoot pathology must be based on robust knowledge of the regional anatomy, clinical observation, and an understanding of the range of conditions that affect the MTP joints.
Anatomy of the metatarsophalangeal joints
Although the general structure of MTP joints of the great and lesser toes follows a similar pattern, important anatomic differences exist between the first and the second through fifth rays. All 5 metatarsal heads are rounded and convex in the sagittal plane, but the head of the first metatarsal has a larger transverse than vertical dimension, which results in a slightly flattened appearance. Conversely, the heads of the lesser metatarsals (second to fifth) are larger in the vertical than the transverse dimension, resulting in a more slender appearance in the coronal plane.
The first metatarsal head has 2 different articular surfaces. The superior surface, which articulates with the proximal phalanx, is convex and wide, extending to the dorsal aspect of the metaphysis. A sagittal plane crest (the “crista”) divides the plantar articular surface into 2 grooves, one for each hallucal sesamoid. The medial groove is deeper and wider than the lateral groove to accommodate the larger tibial sesamoid ( Fig. 1 ).
Sagittal plane stability of the first ray MTP joint is provided by the glenosesamoid apparatus, a gliding and pressure-absorbing mechanism formed by the 2 sesamoids embedded in a thick fibrous tissue (Gillette, 1872) —in combination with the intrinsic and extrinsic muscles of the hallux. The medial plantar tubercle at the base of the proximal phalanx of the hallux is the insertion site for the medial head of the flexor hallucis brevis (medial) and abductor hallucis tendons. The plantar plate anchors to the adjacent inferior margin of the proximal phalanx. The lateral head of the flexor hallucis brevis (lateral) and conjoint tendon of the adductor hallucis muscle (adductor hallucis oblique and transverse bellies) all insert onto the lateral plantar tubercle of the proximal phalanx. Both sesamoids are embedded in the plantar plate, which receives fibers from flexor hallucis brevis tendons, lateral deep intermetatarsal ligament, plantar fascia, and suspensory ligaments ( Table 1 ).
| Anatomic Structure | Special Characteristics |
|---|---|
| FHB tendon (medial head) | Inserts on medial plantar tubercle at base of proximal phalanx of the hallux |
| Abductor hallucis tendon | Inserts on medial plantar tubercle at base of proximal phalanx of the hallux (together with FHB) |
| Plantar plate | Formed by fibers from the FHB tendon, lateral deep intermetatarsal ligament, plantar fascia, and suspensory ligaments, with contribution from aponeurotic fibers of extensor hood Extends from distal margin of the intersesamoidal ligament Inserts on inferior plantar margin of the proximal phalanx Often difficult to visualize as distinct structure unless thickened or surrounded by edema |
| FHB tendon (lateral head) | Inserts on lateral plantar tubercle of the proximal phalanx of the hallux |
| Adductor hallucis tendon (conjoint tendon from oblique and transverse muscle bellies) | Inserts on lateral plantar tubercle of the proximal phalanx of the hallux (together with FHB) |
| Proper collateral ligaments (medial and lateral) | Course obliquely to insert on medial and lateral phalangeal tubercles |
| Accessory collateral ligaments (medial and lateral) | Insert broadly along medial and lateral borders of the MTP joint plantar plates |
| Hallucal sesamoids (tibial and fibular) | The medial sesamoid is slightly wider and larger than the lateral |
| Intersesamoid ligament | Transverse ligament that runs between the tibial and fibular sesamoids |
| Metatarsal–sesamoid ligaments (medial and lateral) | Thickened portions of the plantar capsule that may be hard to distinguish from capsule Originate with joint capsule from plantar aspect of first metatarsal and attach to proximal margin of respective sesamoid |
| Sesamoidal–phalangeal ligaments (medial and lateral) | Extend from distal margin of sesamoids to plantar base of the proximal phalanx |
Of the hallucal sesamoids, the medial one is slightly larger. A strong intersesamoid ligament binds the tibial and fibular sesamoids and forms the roof of a fibrous tunnel for the flexor hallucis longus tendon ( Figs. 2 and 3 ).
At the dorsal aspect of the first MTP joint, the extensor system includes the extensor hallucis longus and extensor hallucis brevis tendons and the extensor hood that is composed of oblique and transverse aponeurotic fibers that extend around the capsule and blend on the plantar aspect with the plantar plate and deep transverse intermetatarsal ligament.
The lesser metatarsal distal articular surfaces are bicondylar, with 2 plantar articular segments separated by a central concavity; typically, the lateral condyle is larger. In rare instances (1.8%), there are sesamoids of the lesser MTP joints.
On each side of the lesser metatarsal heads, there are bony tubercles (epicondyles) that provide insertion sites for the MTP collateral ligaments (proper collateral ligaments) and for the fan-shaped suspensory metatarsoglenoid ligaments (accessory collateral ligaments). The MTP joint proper collateral ligaments, which course obliquely to insert onto the medial and lateral phalangeal tubercles, play an important role in stabilization of the joint in the transverse plane. The suspensory (accessory collateral) ligaments broadly insert along the medial and lateral borders of the MTP joint plantar plates, which they stabilize.
The rounded metatarsal heads articulate with shallow, ovoid, concave bases of the proximal phalanges. These “glenoid” cavities are smaller than the articular surfaces of the metatarsal heads, conferring a degree of inherent instability to the MTP joints.
The anatomy of the lesser MTP joints is somewhat simpler than that of the first ray. The fibrocartilaginous plantar plate is now recognized as the primary stabilizer of the lesser MTP joints, especially in the dorsal–plantar direction. The plantar plate firmly inserts onto the plantar bases of the lesser toe proximal phalanges. Along with its connections from the distal plantar fascia, accessory collateral ligaments (suspensory ligaments) and deep transverse intermetatarsal ligament, it acts as a cradle for the metatarsal head. Dorsal and plantar interossei and lumbrical tendons insert onto the bases of the proximal phalanges, helping to maintain balance and function of the lesser MTP joints. At the central plantar surface of the plantar plate, a fibrous tunnel accommodates the flexor digitorus longus and brevis tendons ( Table 2 ).
| Proximal | Phalanx | |
|---|---|---|
| Medial Plantar Tubercle (1) Medial Metatarsophalangeal Joint Capsule (2) | Lateral Plantar Tubercle | |
| Great toe | Abductor hallucis + medial head of flexor hallucis brevis (1) | Adductor hallucis + lateral head of flexor hallucis brevis |
| Second toe | First dorsal interosseous (1) First lumbrical (2) | Second dorsal interosseous |
| Third toe | First plantar interosseous (1) Second lumbrical (2) | Third dorsal interosseous |
| Fourth toe | Second plantar interosseous (1) Third lumbrical (2) | Fourth dorsal interosseous |
| Fifth toe | Third plantar interosseous (1) Fourth lumbrical (2) | Abductor digitus V + digitus V short flexor |
Both the extensor digitorum longus and brevis tendons cross the dorsal surface of the lesser MTP joint inside a fibroaponeurotic sling—the extensor hood—that helps to maintain joint balance ( Figs. 4 and 5 ).
Turf toe (first metatarsophalangeal joint)
Hyperextension injury of the first MTP joint was first reported by Ryan and colleagues in 1975. The following year, Bowers and Martin coined the term “turf toe” owing its prevalence in American football players injured while wearing flexible shoes on artificial turf.
Unfortunately, varied pathologies of the first MTP joint have been incorrectly bundled along with the diagnosis of turf toe, creating some confusion in the literature. The classic “turf toe” lesion occurs when an axial force is applied to the foot while the great toe is fixed to the ground with hyperextension of the MTP joint ( Fig. 6 ). The glenosesamoid apparatus and the plantar ligaments are the most frequently injured structures. Depending on the intensity of the force applied to the foot, injuries can range in severity from mild sprain to complete disruption of the plantar structures ( Table 3 ).
| Injury | Grade | Description |
|---|---|---|
| Hyperextension (turf toe) | I | Attenuation of the glenosesamoid complex Local tenderness, minimal swelling and ecchymosis |
| II | Partial tear of the glenosesamoid complex Diffuse tenderness, moderate swelling and ecchymosis Restricted painful movement | |
| III | Complete disruption of the glenosesamoid complex Severe tenderness, marked swelling and ecchymosis Limited painful movement + positive MTP drawer test | |
| Hyperflexion (sand toe) | Hyperflexion injury of MTP or interphalangeal joint Lesser MTP joints may be involved | |
| Dislocation | I | Dislocation of the hallux with the sesamoids No lesion of the intersesamoid ligament |
| IIA | Associate disruption of the intersesamoid ligament | |
| IIB | Associate transverse fracture of one of both sesamoids | |
| IIC | Complete disruption of the intersesamoid ligament with fracture of one of the sesamoids |
In contradistinction to turf toe, “sand toe” was described as an injury resulting from hyperplantarflexion of any of the MTP joints. This most commonly occurs in barefoot beach volleyball players. The most frequently affected structures in sand toe are the extensor tendons, the extensor hood and the articular capsule.
Diagnosis
The diagnosis of the first MTP joint injuries is based not only on an accurate history, but also thorough physical examination and imaging studies. It is important to identify the points of tenderness, ecchymosis, and swelling to correlate them with the deep anatomic structures potentially involved in the lesion.
The MTP joint drawer test is very useful to establish and grade joint instability. It is important to test the joint stability in different directions—varus stress/valgus stress/hyperflexion—because of the possibility of coexisting lesions in multiple planes. Comparison with the asymptomatic contralateral foot is extremely helpful.
Weight-bearing anteroposterior and lateral radiographs may show avulsion fractures of the proximal phalanx and sesamoids as well as proximal migration of the sesamoids, which may accompany complete rupture of the distal insertion of the glenosesamoid apparatus. Waldrop and colleagues showed that, when the distance between the sesamoids and the proximal phalanx differed by 3 mm or more between the right and left feet, then that was a significant and predictive of severe injury to the hallucal plantar plate ( Fig. 7 ).
A dorsiflexed lateral radiograph of the hallux or fluoroscopic imaging can easily assess proximal migration of the glenosesamoid apparatus, diastasis of sesamoids, fractures or other coexisting lesions.
MR imaging is the most powerful diagnostic tool for assessment of soft tissue and cartilaginous injuries related to turf toe. By comparison, radiography, arthrography, and computed tomography have limited tissue contrast resolution, which is necessary to delineate the fine anatomic structures of the MTP joint of the great toe. Although high-resolution ultrasonography can delineate soft tissue structures about the first MTP joint, it is not useful for the evaluation of the associated osseous and cartilaginous injuries.
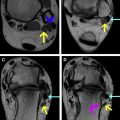
The MR imaging protocol should include at least 1 non–fat-suppressed T1-weighted or proton density-weighted sequence to delineate the anatomy ( Figs. 8 and 9 ). Some authors prefer proton density weighted sequences because of the superior detail of the ligaments and tendons and the improved delineation of the chondral surfaces. In addition, fat-suppressed proton density-weighted sequences or short tau inversion recovery sequences in the coronal, axial, and sagittal planes are recommended for optimal evaluation of fluid and edema associated with acute pathology.
The plantar plate and hallucal sesamoids are analyzed best in sagittal and coronal short axis planes. MR imaging can show variable patterns related to heterogeneous signal intensity resulting from a partial or complete tear of the plantar plate. The lateral deep intermetatarsal ligament is visualized only in the coronal short axis plane. Main collateral ligaments and sesamoid ligaments are analyzed best in the axial long axis and coronal short axis plane. Although it is not commonly performed, and unnecessary in the context of acute injury with posttraumatic fluid signal distention of the joint, MR arthrography has been reported to enhance visualization of many of these structures.
Treatment
First-line treatment of turf toe is conservative based on “RICE” (rest, ice, compression, and elevation). Non–weight-bearing protection or immobilization of the joint is essential to control pain and prevent additional tissue damage in the acute posttraumatic period. After a few days, as pain subsides, careful rehabilitation commences. The challenge lies in finding the balance between the restoring the physiologic range of motion and protecting the healing tissues. Taping and rigid insoles are often used to protect the great toe MTP joint, until recovery is complete.
All grades of turf toe can be treated conservatively; however, higher grade injuries take longer to heal, with greater delay in return to full activity. Fortunately, few cases of turf toe require surgical treatment. According to McCormick and Anderson, there are strict indications for surgical treatment of turf toe that include ( Box 1 ): (1) large capsular avulsion with unstable joint (coronal, sagittal or transverse planes), (2) diastasis and/or retraction of the sesamoids (fracture or bipartite), (3) traumatic hallux valgus/varus deformity, (4) osteochondral injury (including loose bodies), and (5) failed conservative treatment.