Fig. 8.1
Fatigue fracture of the proximal tibial shaft in a 10-year-old girl who presented with left leg pain and no history of trauma. The initial frontal radiograph was normal (not shown) (a) Lateral radiograph shows subtle periostitis along the posterior aspect of the proximal left tibial shaft (arrow). Coronal (b) T1-W and (c) STIR MR images of the left leg show extensive ill-defined bone marrow edema in the proximal and mid-tibial shaft with associated periostitis and edema in the adjacent soft tissues. Subtle hypointense fracture line is seen on the coronal images (arrows). (d) Coronal contrast-enhanced fat-suppressed T1-W MR image shows prominent enhancement in this region (arrows). (e) Frontal radiograph of the left leg obtained 3 weeks later shows a healing stress fracture involving the posterior cortex of the proximal tibial shaft (arrows) (Courtesy of W. Mar, M.D.)
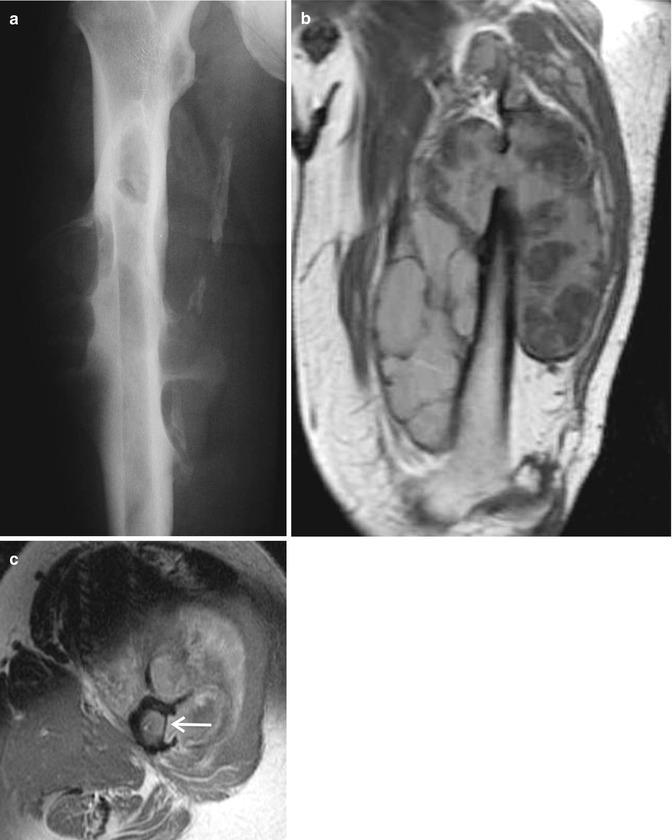
Fig. 8.2
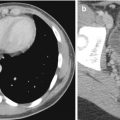
Chronic subperiosteal hematoma in a 59-year-old man with CHF under chronic anticoagulation therapy who presented with right thigh swelling. (a) Radiograph of the right femur shows bizarre periostitis around the femoral shaft with associated cortical scalloping and several osteolytic appearing lesions within the medullary bone. (b) Coronal T1-W and (c) axial PD-W MR images of the right thigh show a large lobulated heterogeneous periosteal mass with probable blood products encasing the right femoral shaft and causing pressure erosions of the outer cortex (arrow). No abnormal bone marrow signal was seen. Two-year stability of this lesion was documented by follow-up MRI
Postsurgical changes, such as sites of prior bone graft harvest, may be erroneously interpreted as possible malignant lesions. These lesions are often seen on pelvic computed tomography (CT) performed for unrelated reasons. Bone graft harvest sites (frequently in the posterior ilium or iliac crest) may mimic osteolytic metastatic disease, multiple myeloma, and atypical infections. It is not infrequent for these lesions to be painful for several months following the initial surgery/harvesting. On MRI and CT, these lesions may be associated with soft-tissue masses and/or insufficiency fractures (Ishii et al. 2010). Multiplanar reformats may reveal a characteristic rectangular shape (Fig. 8.3). Clinical history is confirmatory.
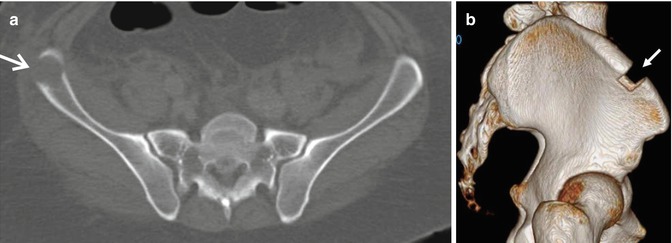
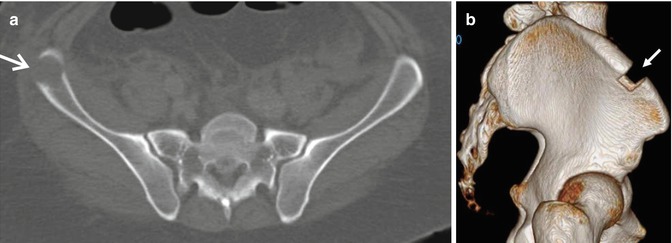
Fig. 8.3
Iliac bone graft donor sites as incidental findings on renal stone CT. (a) Axial CT image shows a bone graft harvest site in the right iliac crest (arrow) that mimics an osteolytic lesion due to partial volume averaging. (b) 3D reconstructed CT image shows the characteristic rectangular-shaped bone graft harvest site (arrow)
8.2.2 Benign Bone Marrow Patterns
Normal skeletal bone marrow contains “red” marrow in which hematopoietic elements predominate and “yellow” marrow with predominantly fatty elements. Conversion of red to yellow marrow begins in the terminal phalanges shortly before birth and progresses in a centripetal direction. The adult pattern of marrow distribution is reached by the age of 25 years, with recognized gender-dependent variations (Fig. 8.4). In conditions with increased hematopoietic demand, marrow reconversion occurs in a reverse order of physiologic marrow conversion. Hematopoietic marrow hyperplasia of the vertebral marrow typically demonstrates low signal intensity on spin-echo (SE) T1-weighted images (lower than adjacent disc or skeletal muscle), low signal intensity on SE T2-weighted images, intermediate signal on fat-suppressed proton density (PD)-W images and moderate enhancement on post-gadolinium T1-W images. In the appendicular skeleton, regenerating red marrow nodules may simulate metastatic disease. Differentiation of benign hematopoietic marrow hyperplasia from diffuse marrow infiltration remains difficult. While knowledge of the typical distribution of residual red marrow in adults and its signal characteristics will often allow the correct diagnosis, problem cases may require iliac crest biopsy (Vande Berg et al. 1998a, b, 2005, 2009; Hanrahan and Shah 2011; Shah and Hanrahan 2011).
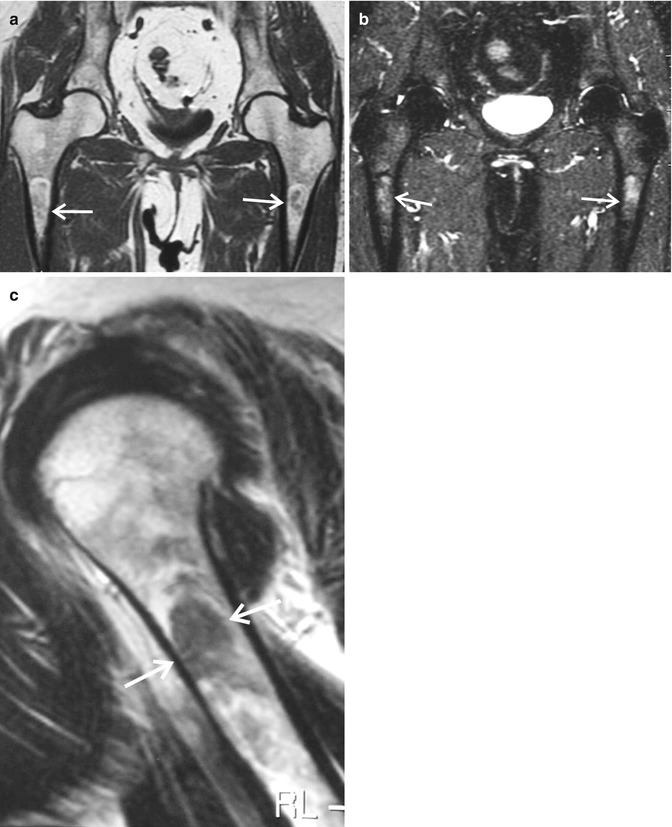
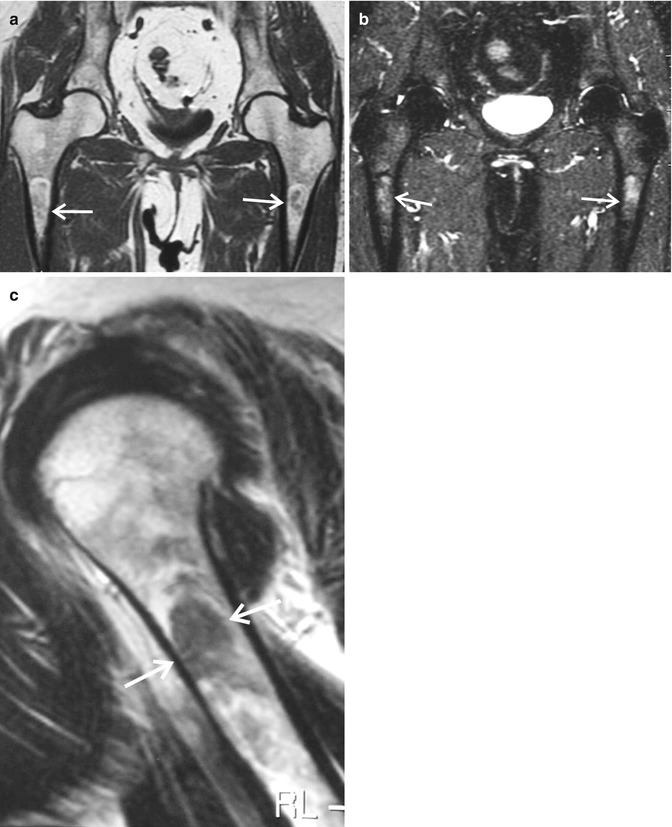
Fig. 8.4
Normal variant bone marrow pattern “bullet lesion” in proximal femurs and humerus (possibly related to local encystification of marrow or focal marrow reconversion). These lesions should not be mistaken for metastatic disease. Coronal (a) T1-W and (b) STIR MR images of the pelvis/proximal femurs and (c) sagittal T1-W MR image of the proximal humerus in a middle-aged woman show normal bone marrow pattern variant in the proximal shafts of these long bones (arrows)
Patchy areas of decreased T1 signal intensity and increased signal on the fluid-sensitive sequences in the feet and ankles of children are frequently observed and represent a normal variant (possibly residual hematopoietic marrow) and should not be mistaken for pathology/marrow infiltrative process (Fig. 8.5). These findings typically resolve by age 16 years (Pal et al. 1999; Shabshin et al. 2006). FDG–PET may be false positive in cancer patients who have received recent bone marrow-stimulating agents for treatment of leukopenia (Fletcher et al. 1993; Kazama et al. 2005; Naples et al. 2007; Morooka et al. 2008), as well as in patients with acute compression fractures and recent vertebroplasty (Kuo and Cheng 2005; Bredella et al. 2008) (Figs. 8.6 and 8.7). Clinical history and correlation with radiographs in acute compression fractures or vertebroplasty should allow diagnosis. If possible, PET imaging should not be performed in the first three weeks following therapy with marrow-stimulating agents.
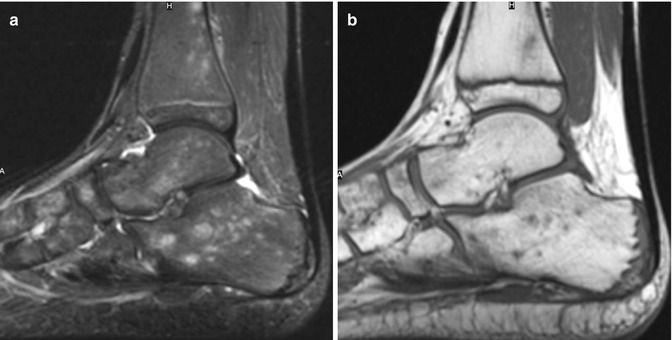
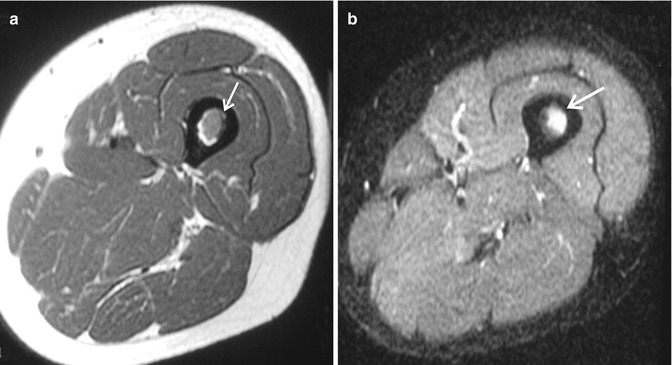


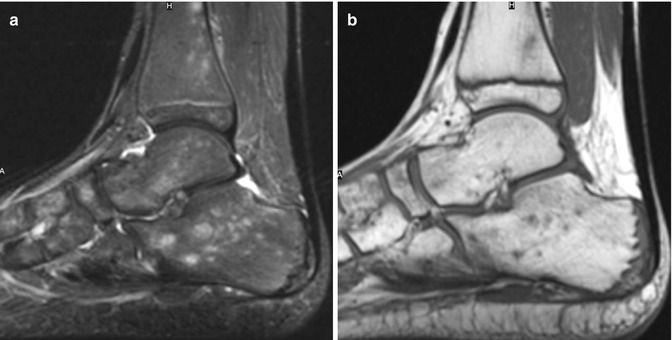
Fig. 8.5
Normal bone marrow pattern variant in an 11-year-old boy with hypereosinophilia syndrome and right ankle pain. Normal bone marrow pattern variant in children may be mistaken for marrow infiltrative process. (a) Sagittal STIR MR image shows multiple small focal areas of hyperintensity in multiple bones which are hypointense on the corresponding (b) sagittal T1-W MR image
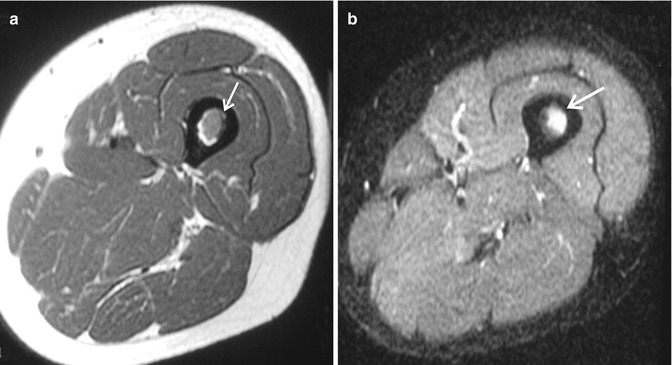

Fig. 8.6
Granulocyte-stimulating factor (GSF)-induced bone marrow conversion in two different patients that can mimic metastatic disease. (a, b) 29-year-old man with history of clear cell sarcoma of foot status post-below the knee amputation, with GSF-induced bone marrow conversion. Axial (a) T1-W and (b) fat-suppressed T2-W MR image of the distal thigh shows a T1-iso to hypointense and T2-hyperintense lesion (arrow). (c) 55-year-old man with recurrent rectal adenocarcinoma, status post-pelvic radiation. The patient received GSF 5 days prior to PET scan causing bone marrow reconversion. Sagittal PET–CT image shows diffuse shift of FDG tracer into the marrow of the axial and appendicular skeleton. Subtle lesions would be obscured, and quantitative measurements (SUVs) would be unreliable for bony and soft-tissue lesions. We recommend waiting three weeks post-GSF, when possible, to allow for resolution of hematopoietic stimulation (Courtesy of Fabio Almeida M.D.)

Fig. 8.7
Vertebroplasty in a 68-year-old woman with non-Hodgkin lymphoma, treated by chemotherapy and radiation to the abdomen and L1 vertebroplasty about 1 month prior. Sagittal PET–CT image shows increased FDG uptake in the L1 vertebroplasty site consistent with post-procedure healing and inflammation (upper arrow). Increased uptake is also seen throughout the body of L3 vertebral body (lower solid head arrow) concerning for early/evolving compression fracture and would be indistinguishable from lymphoma involvement. The lack of lesions elsewhere is supportive of diagnosis of fracture (Courtesy of Fabio Almeida M.D.)
8.2.3 Benign Tumors and Tumor-Like Conditions
8.2.3.1 Fibrous Dysplasia
Fibrous dysplasia (FD) is a noninherited bone disease in which abnormal differentiation of osteoblasts leads to replacement of normal marrow and cancellous bone by immature bone and fibrous stroma. It is usually an incidental imaging finding, generally not requiring further investigation. This disease is categorized as either monostotic or polyostotic and may occur as a component of McCune–Albright syndrome or the rare Mazabraud syndrome. Malignant degeneration is rare. Classically, on radiographs, FD lesions are intramedullary, expansile, and well defined with varying degrees of hazy density with a ground-glass quality, although some may be almost completely radiolucent or sclerotic. Endosteal scalloping may be present, but a smooth cortical contour is typically maintained. The lesions usually show nonspecific increased radiotracer uptake on bone scans. The MRI characteristics of FD are variable, typically showing signal intensity that is intermediate to low on T1-weighted images and intermediate to high on T2-weighted images, with heterogeneous enhancement after administration of gadolinium-based contrast agent (Fitzpatrick et al. 2004; Remotti and Feldman 2012). Single cases have been reported in which FD is present in patients undergoing FDG–PET scanning for oncological reasons, and FD can appear with and without increased FDG uptake (Stegger et al. 2007). Biopsy and surgical removal of FD lesions is generally reserved for equivocal cases or those with complications (Figs. 8.8 and 8.9).
Fig. 8.8
Asymptomatic polyostotic fibrous dysplasia in a 65-year-old woman with a known history of breast carcinoma. She was otherwise asymptomatic and had a PET–CT (not shown) performed which showed multiple foci of skeletal radiotracer uptake. (a) Coronal reconstructed CT image of the abdomen and pelvis shows several well-defined expansile osteolytic lesions involving multiple ribs and the axial skeleton (arrows). Axial (b) T2-W and (c) GRE T1-W MR images of the abdomen show a large expansile heterogeneous hypointense lesion involving the lower rib with a mass effect to the right kidney and an additional less expansile lesion of similar signal in the adjacent rib (arrows). Diagnosis was confirmed by biopsies of the rib and sacral lesions
Fig. 8.9
Symptomatic monostotic fibrous dysplasia in a 25-year-old man who presented with chronic right hip pain. (a) Radiograph of the right hip shows an expansile lobulated predominantly osteolytic lesion of the right ischium suggestive of fibrous dysplasia, possibly with an associated aneurysmal bone cyst (arrows). (b) Axial CT image of the lower pelvis shows the osteolytic lesion in the right ischium with marked cortical thinning/breakthrough of the medial ischial wall worrisome for malignancy or atypical infection (arrows). Diagnosis of fibrous dysplasia was confirmed by biopsy
8.2.3.2 Langerhans Cell Histiocytosis
Langerhans cell histiocytosis (LCH), formerly known as histiocytosis X, is a rare group of disorders of unknown etiology which can occur in any age group with a wide spectrum of clinical presentation causing local or systemic effects. The hallmark of LCH is the proliferation and accumulation of a specific histiocyte, the Langerhans cell. LCH includes three classic clinical syndromes that are considered to be clinical variations of the same disease: eosinophilic granuloma, Hand–Schuller–Christian disease, and Letterer–Siwe disease. Eosinophilic granuloma, the most common form, is isolated to the bone, often monostotic, with potential involvement of any bone. Radiographically, early-phase lesions are osteolytic with an aggressive appearance, poorly defined margins, variable aggressive-appearing periostitis, and difficult to differentiate from malignancy, such as Ewing sarcoma, lymphoma, leukemia and metastasis, osteoblastoma, or atypical infection. In the flat bones and in the late phase, the lesions are typically better defined and may have sclerotic margins suggestive of spontaneous healing.
CT and MRI are useful in providing detailed cross-sectional anatomic detail of the involved bone, including the bone marrow and the adjacent soft tissues (Fig. 8.10), and bone scintiscans are useful in the detection of multifocal involvement. On MRI, the lesions typically show decreased signal on T1-weighted images, increased signal on fluid-sensitive sequences, and marked enhancement on contrast-enhanced fat-suppressed T1-weighted sequences which decreases with healing. Prominent perilesional edema may be present. FDG–PET shows radiotracer uptake in active lesions as opposed to healed lesions. Patients with skeletal LCH may be asymptomatic or present with pain, swelling, and soft-tissue mass. Biopsy is frequently needed for diagnosis. Although the natural history for most lesions is of gradual healing, curettage and bone grafting are sometimes performed to accelerate the healing process. Internal fixation for stability is occasionally necessary. Chemotherapy is used for multisystemic disease, and radiotherapy is no longer used (Hoover et al. 2007; Arkader et al. 2009; Remotti and Feldman 2012).
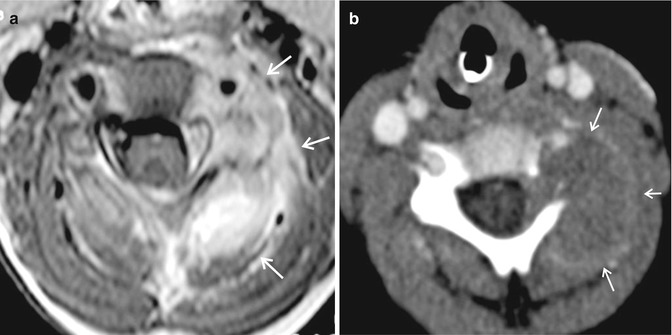
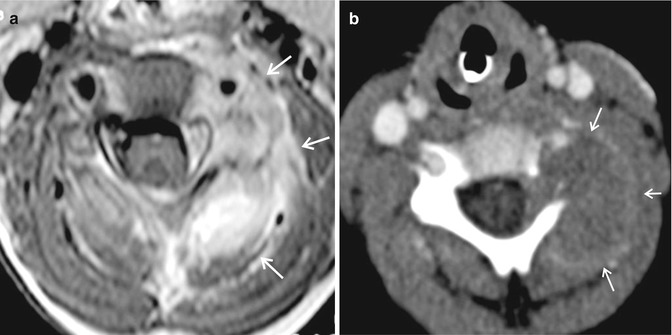
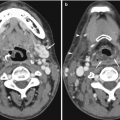
Fig. 8.10
Eosinophilic granuloma of C4 vertebra in a 4-year-old child who presented with left-sided neck pain. Radiographs were normal (not shown). (a) Axial contrast-enhanced fat-suppressed T1-W MR image of the neck shows an avidly enhancing lesion at the left side of the C4 vertebra with involvement of the vertebral foramen and posterior elements. There is extension into the epidural space and a large soft-tissue component with associated edema (arrows). (b) Axial CT image taken at the same level shows a large destructive rim-enhancing lesion (arrows). Diagnosis of eosinophilic granuloma was confirmed by biopsy
8.2.3.3 Enchondroma
Enchondroma is a common benign bone tumor which is characterized by formation of abundant mature hyaline cartilage. This tumor can be seen in any age group. Any bone can be involved and majority of the lesions are asymptomatic. Radiographs show central, well-defined, possibly expansile osteolytic lesions with variable endosteal scalloping. Periosteal reaction or frank cortical breakthrough is an ominous sign. Chondroid matrix calcifications may be seen. When noncalcified, lesions are often radiographically occult and identified first on MRI, where they are characterized by lobulated T1-hypointense signal, lobulated hyperintense signal on fluid-sensitive sequences, and variable enhancement on the contrast-enhanced T1-weighted sequences (Fig. 8.11). On bone scintigraphy, enchondromas typically show normal or only slightly increased radiotracer uptake. Markedly increased activity of enchondroma with pain is most often associated with pathologic fracture or malignant degeneration (Murphey et al. 1998; Azouz et al. 2005; Hommadi et al. 2009; Wootton-Gorges 2009). FDG–PET may help in distinguishing benign from malignant chondroid matrix lesions (Kim et al. 2003).


Fig. 8.11
Enchondroma of the acromion in a 14-year-old boy who presented with right shoulder pain. (a) Radiograph shows a nonspecific osteolytic lesion with permeative appearance in the acromion (arrows). (b) Axial fat-suppressed PD-W MR image shows a lobulated, minimally expansile, well-defined hyperintense lesion with endosteal scalloping involving the acromion (arrows). (c) The lesion shows intermediate signal intensity on the sagittal T1-W MR image (arrows)
8.2.3.4 Non-ossifying Fibroma
Non-ossifying fibroma (NOF) (or fibroxanthoma) is a common benign tumor seen in children and adolescents that has typical radiographic and MRI characteristics. On radiographs, these lesions are usually seen in the diametaphyseal regions; they are eccentrically located and show sclerotic margins. They appear lobulated and radiolucent, become sclerotic with healing, and may resolve (Kim et al. 2003; Stacy and Dixon 2007; Remotti and Feldman 2012). When PET or bone scintigraphy reveal metabolically active osseous abnormalities in children who are at risk for bone metastases, benign fibro-osseous lesions should also be considered in the differential diagnosis, and correlation with radiographs should be performed (Feldman et al. 2005). Fractures (stress or acute) through NOFs are particularly confusing and may be mistaken for malignancy on MRI. Radiographic findings are typically reassuring (Goodin et al. 2006) (Fig. 8.12).


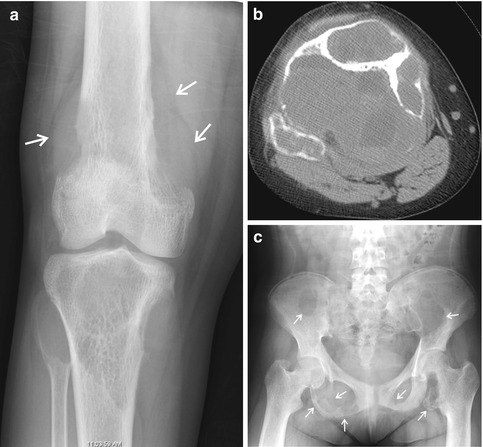
Fig. 8.12
Non-ossifying fibroma of the left distal femoral diametaphysis with an associated stress fracture in an 18-year-old girl, active in sports, who presented with distal left thigh pain. (a) Coronal STIR MR image shows an abnormal hyperintense lesion involving the left distal femoral diametaphysis (arrows) with foci of decreased signal at the medial aspect of the lesion. The lesion shows hypointense signal on the (b) axial T1-W MR image and hyperintense signal on the (c) axial fat-suppressed T2-W MR image, with associated periostitis at the posterior aspect of the lesion (arrows). The MRI findings may be mistaken for malignancy. Subsequently performed (d) frontal radiograph shows an eccentrically located geographic lesion at the posterior aspect of the distal femoral diametaphysis with typical radiographic findings of a non-ossifying fibroma (arrows). (e) Lateral radiograph shows a subtle pathologic fracture (arrow)
8.2.3.5 Benign Radiation-Induced Changes
Advances in oncological treatments have resulted in improved survival rates, and it is not unusual to see the late effects of radiotherapy in both pediatric and skeletally mature cancer patients (Sakamoto et al. 2008). It is important to recognize the skeletal complications of radiotherapy, as they can cause diagnostic problems, and some are associated with significant morbidity. The effects of radiation on mature bone result in weakening and vary according to the absorbed dose and other factors, such as beam energy and fractionation. The benign radiographic changes constitute a spectrum from mild osteopenia, approximately 1 year after treatment, to osteonecrosis, reflecting bone atrophy, attempted repair, and possibly late vascular changes. On MRI, benign radiation-induced changes may mimic infection and malignancy such as multiple myeloma, recurrent tumor, and metastatic disease (Williams and Davies 2006) (Fig. 8.13). In equivocal cases, tissue diagnosis may be required.
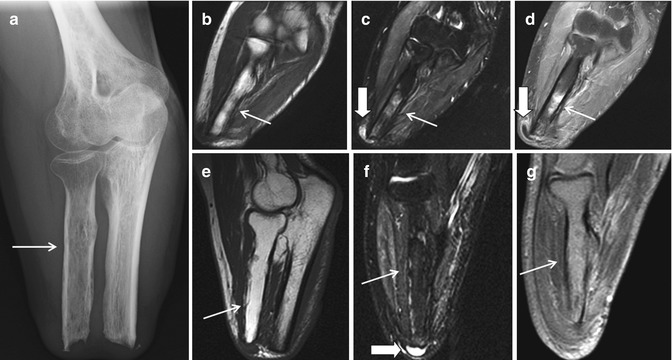
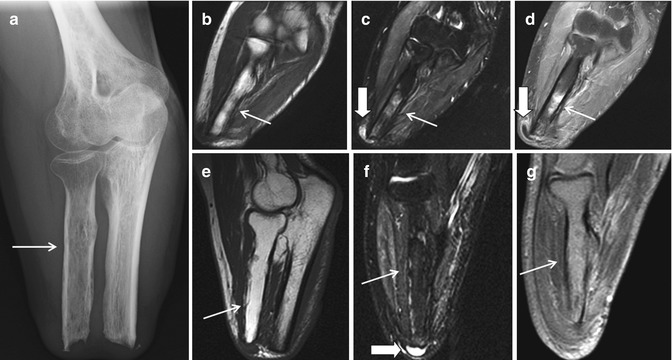
Fig. 8.13
Radiation-induced osteopenia in a 25-year-old man who had a below-elbow amputation for high-grade soft-tissue sarcoma of the forearm. (a) After receiving high-dose radiation to his stump, radiograph shows osteopenia, most apparent in the radius (arrow). Subsequent coronal (b) T1-W, (c) STIR, and (d) contrast-enhanced fat-suppressed T1-W MR images show a patchy area of T1-hypointense and T2-hyperintense signal that is enhanced (arrows). A year later, the bone marrow signal was normal on repeat sagittal (e) T1-W, (f) STIR, and (g) contrast-enhanced fat-suppressed T1-W MR images (arrows). The patient also had a stump bursa (b, c, f, thick block arrows)
8.2.4 Osteomyelitis
The imaging appearance of osteomyelitis may mimic malignancy, most often Ewing sarcoma, osteosarcoma, or lymphoma. Clinical history and laboratory findings are frequently reassuring. On MRI, contrast-enhanced fat-suppressed T1-weighted sequences depict rim-enhancing intraosseous, subperiosteal, and soft-tissue abscesses (Fig. 8.14). If blood cultures are negative, bone aspirate/biopsy may yield a diagnosis (Caraway et al. 2003; Tong et al. 2003; Ollivier et al. 2006; Gould et al. 2007; Sheppard and Switlick 2008; Shimose et al. 2008). Recently, the penumbra sign, a higher signal intensity feature of the thin layer of granulation tissue which lines the abscess cavity on T1-weighted MR images, has been reported to be helpful for discriminating subacute osteomyelitis (Witte et al. 2000). Chronic recurrent multifocal osteomyelitis (McGuinness et al. 2007) and multifocal atypical infections may mimic metastatic disease (Dalinka et al. 1971; Wipff et al. 2011) (Fig. 8.15).

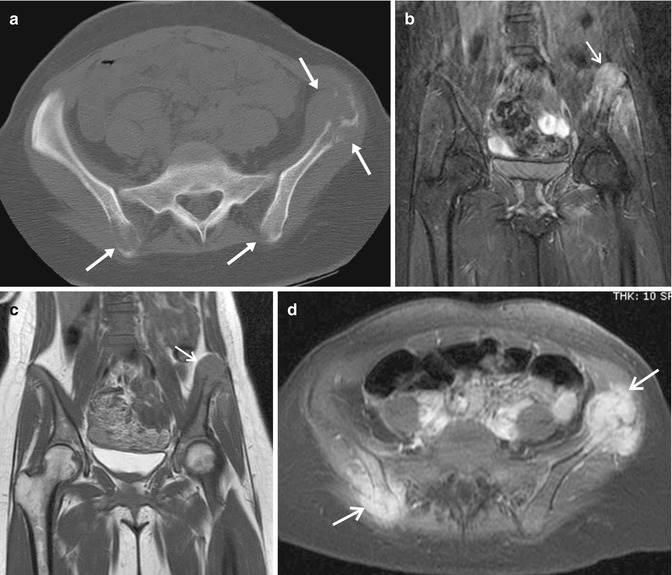

Fig. 8.14
15-year-old boy with neglected osteomyelitis (S. aureus) of the right distal femur. Initial (a) frontal and (b) lateral radiographs show mottled appearance of the distal femoral diametaphysis with associated aggressive-appearing periostitis (arrows). The preliminary diagnosis was possible Ewing sarcoma. One month later, after surgical debridement and initiation of intravenous antibiotics, repeat (c) frontal and (d) lateral radiographs show mixed sclerotic and osteolytic appearance of the femoral lesion with associated extensive periostitis, consistent with known chronic osteomyelitis, but mimicking osteosarcoma. (e) Coronal STIR MR image shows a hyperintense lesion involving the mid- and distal femur with extension into the epiphysis and associated soft-tissue component which mimics malignancy (arrows). (f) Sagittal contrast-enhanced fat-suppressed T1-W MR image shows a large rim-enhancing intraosseous abscess with a heterogeneously enhancing soft-tissue component (arrows). The diagnosis was confirmed by blood cultures and biopsy/aspiration
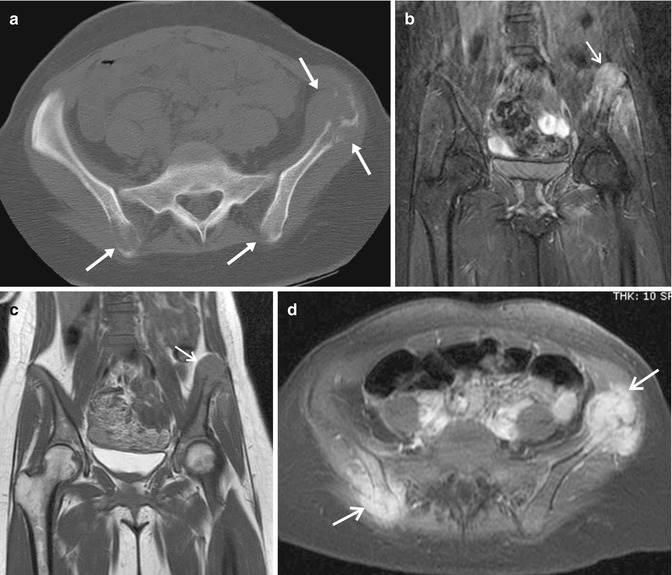
Fig. 8.15
20-year-old African–American woman with disseminated coccidioidomycosis infection that can mimic metastatic disease. (a) Axial CT image of the pelvis shows multiple destructive osteolytic lesions in the pelvic bones (arrows). (b) Coronal STIR MR image shows a hyperintense lesion in the left iliac bone with associated soft-tissue component (arrow). (c) The lesion is of intermediate signal intensity on the coronal T1-W MR image (arrow). (d) Axial contrast-enhanced fat-suppressed T1-W MR image shows marked enhancement of the right posterior iliac bone and left anterior iliac bone lesions (arrows). Coccidioidomycosis infection is known to be prone to involvement of bony protuberances. The diagnosis was made by serology and biopsy
8.2.5 Rheumatologic Diseases
Imaging findings related to inflammatory, metabolic, or degenerative arthritis sometimes may mimic malignancy (Stacy and Dixon 2007). Distended synovial bursae may cause pressure erosions in the adjacent bones, occasionally mimicking osteolytic/destructive lesions on radiographs. Clinical history, associated findings in adjacent or other skeletal structures, and MRI should clarify the diagnosis (Fig. 8.16). Literature review revealed a few cases of inflamed bicipitoradial bursa mimicking malignant tumor on clinical examination, MRI, bone scintigraphy, and CT that required tissue diagnosis (Kheireddine et al. 2008; Taljanovic and Adam 2011).
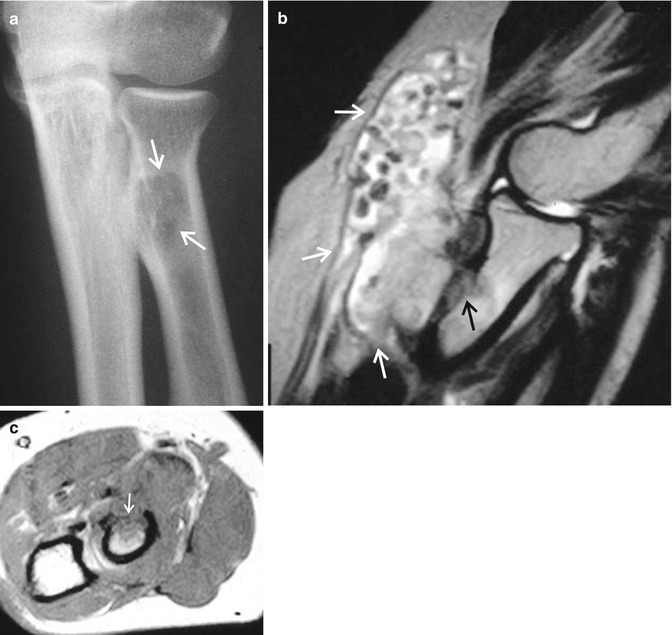
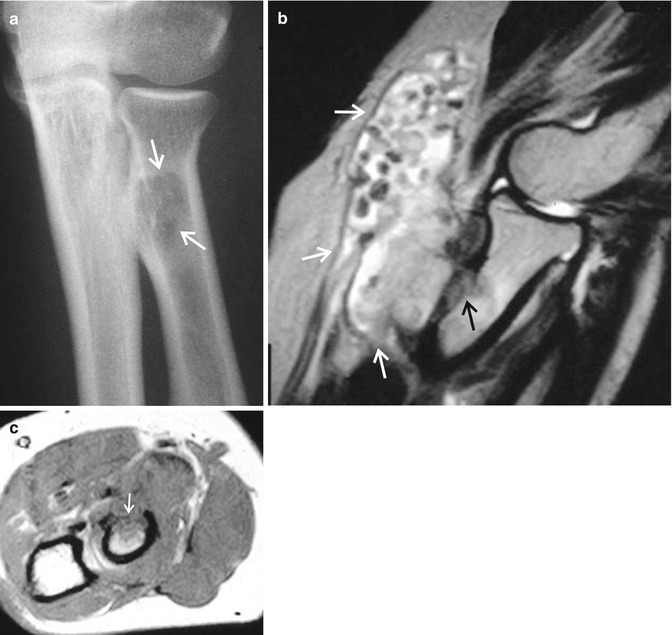
Fig. 8.16
Bicipitoradial bursitis with rice bodies causing erosion of the radial tuberosity in a patient with rheumatoid arthritis who presented with a slowly progressing painful antecubital swelling/mass. (a) Frontal radiograph of the right elbow shows a lucent lesion in the region of the radial tuberosity, which may mimic metastatic disease or a primary bone tumor (arrows). (b) Sagittal fat-suppressed T2-W MR image shows a distended bicipitoradial bursa containing multiple rice bodies (arrows). (c) Axial T1-W MR image shows an abnormal area of hypointense signal in the anterior aspect of the radial tuberosity with an associated cortical breakthrough, consistent with erosion (arrow) caused by the adjacent bicipitoradial bursa
Calcium hydroxyapatite deposition disease (HADD) frequently causes increased radiotracer uptake on bone scintigraphy and may be mistaken for primary malignancy or metastatic disease (Kannangara et al. 2002; Kerimoglu et al. 2007). MRI may also be confusing, with findings of bone marrow edema, associated erosions, and soft-tissue edema (Flemming et al. 2003; Kerimoglu et al. 2007). Associated calcifications are not always clearly visible on MRI. Radiographs and/or CT should aid to correct diagnosis (Figs. 8.17 and 8.18). Intraosseous gouty tophi with soft-tissue extension may mimic malignancy or atypical infection on MRI (Liu et al. 1996; Bui-Mansfield and Moak 2005). Correlation with clinical history, laboratory findings, and radiographs usually allows for the correct diagnosis (Fig. 8.19).

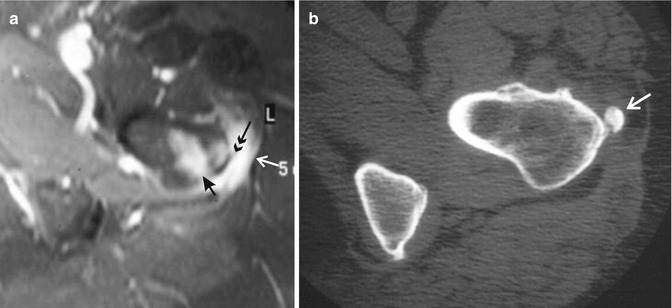


Fig. 8.17
(a–d) Calcium hydroxyapatite deposition disease (HADD) in a 60-year-old woman with a history of breast carcinoma. (a) anterior view and (b) posterior view Tc-99m diphosphonate bone scintiscans of the pelvis show a focal area of increased radiotracer uptake at the posterior aspect of the proximal right femoral diaphysis which was read as probable metastatic disease (arrows). (c) Radiograph and (d) sagittal reconstructed CT image show a conglomerate of calcifications at the gluteus maximus tendon attachment site, consistent with HADD (arrows)
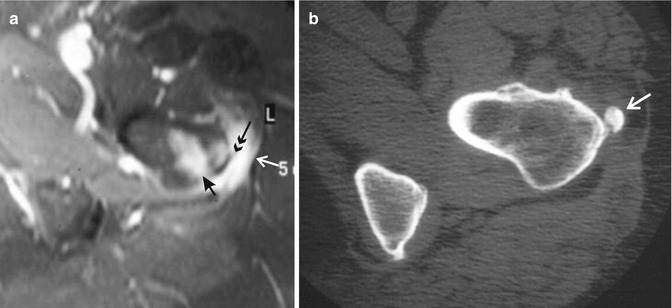
Fig. 8.18
Calcium hydroxyapatite deposition disease (HADD) in a 60-year-old woman with a history of breast carcinoma and left hip and thigh pain, with a positive bone scintiscan in the region of the left greater trochanter, suspicious for metastatic disease. (a) Axial fat-suppressed T2-W MR image of the left hip/proximal femur shows a hyperintense lesion in the greater trochanter/intertrochanteric region with associated cortical discontinuity (short black arrow) and adjacent soft-tissue edema (white arrow). A faint punctuate area of hypointense signal (calcification) adjacent to the greater trochanter (double black arrow) is barely seen. (b) Subsequent axial CT image of the same region clearly shows a focal calcification adjacent to the greater trochanter, consistent with HADD of the gluteus maximus tendon (arrow)

Fig. 8.19
Gouty arthritis of the proximal interphalangeal joint of the fifth toe. Sagittal (a) T1-W and (b) STIR MR images show an associated large soft-tissue component (tophus) which may mimic malignancy. (c) Radiograph of the fifth toe clearly shows findings of gouty arthritis of the fifth toe proximal interphalangeal joint (arrows) with associated dense periarticular soft-tissue swelling
Large subchondral geodes and intraosseous ganglion cysts are not uncommon in patients with advanced osteoarthritis and may mimic giant cell tumors typically seen in young adults. On T1-weighted images, these lesions show low signal intensity suspicious for bone marrow replacement. Fluid-sensitive sequences (showing geographic region of high signal intensity) and contrast-enhanced fat-suppressed T1-weighted MR images (demonstrating thin rim and septal enhancement) are typically reassuring (Hughes et al. 2005; Ollivier et al. 2006) (Fig. 8.20).
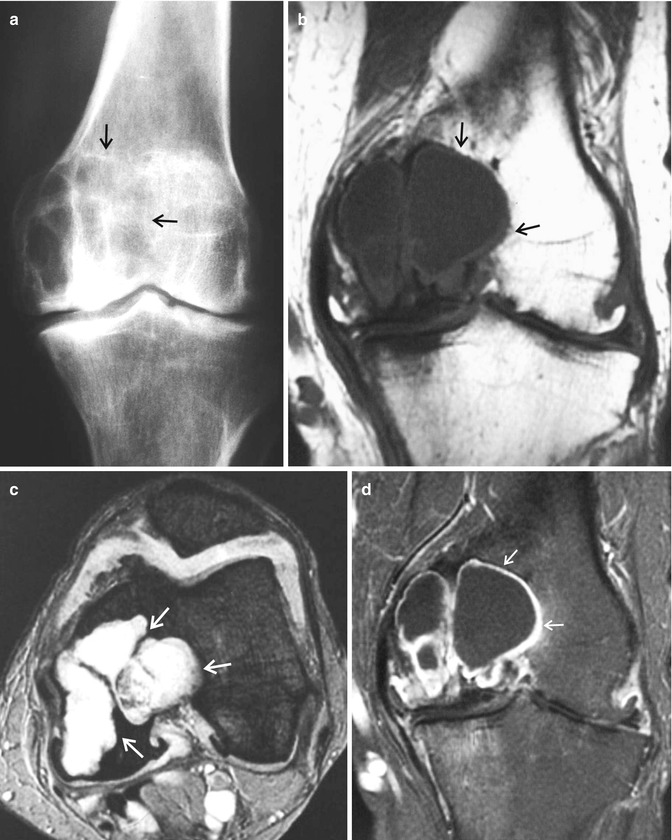
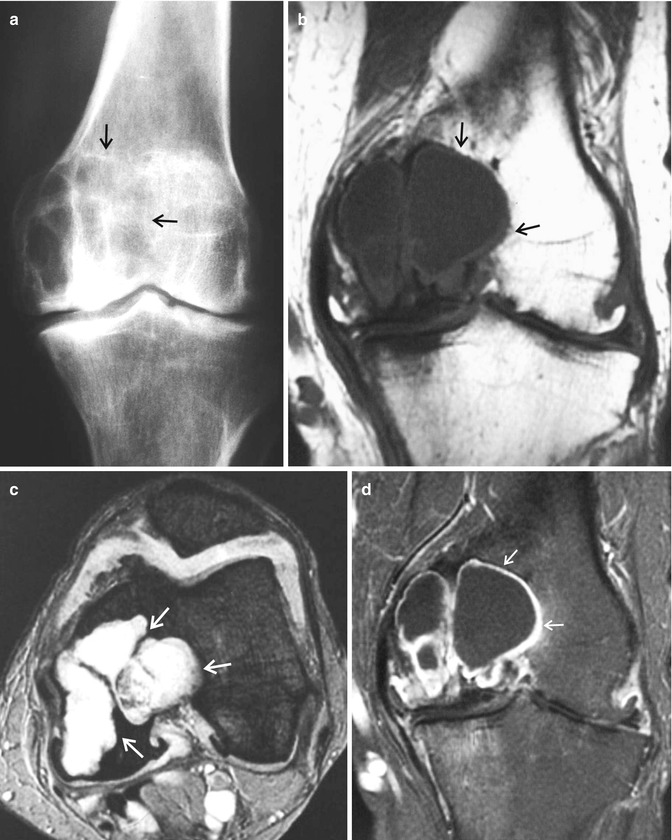
Fig. 8.20
Large geode in a 75-year-old man with advanced painful left knee osteoarthritis. (a) Radiograph and (b) coronal T1-W MR image appearances may mimic those of a giant cell tumor or metastasis (arrows). (c) Axial fat-suppressed T2-W MR image shows a geographic multiloculated hyperintense lesion involving the medial femoral condyle, suggestive of a large geode or an intraosseous ganglion cyst (arrows). (d) Coronal contrast-enhanced fat-suppressed T1-W MR image shows the characteristic thin rim and septal enhancement of the lesion (arrows)
8.2.6 Miscellaneous
8.2.6.1 Paget Disease
Paget disease affects elderly and middle-aged patients and is characterized by abnormal osteoclastic and osteoblastic activity. In the early “active” phase, osteolytic lesions are observed on radiographs. Involved long bones may have a characteristic “blade of grass” appearance. In the late “inactive” phase, cortical and trabecular thickening is seen. Characteristics of both phases may be present simultaneously. CT imaging parallels the radiographic findings. MRI findings are variable, ranging from normal to abnormal with nonspecific foci of decreased signal intensity on the T1-weighted sequences and increased signal on the fluid-sensitive sequences that can mimic metastatic disease or multiple myeloma. Increased radiotracer uptake is observed on bone scintigraphy (Stacy and Dixon 2007; Marra et al. 2008) (Figs. 8.21 and 8.22).
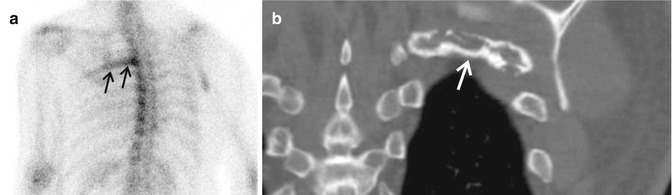

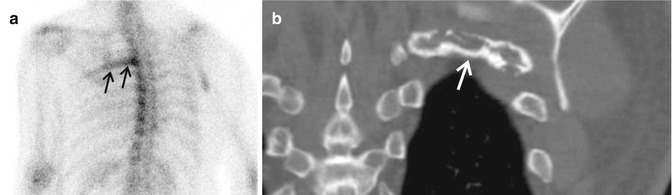
Fig. 8.21
Paget disease of the rib in a 76-year-old asymptomatic man with a history of prostate carcinoma and normal PSA. (a) Tc-99m diphosphonate bone scintiscan shows increased radiotracer uptake in a single posterior left rib (arrows). (b) Coronal reconstructed CT image shows cortical thickening with mild expansion of the same rib, suggestive of Paget disease (arrow). Follow-up yearly CT studies over the next 5 years showed no change in appearance of the lesion. Retrospective analysis of the patient’s old chest radiographs revealed that the lesion was present but was not described 45 years ago

Fig. 8.22
Osteolytic phase of Paget disease in a long bone. Radiograph shows the V-shaped, so-called blade of grass, sign, which may be mistaken for metastatic disease or multiple myeloma (arrows)
8.2.6.2 Melorheostosis
Melorheostosis is an uncommon mesenchymal dysplasia that affects the appendicular or (rarely) axial skeleton and may have soft-tissue manifestations. Unilateral well-marginated undulating zones of cortical hyperostosis with a “dripping candle wax” appearance, with or without associated soft-tissue masses, occur in the distribution of the sclerotomes (Judkiewicz et al. 2001; Nasu et al. 2002; Smith et al. 2002) (Fig. 8.23). Mineralized or nonmineralized soft-tissue masses adjacent to sites of osseous melorheostosis should be recognized as another manifestation of this disease, as opposed to a more ominous finding, making biopsy unwarranted (Smith et al. 2002). The lesions typically show increased radiotracer uptake on bone scintigraphy (Chanda and Millner 2007; Izadyar and Gholamrezanezhad 2012).
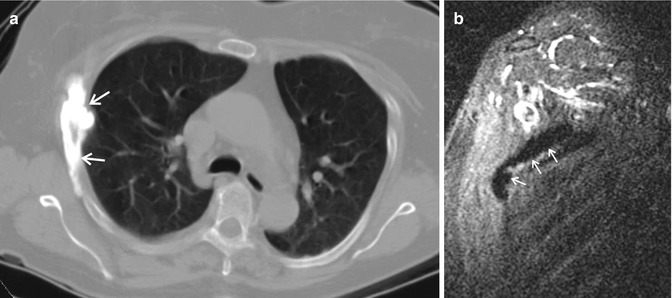
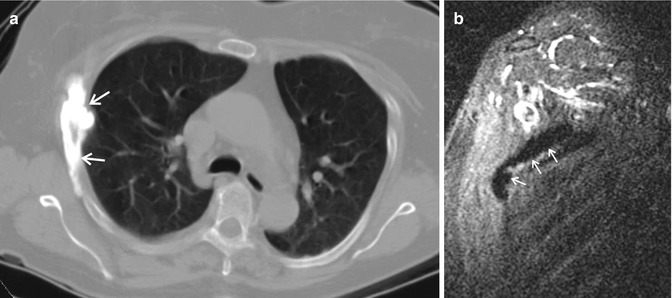
Fig. 8.23
Melorheostosis of the rib in a 69-year-old woman may mimic osteoblastic metastatic disease. This was an incidental finding on a trauma CT which prompted an unnecessary MRI study. (a) Axial CT image of the chest shows a typical “dripping candle wax” sclerotic lesion along the right thoracic rib, characteristic for melorheostosis (arrows). (b) The lesion showed hypointense signal on the coronal oblique STIR MR image (arrows)
8.2.6.3 Neuropathic Joint
Neuropathic joint or Charcot arthropathy typically does not mimic malignancy. As shown in this chapter, however, proliferative Charcot arthropathy may occasionally resemble an osteosarcoma (Fig. 8.24).
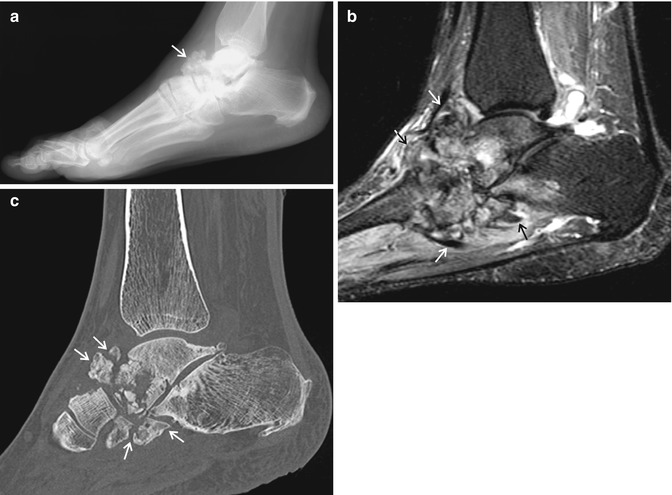
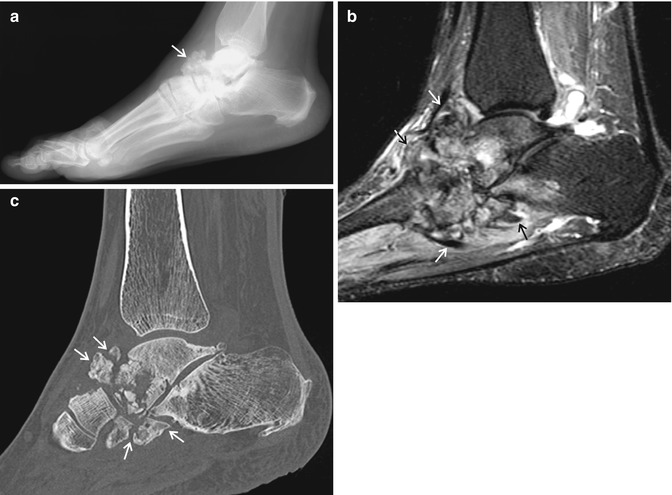
Fig. 8.24
Charcot arthropathy in a 37-year-old diabetic woman. (a) Lateral radiograph shows appearances of neuropathic arthropathy which resemble those of an osteosarcoma (arrow). (b) Sagittal STIR MR image shows destructive changes with intermediate increased signal intensity centered in the midfoot (arrows), typical of Charcot arthropathy. (c) Sagittal reconstructed CT image confirms the diagnosis of Charcot arthropathy (arrows)
8.2.6.4 Brown Tumor
Brown tumors of primary and secondary hyperparathyroidism are now uncommon, with typical earlier clinical diagnosis and effective treatment of hyperparathyroidism. However, brown tumors remain a consideration in the evaluation of patients presenting with multiple lucent or tumor-like lesions on radiographs, CT, MRI, and bone scintigraphy, in which no primary neoplasm is known (Tigges et al. 1995; Meydan et al. 2006; Ollivier et al. 2006; Kirk et al. 2009; Sonoda et al. 2011) (Fig. 8.25). Clinical, laboratory, radiographic, and histologic investigations can lead to a correct diagnosis.