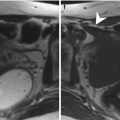
Fig. 9.1
Appearance of the normal testes on MR imaging. Coronal images. (a, b) The testes show high signal intensity on T2- and intermediate signal intensity on T1-weighted images, respectively. The tunica albuginea has low signal intensity in all sequences. (c) Diffusion-weighted image (b = 1,000 s/mm2) shows signal restriction of the testicular parenchyma
The fluid between the visceral and the parietal layers of the tunica vaginalis shows high and very high signal intensity on T2- and heavily T2-weighted images, respectively [5, 6].
9.4 Congenital Abnormalities
MR imaging is the imaging modality of choice in investigating patients with ambiguous genitalia, which are usually associated with complex malformations of the genitourinary tract. The most common isolated abnormalities of the scrotal content are undescended testis and congenital hydroceles. Bell-clapper deformity is difficult to be detected. Polyorchidism and adrenal rests are rare.
9.4.1 Undescended Testis
Undescended testis is the most common genitourinary anomaly with a prevalence at birth of 2–5 % and up to 30 % in preterm infants. Approximately 2:3 undescended testes will spontaneously descend within the first months of life, with a prevalence at the age of 1 year of 0.8 %. The testis may be located at any point along the descent route from the retroperitoneum to the external inguinal ring [18]. It can be ectopic, but in general it is found along the normal path of descent: approximately 70 % in the inguinal canal, 20 % in the prescrotal region just beyond the external inguinal ring, and the remaining in the abdomen. About 3–5 % of patients with undescended testis have congenital absence of the testis. It is conceivable that in most cases, the testis was originally present during fetal life and then regressed.
The major complications of cryptorchism are malignant degeneration, infertility, torsion, and bowel incarceration because of an associated indirect inguinal hernia. Tumors are far more common in an undescended testis than in a normally positioned testis.
Imaging is indicated to search for the location of the cryptorchid testis to evaluate its size and to seek for parenchymal lesions. The cryptorchid testis is usually smaller relative to the normally located testis because of testicular dystrophy and degeneration [19].
Ultrasonography can reliably detect testicles located in the inguinal canal or between the external inguinal ring and the scrotal neck. Detecting the testicle in intra-abdominal locations is often difficult or even impossible. MR imaging allows detecting the testis not only in the inguinal canal but also in the abdomen. High abdominal testes, however, may be difficult to identify, and a recent meta-analysis of an American pediatric group shows a low sensitivity [20]. DWI performed at high b-values (800–1,000 s/mm2) improves visualization of the undescended testis which appears hyperintense in most of cases [13] (Fig. 9.2). Severely atrophic testes, however, may show low signal intensity on diffusion-weighted imaging [21] (Fig. 9.3).
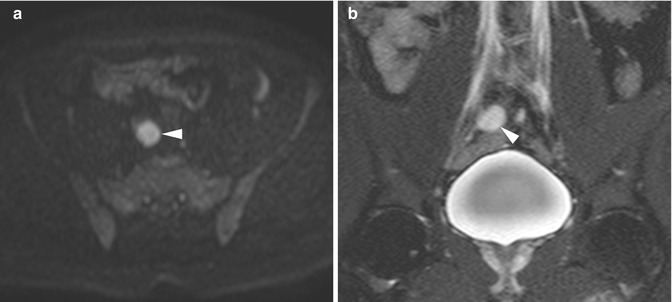
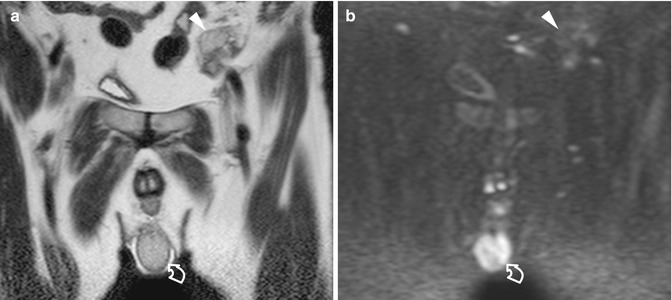
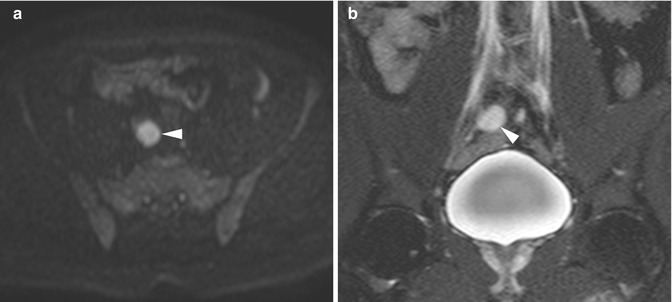
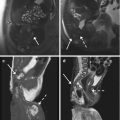
Fig. 9.2
An undescended testis located in the abdomen near the right iliac vessels. (a) Axial diffusion-weighted image (b = 800 s/mm2) identifies the retained testis as a lesion with signal restriction (arrowhead). (b) Coronal T2-weighted image confirming the location of the testis adjacent to the right iliac vessels (arrowhead)
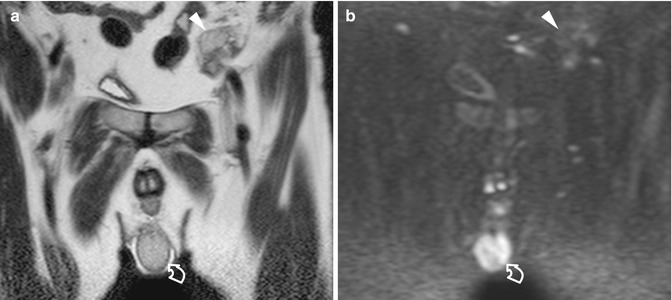
Fig. 9.3
An undescended testis located in the abdomen near the left iliac vessels. (a) Coronal T2-weighted image showing a normally descended right testis (curved arrow) and a small left testis adjacent to the left iliac vessels (arrowhead). (b) Coronal diffusion-weighted image (b = 1,000 s/mm2) fails to show signal restriction of the retained testis (arrowhead), which was markedly dystrophic and poorly vascularized at surgery (arrowhead). The normally descended right testis (curved arrow) displays signal restriction
9.4.2 Congenital Hydrocele
Congenital hydrocele occurs when there is incomplete closure of the processus vaginalis. It is very common in newborn but is encountered in less than 1 % of adults. The patent processus vaginalis permits flow of peritoneal fluid into the scrotum. Indirect inguinal hernias can be associated. There are two subtypes of congenital hydrocele: the encysted type, also called spermatic cord cyst, with no communication with the peritoneum and with the tunica vaginalis, and the funicular type, also called funiculocele, which communicates with the peritoneum at the internal ring but does not surround the testis.
Either ultrasonography or MR imaging can be used to evaluate congenital hydrocele. On ultrasound, it appears as an anechoic fluid collection surrounding the anterolateral aspects of the testis extending to the inguinal canal or as a well-demarcated anechoic mass, associated with either a patent or a closed internal ring, separated from the testis and epididymis which are displaced inferiorly. On MR imaging hydrocele is homogeneous and hypointense on T1-weighted images and hyperintense on T2-weighted images, characteristic of fluid. Occasionally, septations are identified, although prominent septations should suggest a hematocele or pyocele. Patency of the processus vaginalis with entry of peritoneal fluid into the scrotal sac is best demonstrated in heavily T2-weighted images.
9.4.3 Bell-Clapper Deformity
Failure of the normal posterior anchoring of the epididymis and testis is called bell-clapper deformity because it leaves the testis free to swing and rotate within the tunica vaginalis of the scrotum like the clapper inside of a bell. It is a common precondition for testicular torsion, with a 12 % incidence in an autopsy series.
Bell-clapper deformity itself is hard to be detected by imaging. A suggestive feature is the abnormal direction of the long axis of the testis on the axial plane, in the right-to-left or anterior-posterior direction with the epididymis right upon the testis (Fig. 9.4). The deformity is more often recognized in heavily T2-weighted images when hydrocele is present and the tunica vaginalis completely encircles the epididymis, distal spermatic cord, and testis rather than attaching to the posterolateral aspect of the testis.
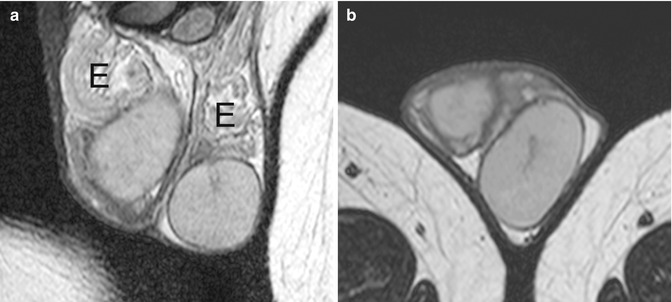
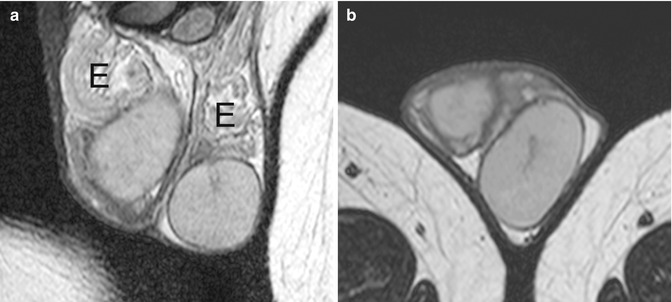
Fig. 9.4
Surgically proved bell-clapper deformity. The patient had several episodes of acute scrotal pain on both sides which released spontaneously, interpreted as recurrent episodes of low-degree torsion with spontaneous detorsion. Coronal (a) and axial (b) T2-weighted images show the major axis of the testes laying on an axial plane, the right testis in right-to-left direction, the left in anterior-posterior direction. The epididymis (E) is right upon the testes in both sides
9.4.4 Polyorchidism
Polyorchidism is a rare congenital abnormality where more than two testes are present which may have separate or common spermatic cords and epididymis. Although three testes is the most common form, as many as five have been reported. In approximately 75 % of cases, the supernumerary testes are intrascrotal. Of the remaining cases, 20 % of the supernumerary testes are inguinal and 5 % retroperitoneal. On ultrasonography the accessory testis presents with the same echogenicity, echotexture, and vascular pattern as the normal testes. On MR imaging it has the same signal characteristics as the normal testes: intermediate signal intensity on T1-weighted images, high signal intensity on T2-weighted images, and hyperintensity on DWI (Fig. 9.5). Thanks to its panoramicity and improved tissue characterization, MR imaging is helpful in making a definitive diagnosis in case of equivocal ultrasound findings or extrascrotal testes [22].
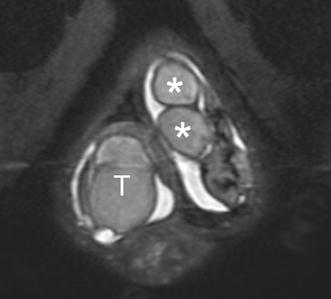
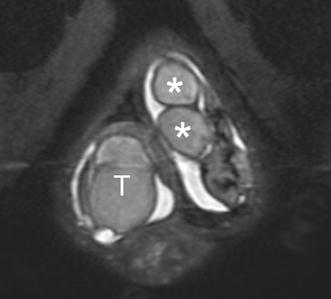
Fig. 9.5
Polyorchidism. Oblique-coronal T2-weighted image shows a single testis (T) on the right hemiscrotum and two testes (asterisks) in the left hemiscrotum
9.4.5 Testicular Adrenal Rests
Testicular adrenal rests derive from the hyperplasia of aberrant adrenal cortical tissue that descends during prenatal life with the testes or ovary. In approximately 8 % of patients with congenital adrenal hyperplasia, the elevated levels of serum adrenocorticotropic hormone stimulates these rests to grow. They are bilateral in more than 80 % of cases, usually presenting as palpable masses inside of or close to the mediastinum testis.
Testicular adrenal rests present on ultrasound as unilateral or bilateral lobulated masses with variable echogenicity located within or adjacent to the mediastinum testis. Acoustic shadowing may be due to fibrotic changes or calcifications. Lesions are isointense to the surrounding normal tissue of the testis on T1-weighted images and hypointense to the surrounding normal tissue of the testis on T2-weighted images with and without fat suppression. Strong enhancement is demonstrated after gadolinium administration.
9.5 Ischemic Disorders
The mainstay of imaging ischemic scrotal disorders is color Doppler ultrasonography. In high-degree torsion non-enhancement of the testis after gadolinium administration has been reported as highly sensitive and specific for torsion [14], but MR imaging is more expensive and time-consuming than color Doppler ultrasonography and therefore has no or minimum practical role in the setting of acute scrotal pain. In low-degree torsion perfusion is reduced compared with the healthy contralateral testis [23]. In acute testicular torsion, the testis has normal signal intensity on both T1- and T2-weighted images and high signal intensity on DWI [9]. The twisted spermatic cord is best demonstrated on transaxial T2-weighted and contrast-enhanced images [24]. In the subacute and chronic stages, the signal intensity of the testis changes due to necrosis and hemorrhagic components (Fig. 9.6).
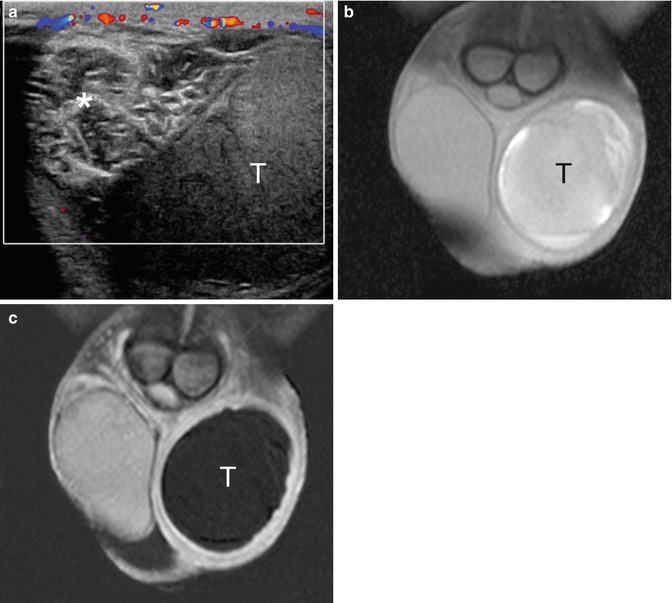
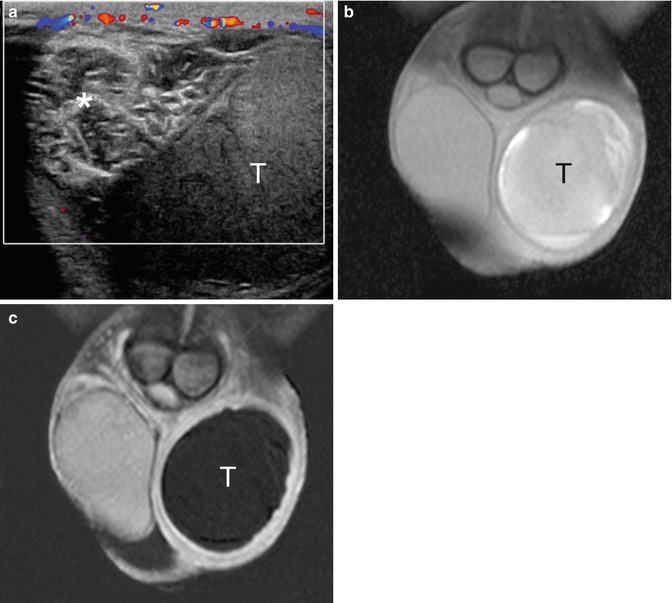
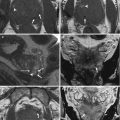
Fig. 9.6
Long-standing high-degree left testicular torsion. (a) Color Doppler interrogation shows an avascular left testis (T) and a twisted spermatic cord (asterisk). The paratesticular tissues display increased vascularization. (b) T1-weighted coronal image with fat suppression shows inhomogeneous left testis (T) with high signal intensity due to hemorrhagic changes. (c) Gadolinium-enhanced subtracted image showing complete lack of vascularization of the left testis (T) and slight hyperemia of the surrounding tissues
9.5.1 Torsion of the Appendages
The normal appendages are typically seen only when hydrocele is present [25–27]. They usually display intermediate signal intensity on T2-weighted images. In appendiceal torsion, a twisted and swollen appendage is usually seen as a hyperintense oval structure on T2-weighted images lacking intralesional enhancement with ring-like perilesional enhancement on dynamic subtraction contrast-enhanced images [2, 28].
9.5.2 Segmental Testicular Infarction
MR imaging has been claimed as a problem-solving technique in doubtful cases of segmental testicular infarction [29, 30]. On T1-weighted MR images, infarcts may appear isointense to the surrounding normal testicular parenchyma, occasionally with foci of high signal intensity due to hemorrhage.
On T2-weighted images, the signal intensity is variable. The lesion is avascular after gadolinium contrast administration (Fig. 9.7), often with an enhancing perilesional rim in subacute infarction [29, 31]. Although segmental testicular infarction presents with characteristic MR features, this investigation is not commonly performed in our clinical practice, as similar information is provided by contrast-enhanced ultrasonography which is quicker and with a lower cost [32].
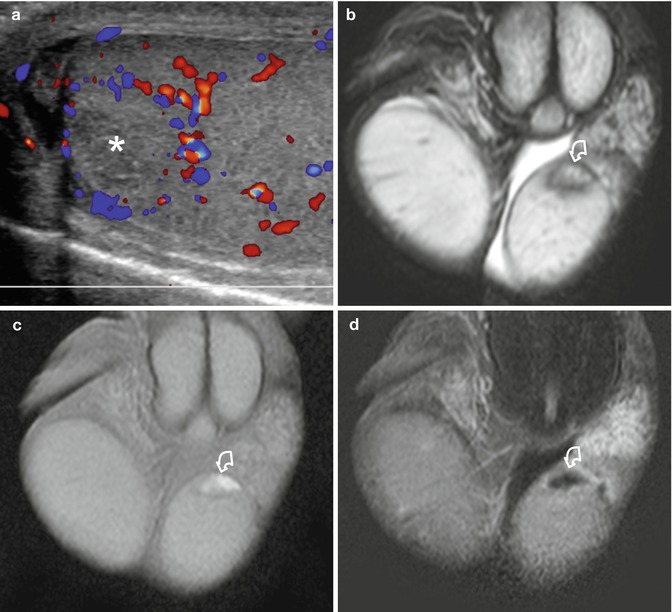
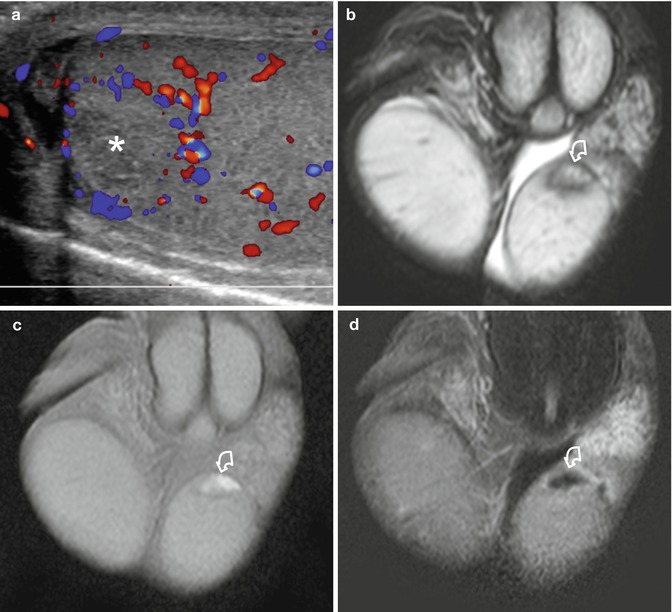
Fig. 9.7
Segmental testicular infarction. Patient presenting with acute left scrotal pain. (a) Color Doppler interrogation shows an avascular, slightly hypoechoic area (asterisk) in the upper pole of the left testis with perilesional hypervascularization. (b) T2-weighted coronal image showing the lesion (curved arrow) with inhomogeneous signal intensity. (c) T1-weighted image showing the hyperintense lesion (curved arrow) due to hemorrhagic changes. (d) Gadolinium-enhanced subtracted image shows lack of vascularization of the lesion (curved arrow) and slight perilesional hypervascularization
9.6 Inflammation
MR imaging provides a panoramic view of the extension of the disease to adjacent organs in severe scrotal inflammation. Involvement of the perineum and/or abdominal region can be investigated. MR imaging enables a diagnosis of postinflammatory testicular ischemia, testicular hemorrhagic and necrotic changes, epididymo-orchitis with abscess formation, and intrascrotal fistulas [33]. In acute epididymitis the enlarged epididymis has increased signal intensity relative to the normal side on T2-weighted images and clearly shows intense contrast enhancement on dynamic subtraction contrast-enhanced images. Abscesses are typically hypointense on T1-weighted images, hyperintense on T2-weighted images, and display high signal intensity on DWI images. They do not enhance, while the surrounding tissues show avid enhancement.
9.7 Testicular Masses
Not all intratesticular lesions are tumors, and not all testicular tumors are malignant. Granulomata, focal orchitis, fibrous pseudotumors, and spontaneous hematomas are often difficult to differentiate from tumors on ultrasound examination. In many cases, however, it is suggested that the diagnosis integrates the history of the patient, clinical presentation, and the superior capability of MR imaging for tissue characterization and evaluation of intralesional flows.
The patient’s age at presentation is important. Germ cell tumors are prevalent in the young while lymphomas in the elderly, and some histotypes are much more prevalent in prepuberal than in puberal boys. Clinical correlation is vital: many nonneoplastic intratesticular conditions are likely to manifest with acute scrotum. One needs to be cautious, however, because tumors can also occasionally manifest with pain. A history of fever or trauma may suggest a nonneoplastic origin as well. Tumor markers often help in the differential diagnosis between testicular tumors and nonneoplastic lesions. Normal serum tumor markers, however, do not rule out testicular neoplasms. In any case, traumatic and inflammatory changes evolve rapidly; if a nonneoplastic pathology is suspected, a short-term follow-up examination will likely allow differential diagnosis with tumor.
9.7.1 Dilated Rete Testis
Tubular ectasia of the rete testis is a benign nonneoplastic condition thought to result from partial or complete obliteration of the efferent ducts. It is more common in men over the age of 55 years, often bilateral, and frequently associated with spermatoceles.
Using modern ultrasonographic equipment, a tubular ectasia of the rete testis is characterized in virtually all patients; in case of doubt, however, MR can show the dilatation of multiple small tubules of the rete testis appearing hyperintense on T2-weighted and heavily T2-weighted images. After gadolinium administration no internal enhancement is seen [16].
9.7.2 Testicular Epidermoid Cyst
The classic ultrasonographic appearance of testicular epidermoid cyst is the “onion ring” pattern, consisting in alternating rings of low and high echogenicity, which represent layers of keratinized squamous epithelium. This appearance is virtually pathognomonic, but epidermoid cysts with an atypical appearance may be difficult to differentiate from tumors. On MR imaging an epidermoid cyst typically shows on T2-weighted images alternating zones of high- and low signal intensity [1, 34, 35] and signal restriction on DWI [11]. This appearance, however, is not constant (Fig. 9.8). Signal intensity on T1-weighted images is variable. No matter the imaging features, epidermoid cysts do not demonstrate internal flow on Doppler interrogation nor enhancement after gadolinium administration [16].
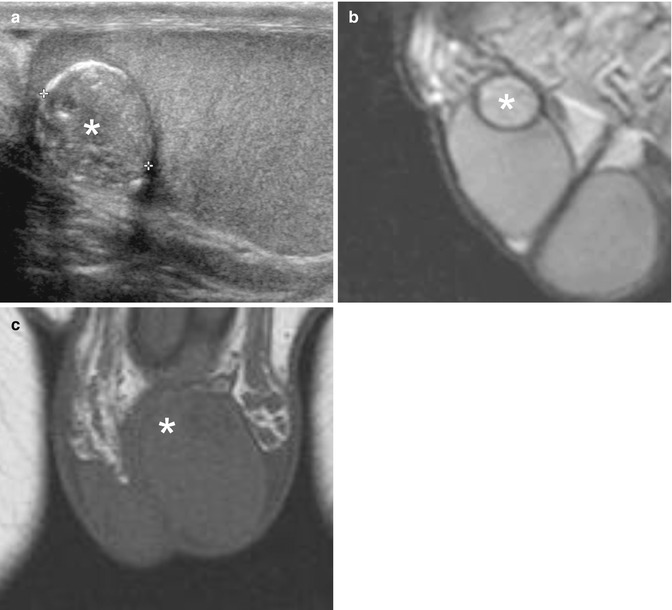
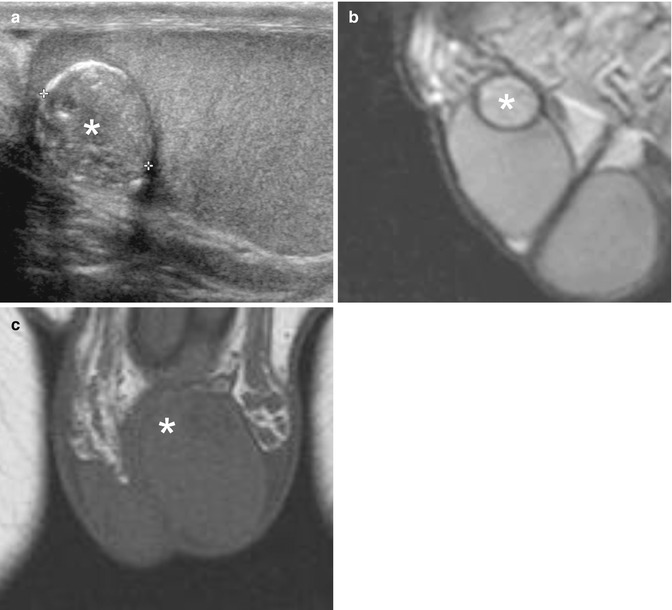
Fig. 9.8
Epidermoid cyst presenting as a palpable nodule of the left testis. (a) Grayscale ultrasonography showing a slightly inhomogeneous lesion isoechoic to the surrounding normal tissue of the testis, with a few wall calcifications (asterisk). (b) Sagittal T2-weighted image shows a slightly hyperintense nodule (asterisk) with hypointense wall. (c) Coronal T1-weighted image showing the lesion (asterisk) isointense to the surrounding normal tissue of the testis, which was completely avascular after gadolinium contrast administration (not shown)
9.7.3 Spontaneous Testicular Hematoma
Spontaneous intratesticular hematoma is a rare entity with few reports in the literature, mimicking a neoplasm on grayscale ultrasonography. Diagnosis of a nonneoplastic condition, however, is suggested as the lesion lacks vascularization on color Doppler interrogation and contrast-enhanced ultrasonography [36, 37]. MR imaging confirms the diagnosis showing a lesion with the characteristic signal changes of blood. No enhancement is seen after gadolinium contrast administration (Fig. 9.9). Follow-up is recommended to ascertain lesion size reduction and signal intensity changes over time of the blood content.
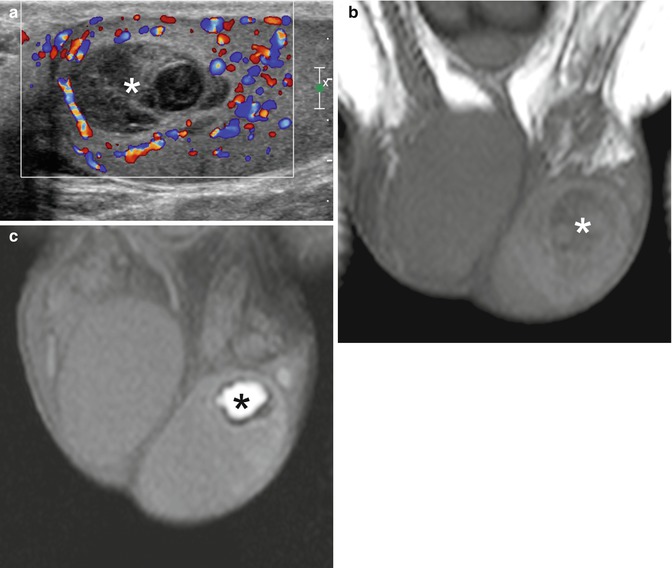
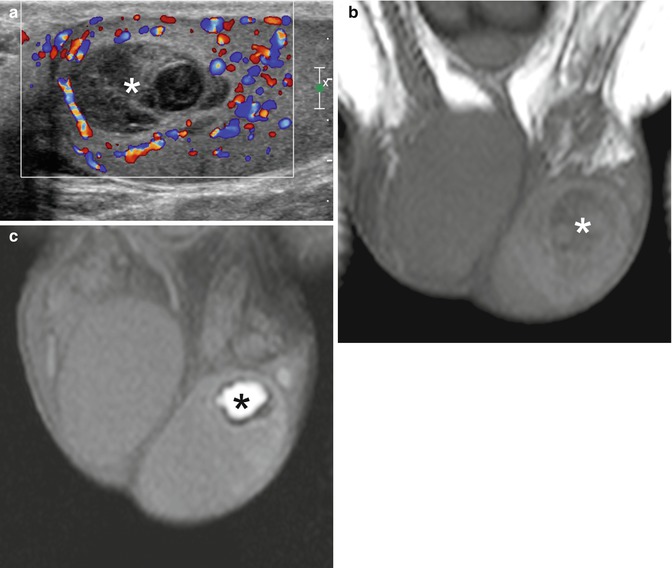
Fig. 9.9




Spontaneous testicular hematoma. The patient presented with acute left scrotal pain for 3 h with no history of trauma. (a) Color Doppler interrogation shows an inhomogeneously hypoechoic left testicular lesion lacking vascularization (asterisk). (b) Coronal T1-weighted image obtained within 24 h after ultrasonography shows an inhomogeneous isointense lesion (asterisk) which was avascular after gadolinium contrast administration (not shown). (c) Follow-up MR investigation obtained 2 months after the previous study. Coronal T1-weighted image shows a hyperintense lesion (asterisk) which is reduced in size, characterized by hypointense rim due to blood degradation
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree