Chapter 3 MUSCULOSKELETAL PERCUTANEOUS BIOPSY: Techniques and Tips
Image-guided percutaneous biopsy of bone and soft tissue lesions has become integral to modern medical care and is an essential part of the practice of musculoskeletal radiology. This technique has a number of advantages. For example, imaging guidance increases the likelihood of the biopsy being acquired from the lesion if it is small or from viable regions of the lesion if it is large. Imaging also facilitates avoidance of vessels, nerves, organs, and other sensitive structures. Conscious sedation (or in some cases just local anesthetic) may be used rather than the general anesthesia that is associated with surgery. Therefore, percutaneous biopsy can also reduce risk of complications. Percutaneous biopsy has been shown in numerous studies to be safe and effective. However, biopsy must be performed by a radiologist with knowledge of equipment, use of the imaging modalities and relevant anatomy, approaches and potential complications, and limitations of the procedure. This chapter outlines these issues but cannot substitute for practical experience.
EVALUATION OF THE PRE-BIOPSY IMAGING STUDIES
Conversely, the radiologist interpreting an exam should keep in mind that a report suggesting the presence of infection or tumor may obligate the surgeon to request biopsy, either surgical or percutaneous. If the lesion is clearly benign or noninfectious on imaging, an ambiguous report may be detrimental to the patient and could leave the radiologist at risk for litigation if a complication arises from the resultant invasive procedure. The two main situations in which this occurs are a bone lesion clearly demonstrating nonaggressive features and degenerative disk disease, which is often related to segmental instability. Ways to be more specific about these diagnoses are reviewed in Chapters 5 and 6.
EQUIPMENT
Guidance Modalities
An essential aspect to keep in mind when planning a biopsy is that the lesion should be visible on the guidance modality. Alternatively, if the lesion is extensive or infiltrative, the lesion itself need not be visible, just the region involved. Fluoroscopy has definite advantages over other modalities. For example, imaging is easily performed in real time. The limitation of projectional radiographic imaging is not a major one considering how easy it is to alter the angle craniocaudally or transversely to acquire a different viewpoint. Biopsies using fluoroscopy are often easier to schedule as well. However, the room and configuration of the fluoroscopy equipment (C-arm, fixed-image intensifier, angiography room) can create problems with access to the biopsy area and must be considered in advance. Many angiography units have a narrow work area, which can cause problems when a long biopsy needle is used. Also, some C-arms and angiography units cannot achieve the angulations needed for the desired approach.
Ultrasonography is very versatile and can also be used for localization of soft tissue lesions (Fig. 3-1). Obviously, because ultrasound does not visualize within bone, it generally cannot be used for bone biopsy localization except for superficial lesions or those with cortical breakthrough. Ultrasound with Doppler easily visualizes blood vessels and can improve the safety of the desired approach. Solid and vascular regions of soft tissue masses can also be accurately targeted. The needle passage can be directly visualized in real time rather than periodically after repositioning.
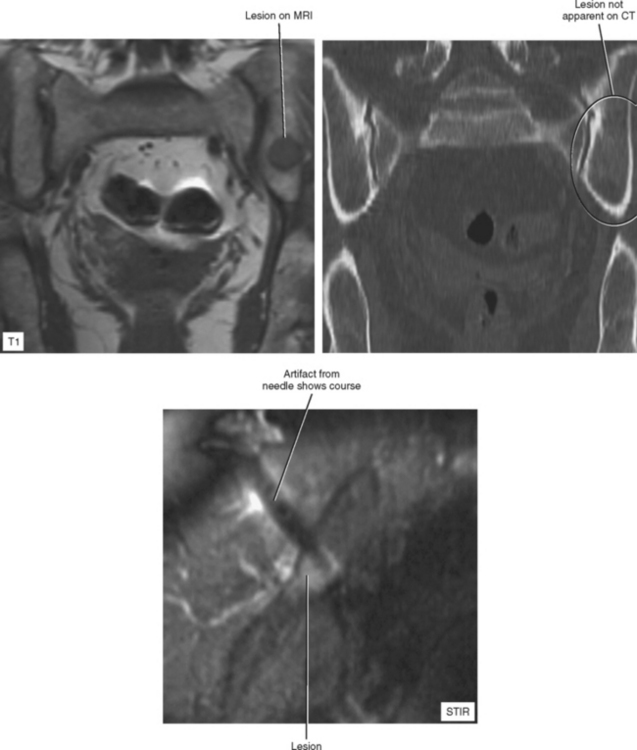
MRI is used in some centers for localization but requires special preparation (Fig. 3-2). If equipment is needed (e.g., to provide sedation and monitoring) it must be MRI-compatible (e.g., all components must be nonferromagnetic). In addition, needles must be MRI-compatible and made of a material that creates relatively little artifact so that the needle tract is well visualized with reference to surrounding anatomy. MRI can be useful for ablation because the destroyed tissue can be visualized (e.g., ice ball formation in cryoablation).
Needles
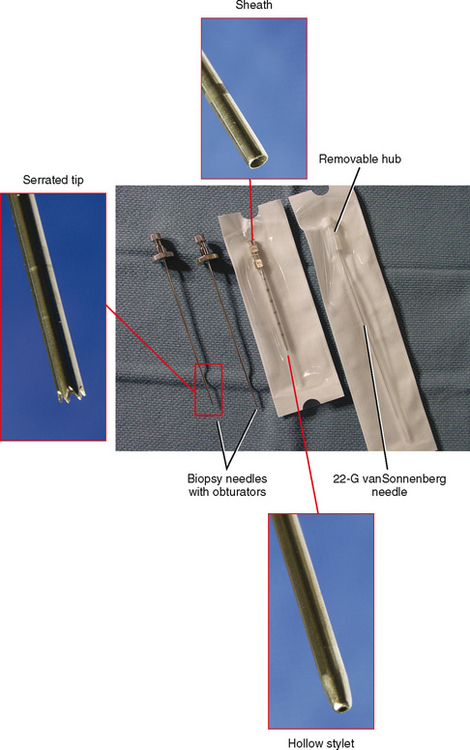
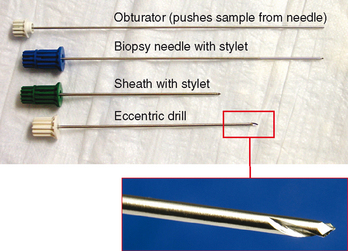
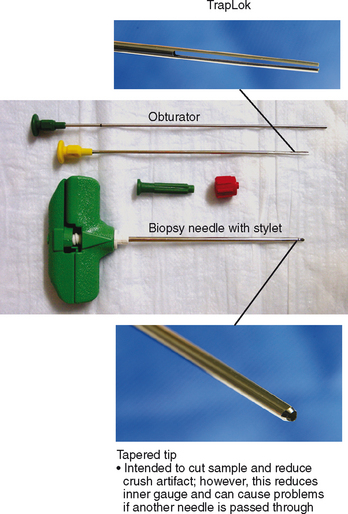
Coaxial Systems
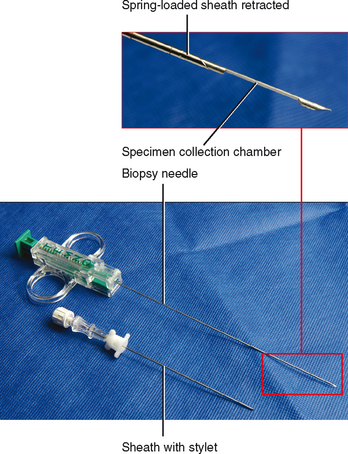
Coaxial systems are needles that have an outer sheath and an inner cutting needle and are intended for either soft tissue or bone (Figs. 3-3 and 3-4). The cutting needle extends a certain distance beyond the sheath. This is almost universally used in musculoskeletal biopsies because it requires only one localization/placement procedure to position the sheath/stylet at the margin of the lesion, after which multiple passes can be obtained. The only situation in which a non–coaxial system may be used is a very superficial lesion that is easy to localize and that is not near any vital structures (Figs. 3-5 and 3-6).
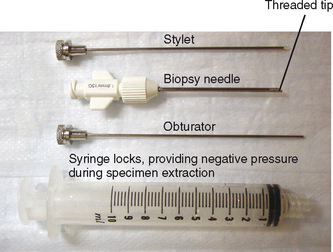
Soft Tissue Guns
Soft tissue guns collect a core of tissue unlike with fine aspiration needles (Fig. 3-7). They are larger gauge—typically 14 to 18 G. Rather than having a hollow cutting needle design, they incorporate a solid inner core with a recess near the tip. This portion of the needle is advanced into the lesion, after which an inner sheath “shoots” over it, cutting the tissue filling the recess. The system is then withdrawn from the outer sheath and the sample is collected. Therefore, two components are advanced in succession: the solid inner needle and the inner sheath. In some needles this is automated, triggered by a button that is pressed when the needle is in position. However, it is not always desirable to shoot the inner needle without feel or control. For example, if the lesion is near a vital structure or not as large as the “throw” of the needle, it is better to retain control of the first step. Some needles have a setting or alternate triggering mechanism that allows the radiologist to slowly advance the inner needle as far as desired; when in position, the sheath is triggered to advance.