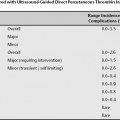
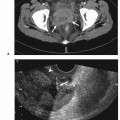
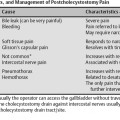
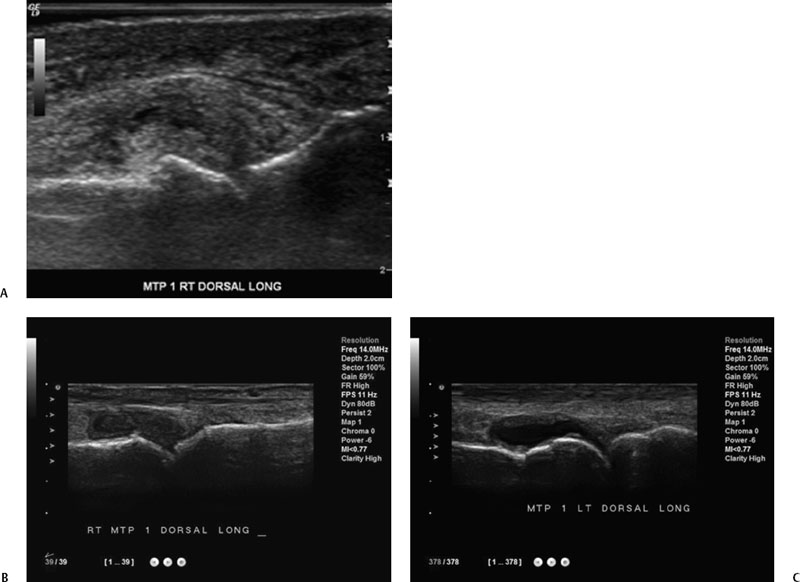
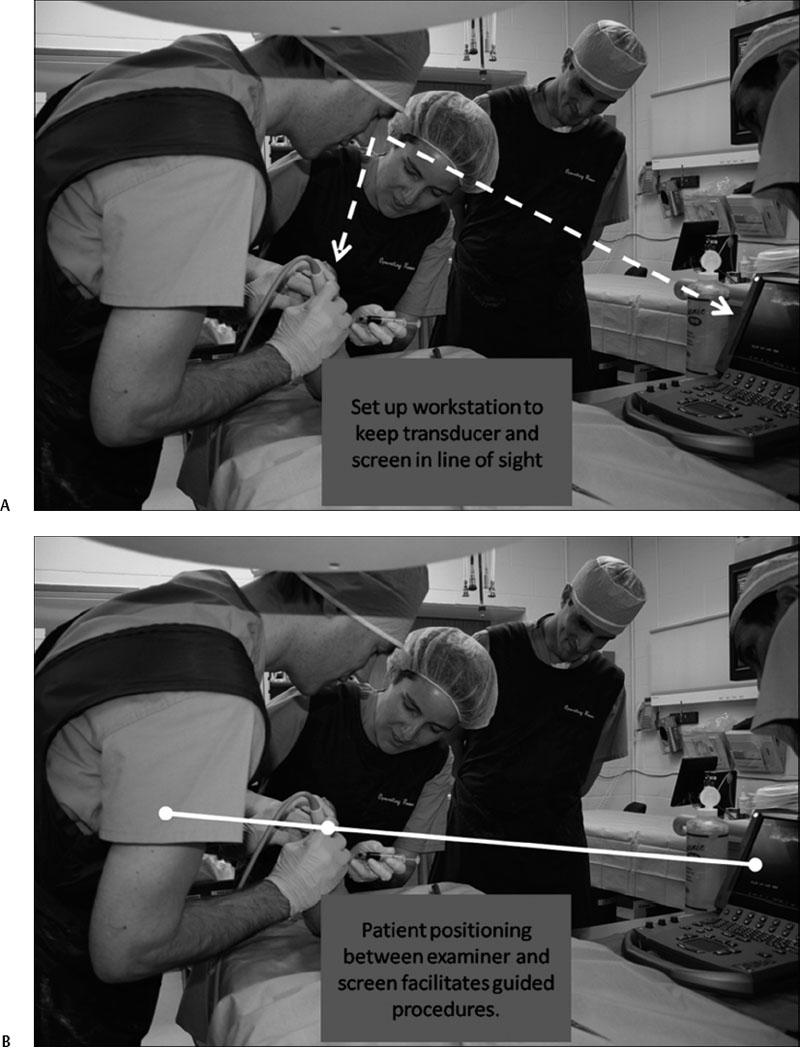
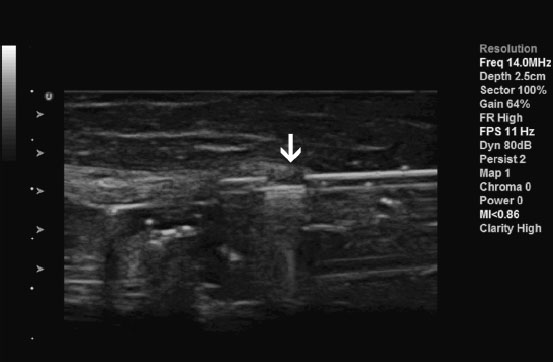
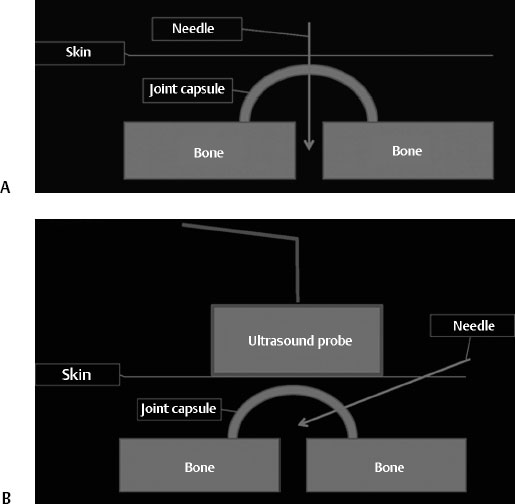
18 Musculoskeletal Joint Interventions Ultrasonography has been used to guide interventions for several decades. Interventional ultrasonography can be an office-based or bedside technique, or performed in a dedicated suite. Interventional ultrasonography in musculoskeletal medicine is used for diagnostic and therapeutic purposes. Fluid obtained is examined for In comparison with blind aspiration, the yield of sonographically guided aspirations is significantly higher, particularly in the small joints of the hands and feet. Guided-diagnostic aspirations are therefore more accurate, there is less delay in diagnosis and treatment, and referrals can frequently be avoided. Analysis of synovial tissue following biopsy can provide valuable insights into Ultrasound guidance can improve the yield of such biopsies because hypertrophied and hypervascularized synovial tissue can be accurately located. If ultrasound guidance is employed, even small joints will be accessible to biopsy. They include Adverse effects can be avoided if Typical indications for diagnostic joint aspirations are These etiologies can be readily determined sonographically and an unnecessary joint aspiration can be avoided. Preprocedure sonographic examination can also determine Fig. 18.1 Dorsal, long axis views centered over joint line of first metatarsophalangeal (MTP) joint in three different patients. All patients present similarly with pain and swelling of the first toe. (A) Shows distension of joint capsule by hyperechoic, crystalline material in a patient with chronic tophaceous gout. No significant amounts of anechoic fluid are seen. This preaspiration image indicates that a “dry tap” can be expected. (B) Shows distension of the joint capsule by synovial tissue in a patient with rheumatoid arthritis. No anechoic free fluid is seen, again indicating a “dry tap.” In (C), hypoechoic synovial proliferation is seen lining the more hyperechoic joint capsule in a patient with inflammatory arthritis. Anechoic free fluid is seen that can be aspirated. Synovial tissue can be distinguished from synovial fluid by its often higher echogenicity and decreased compressibility. In inflammatory arthritis, Doppler signals may be detected in synovial tissue, but not in synovial fluid if the probe is kept steady. Fig. 18.2 When arranging a patient and equipment for a guided injection, it is helpful to place the patient and ultrasound screen so that the examiner can see the injection site and ultrasound image without the need to turn the head. This way the injection site can be observed throughout the procedure. Fig. 18.3 Parker-Pearson needle inserted in target tissue. The opening is marked by an open arrow. Suction of an attached syringe draws tissue into the needle. Fig. 18.4 The difference between palpation guidance and ultrasound guidance of arthrocenteses is illustrated. (A) With palpation guidance, the shortest route between skin and joint space is usually taken for the pass of the needle. (B) Ultrasound guidance using free-hand technique. The joint space is identified sonographically, and the needle is inserted at an angle so that it can be visualized deep to the probe.
Indications
Possible Diagnoses
Intralesional, Intraarticular, and Tendon Sheath Injections of Steroids and Other Therapeutic Agents
Adverse Effects
Contraindications
Preprocedural Evaluation
Room Setup, Patient Positioning, and Equipment
Setup and Positioning
Equipment
Preparation of Injection Equipment for Aspirations and Injections
Preparation of Skin
Technique
Shoulder
Positioning
Procedure
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree