Fig. 18.1
US illustrations show improved demonstration of details in small structures with transvaginal US examination. (a) Transabdominal US image shows a small postmenopausal uterus (within calipers). (b) Transvaginal US image shows an endometrial tumor (within calipers) in the same patient
When using the transvaginal approach, attention must be paid to the real-time images during the insertion of the transducer as some anomalies may “hide” from view. For example, a pedunculated endometrial polyp or intracavitary fibroid with a long stalk that has prolapsed into the vagina may not be visualized (Fig. 18.2). Such lesions are known to slip pass the transducer and could remain undetected as these lesions tend to move to the side of the transducer and lie outside the imaging field. Another example of how lesions may be hidden is the subserous fibroid on the anterior wall of an axially oriented uterus which may be obscured by bowel gas. These subserosal lesions may be better visualized during transabdominal US examination. It is important to tailor the study according to the patient’s symptoms and to scan the symptomatic region, e.g., a painful abdominal wall may be due to endometriotic implants (Fig. 18.3), abscess, hematoma, or hernia. This would necessitate a change of transducer from the convex to a higher frequency linear array probe.
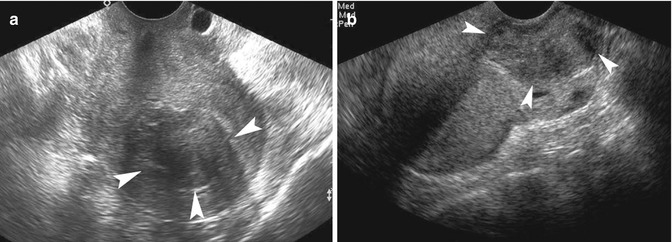

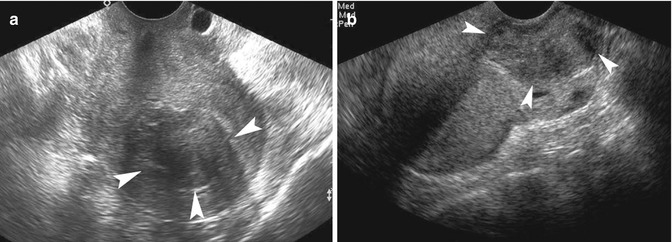
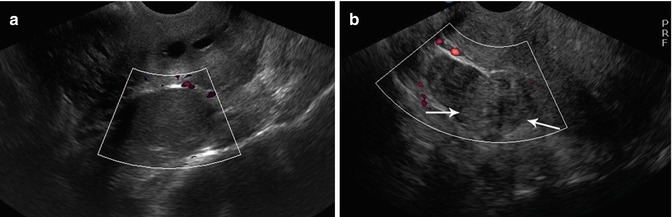
Fig. 18.2
(a) Transvaginal US image shows an intracavitary fibroid in the upper uterine cavity (arrowheads). (b) Follow-up US image shows that the intracavitary fibroid (arrowheads) had prolapsed into the vagina due to its long peduncle

Fig. 18.3
US image shows an endometriotic implant (arrows) in the left rectus abdominis of a 27-year-old patient who had pain over the anterior abdominal wall
18.2.2 Image Orientation
The operator also needs to know that the image shown on the monitor during transvaginal US is essentially rotated due to the way in which the transducer is placed in the patient. The US beam is directed towards the cranial side, instead of the back of the patient in the transabdominal approach. Thus, the top or narrowest part of the image is at the caudal side of the patient, whereas the widest part of the image is towards the cranial side of the patient. On the sagittal view, the anterior part of the patient is on the left side of the monitor. A fluid-fluid level is shown as a vertical interphase (Fig. 18.4) on the sagittal view during transvaginal US imaging.
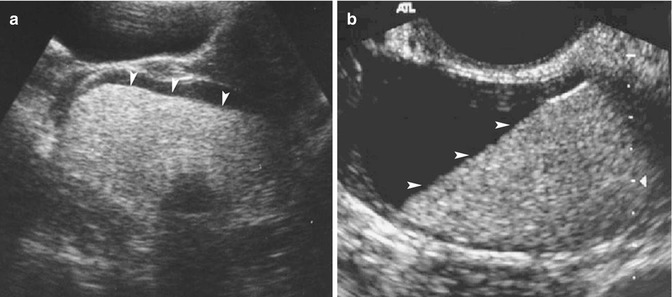
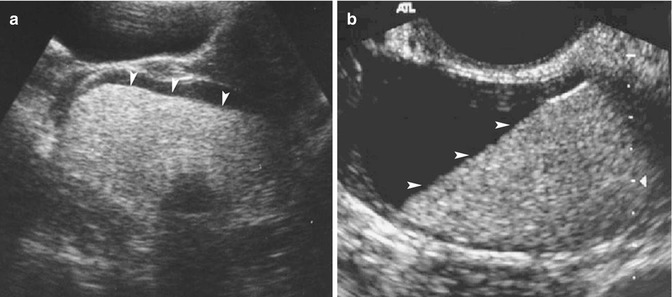
Fig. 18.4
Change in orientation of fluid-fluid levels on transvaginal US. (a) Transabdominal US image shows a fat-fluid level (arrowheads) in a cystic teratoma. (b) Transvaginal US images show almost vertical orientation of fat-fluid level (arrowheads) in the same cystic teratoma
18.2.3 Technical Considerations
Operator skill and patient habitus affect the quality of the US study. With regular use of transvaginal US, the problems relating to body habitus are usually mitigated. The interaction of US and body tissues can sometimes result in appearances that resemble anomalies. An example is the echo enhancement of the uterine wall distal to the endometrium (Fig. 18.5) that may sometimes be mistaken for uterine mass. The enhancement is more pronounced during the luteal phase of the menstrual cycle. An evaluation of the outlines of the apparent “anomaly” would reveal its straight borders that emanate from each end of the endometrium. There are also challenges during scanning and interpretation in the presence of devices such as the vaginal pessary and intrauterine device (IUD). The vaginal pessary prevents good contact of the transducer with the vaginal wall and can result in a less optimal study. In most cases though, it is possible to obtain sufficient images of the uterus for assessment. The acoustic shadowing from the devices (Fig. 18.6) may obscure structures, and therefore, care should be taken to scan around the devices, if possible.
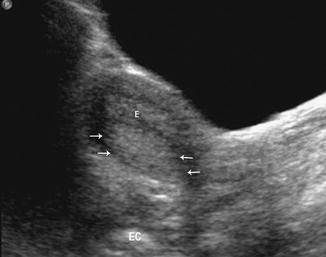
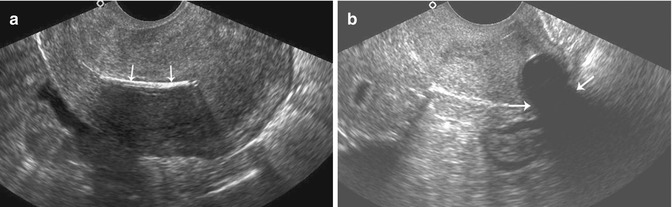
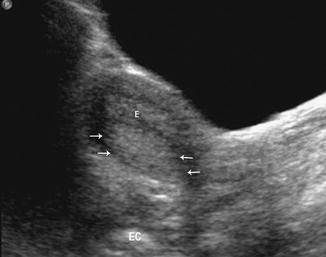
Fig. 18.5
Acoustic enhancement of ultrasound (arrows) seen in the posterior wall of the uterus caused by the normal endometrium (E)
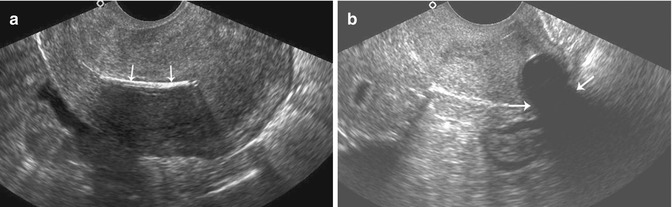
Fig. 18.6
Devices that cause shadowing in a pelvic US study. (a) Sagittal US image of the uterus shows acoustic shadowing from an intrauterine device (IUD) (arrows). (b) US image of the uterus shows acoustic shadowing from a pessary (arrows). The pessary itself cannot be seen as it has been obscured by its own shadow
In the assessment of the IUD, it is essential to report its position in the uterus. However, malpositioning of the IUD may not be readily apparent on a two-dimensional (2D) image to the inexperienced. Three-dimensional (3D) US can provide a better assessment of IUD position and type (Fig. 18.7). The acoustic shadow from the IUD has also been used to assess the type of IUD (Valsky et al. 2006), but it does not confirm its location within the endometrial cavity. Intrauterine devices that are not commonly used in the country of the medical practitioner should be highlighted, such as the ring IUD (Fig. 18.8). Some of these devices may not have any string and require special techniques for their removal. While a vaginal tampon is easily recognized on a radiographic examination or CT, an inexperienced operator may have difficulty recognizing it on US images (Fig. 18.9). Calcified or fat-containing structures may cause underestimation of size (Fig. 18.10) due to difficulties in visualizing the margins. Teratomas may show similar echogenicities to bowel and this may result in its non-detection. Conversely, bowel may be mistaken for an ovarian teratoma.
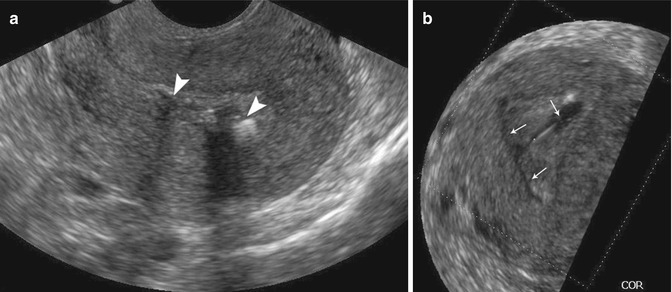
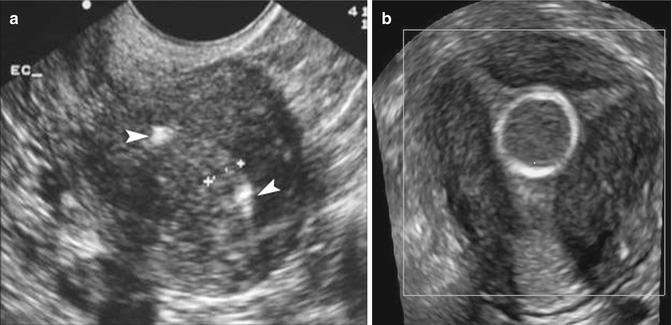
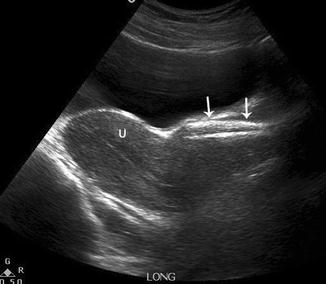
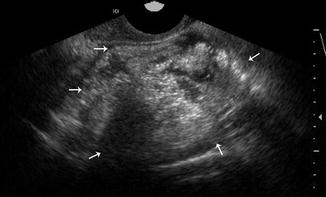
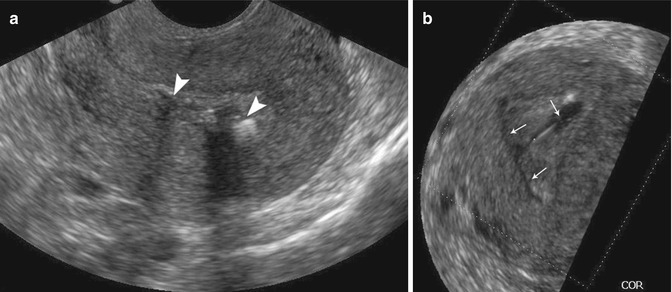
Fig. 18.7
(a) Conventional sagittal US image of the uterus shows parts of the rotated IUD (arrowheads). (b) 3D US image of the uterus shows a rotated T-shaped IUD (arrows)
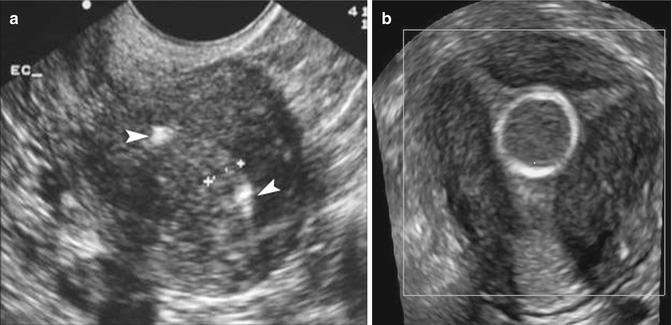
Fig. 18.8
(a) Conventional sagittal US image of the uterus shows parts of ring IUD (arrowheads). (b) 3D US image of the uterus shows a ring IUD
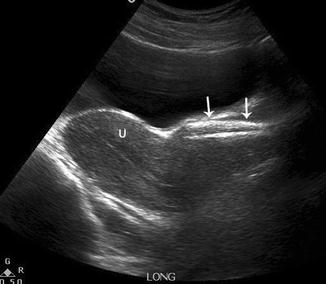
Fig. 18.9
Pelvic US image shows the longitudinal section of the uterus (U) and vaginal tampon (arrows)
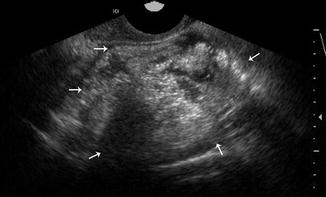
Fig. 18.10
Transvaginal US image shows an ovarian teratoma (arrows) with heterogeneous echogenic material, resembling bowel contents
18.3 Physiological Changes
The ovaries and endometrium undergo changes during the menstrual cycle. When a woman presents for the US examination, the imaging presents only a snapshot of part of the cycle. The clinician interpreting the study has to determine if the findings are physiological, or otherwise, by correlating them to the patient’s menstrual cycle. During the follicular phase, the mature follicle may reach 3 cm in diameter at mid-cycle. Following ovulation, the corpus luteum develops. Hemorrhage may sometimes occur in the corpus luteum. Sometimes the appearance may mimic a neoplasm, a well-known pitfall. Hemorrhage within the cyst commonly produces stranding resembling “fish net” or “cobweb” due to fibrin strands (Fig. 18.11). These features are strong predictors of a non-neoplastic hemorrhagic cyst (Patel et al. 2005). Occasionally, the thick hemorrhagic fluid may resemble a solid-appearing structure, and adherent clots (Fig. 18.12) may resemble papillary excrescences seen in ovarian tumors. Color Doppler may be used to check for vascularity to distinguish solid tumor components from blood clots. Given the challenges in separating pathological from physiological changes, some operators have opted to perform gynecological US imaging during the early follicular phase.
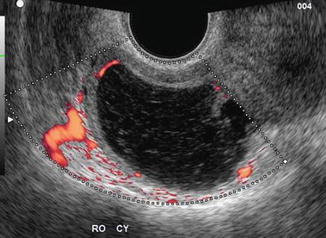
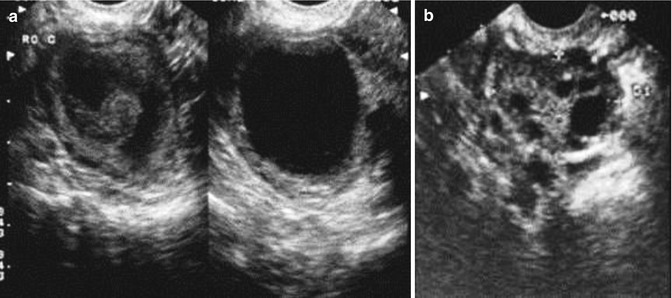
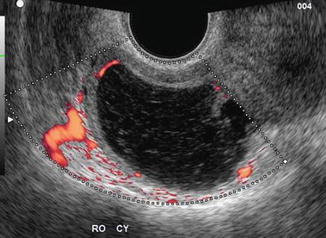
Fig. 18.11
US image shows fibrin strands within a hemorrhagic corpus luteum resulting in a “cobweb” or “fishnet” appearance. Peripheral vascularity of the corpus luteum is also shown
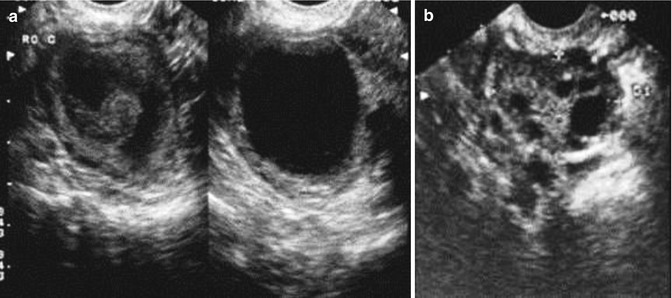
Fig. 18.12
(a) US image shows a blood clot (arrows) within a functional cyst that subsequently resolved. (b) Follow-up US image of the same ovary shows resolution of the clot
18.4 Pitfalls Relating to the Uterus
18.4.1 Uterine Anomalies
The uterine leiomyoma or fibroid is the commonest type of uterine tumor. It is distinguishable by its well-marginated border, internal refractive shadowing, and in some cases, the whorled echo texture. Structures or pathology that may mimic it include adenomyosis, the fundus of the retroverted uterus, the rudimentary horn of a unicornuate uterus, bowel mass, solid ovarian mass, and metastatic disease. Adenomyosis is a common abnormality of the uterus. Its main US features are enlargement of the uterus, inhomogeneity of the myometrium, myometrial cysts, and poor definition of the endometrium. It may present as a mass (Fig. 18.13) and occasionally resemble uterine leiomyoma. Degenerative changes in uterine fibroids can result in a variety of appearances. The most common is calcification. Large calcified fibroids can obscure other parts of the uterus and pelvis. Cystic degeneration of uterine fibroids can sometimes make them indistinguishable from ovarian masses, particularly if the fibroids are extrauterine in location. A subserosal cystic fibroid at the uterine cornu may sometimes be difficult to distinguish from an interstitial ectopic pregnancy (Fig. 18.14), if the intrauterine pregnancy is not found.
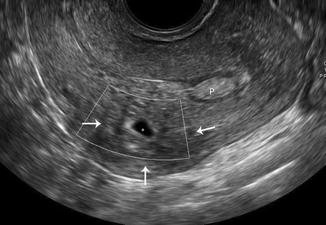

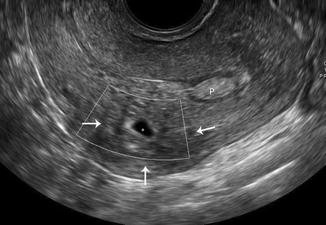
Fig. 18.13
Sagittal US image of the uterus shows focal adenomyosis (arrows) with a cystic area (asterisk). (P endometrial polyp)

Fig. 18.14
US image shows a cystic mass (arrows) that was a uterine fibroid with cystic degeneration in a 33-year-old patient presenting with right-sided pelvic pain. The lesion resembled an interstitial ectopic pregnancy, but the serum β-hCG was only 13/L and declined to nonpregnant levels over a few days. The mass resolved after several months
Marked distension of the uterine cavity due to obstruction by tumor or cervical stenosis may produce an appearance that resembles a cystic ovarian tumor (Fig. 18.15). Occasionally, hematocolpos due to accumulation of menstrual fluid from an imperforate hymen or vaginal septum may be mistaken for the urinary bladder (Fig. 18.16). Careful examination would reveal that the configuration of the cystic structure is unlike that of the urinary bladder, and the uterus should be demonstrated in connection with the structure. Calcifications of the arcuate arteries are common on US in older females and should not be mistaken for pathology (Fig. 18.17). Adhesions that result in a partitioning of the endometrial echo may be mistaken for a septate or subseptate uterus on conventional scans. In a septate or subseptate uterus, the partition (septum) is linear, often midline, and extends up to the uterine fundus, whereas adhesions may have different shapes and occur in any part of the uterine cavity. 3D US examination can be very useful in differentiating these cases (Fig. 18.18).
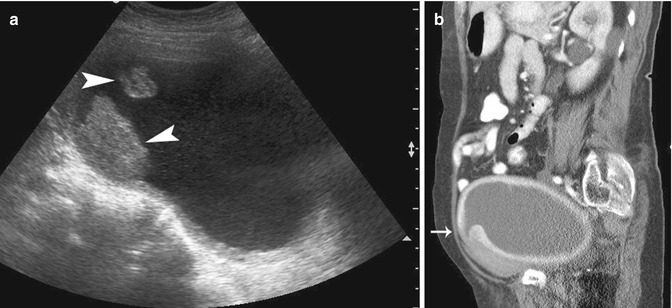
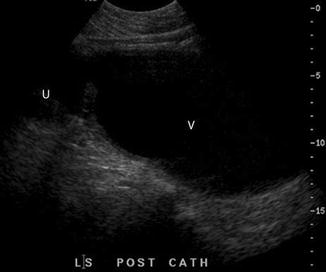
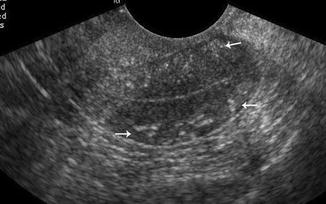
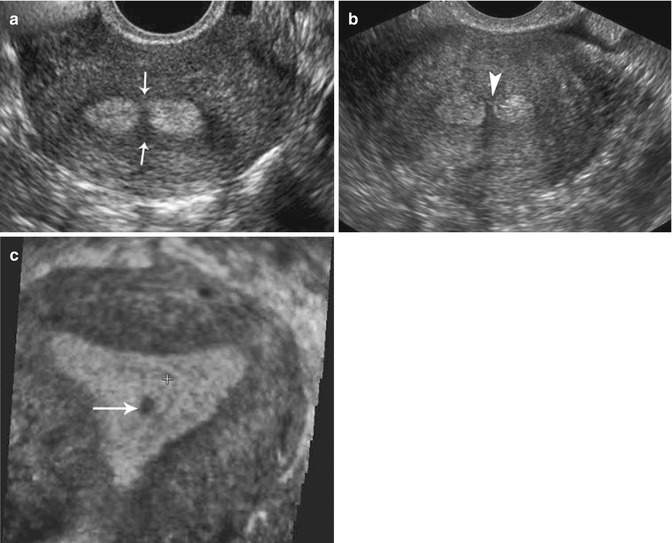
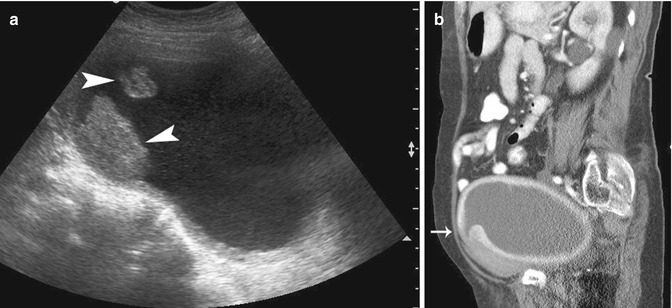
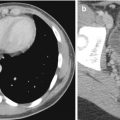
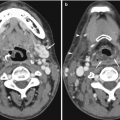
Fig. 18.15
US and CT illustrations of a markedly distended uterus, in an elderly woman, that mimicked an ovarian mass on US. (a) Transabdominal pelvic US image shows a cystic mass with excrescences (arrowheads), suspicious for an ovarian malignancy. (b) CT image shows a markedly distended uterus due to cervical obstruction. The cervix is arrowed
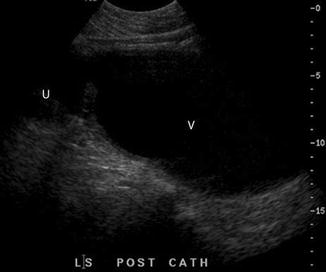
Fig. 18.16
Longitudinal US image of the hematocolpos (V vagina) due to imperforate hymen (U uterus)
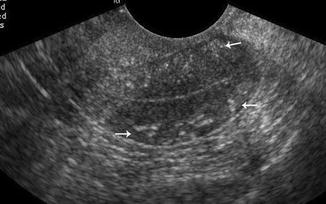
Fig. 18.17
Sagittal US image of the uterus in an elderly woman shows vascular calcifications (arrows)
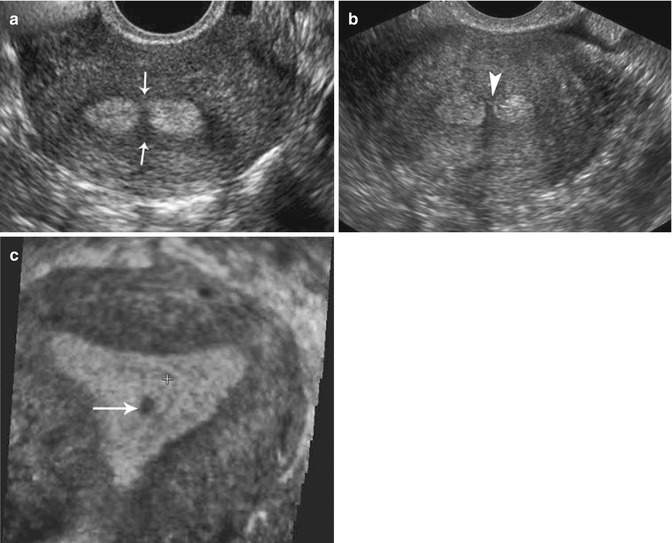
Fig. 18.18
US illustration of uterine adhesion mimicking the uterine septum and use of 3D US to improve demonstration of these anomalies. (a) Coronal US image of the uterus shows a bridging structure or defect in the endometrium (arrows). (b) Coronal US image of the uterus of another patient shows the uterine septum (arrowhead) in a subseptate uterus. (c) 3D US image of the uterus (shown in a) shows the defect (arrow) in the central part of the endometrium due to the adhesion
18.4.2 Postsurgical Changes in the Uterus
Lower segment cesarean section scars are commonly associated with deformity of the lower anterior uterine wall. Such deformities may occasionally be mistaken for a small subserosal fibroid. Menstrual fluid may be trapped in the cesarean section niche (Fig. 18.19) and result in abnormal vaginal bleeding (Thurmond et al. 1999). Even partially resorbed sutures within the uterine myometrium may pose problems in interpretation (Fig. 18.20). Their echogenic appearance resembles calcifications.

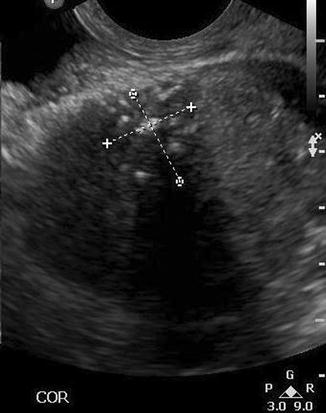

Fig. 18.19
Sagittal transvaginal US image of the uterus distended with saline shows a small niche in the lower anterior uterine wall (arrow) related to previous lower segment cesarean section
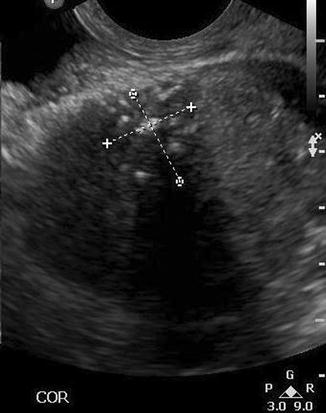
Fig. 18.20
US illustration of echogenicities (within calipers) due to partially resorbed sutures from a recent cesarean section
18.4.3 Small or Absent Uteri
Absence of the uterus may be difficult to differentiate from hypoplastic uterus in a prepubertal patient on US examination. Assessment is better through an MRI study.
18.4.4 Assessment for Retained Products of Conception
US diagnosis of retained products of conception (Fig. 18.21) can be challenging. While a negative US study has a good predictive level (Maslovitz et al. 2004), the presence of a mass in the endometrial cavity or thickened endometrial echo is not always predictive of retained products (Sadan et al. 2004). Blood clots may simulate retained products, while color Doppler US can sometimes differentiate them. Therefore, a combined approach to diagnosis using clinical assessment and ultrasound is essential.
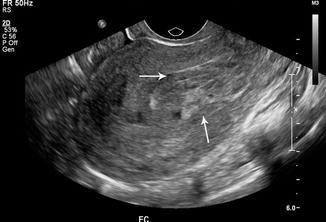
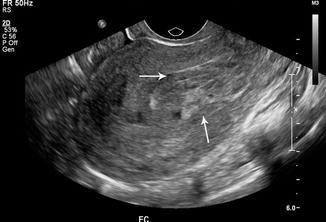
Fig. 18.21
Sagittal US image of the uterus shows inhomogeneous material within the endometrial cavity (arrows) due to retained products of conception
18.5 Pitfalls Related to Adnexal Lesions or Findings
18.5.1 Ovarian Lesions
Apart from physiological cysts, the main point of evaluating ovarian lesions is to determine if they are likely to be benign or malignant. In a study that used data from the International Ovarian Tumor Analysis (IOTA), accuracy in characterization of ovarian lesions was found to depend very much on experience and expertise (Calster et al. 2007). Tumor markers, such as CA-125, risk of malignancy indices and mathematical models are less reliable. Despite the high rates of accuracy in differentiating the benign from malignant lesions, there remain approximately 7 % of ovarian masses that cannot be characterized (Valentin et al. 2011). Benign lesions outnumber malignancies. Even among postmenopausal women, the risk of malignancy of incidental simple ovarian cysts remains low (Bailey et al. 1998). However, the rapid doubling time observed in malignant ovarian lesions does not allow for complacency in the management of any adnexal lesion that is detected.
There are benign ovarian lesions that undergo malignant transformation. A well-known example is endometriosis (Fig. 18.22). Several cohort studies of women suffering from endometriosis has shown an increase in incidence of ovarian cancers among these women (Nezhat et al. 2008). The development of solid nodules or papillary excrescences within a cystic lesion should be regarded with high suspicion. On MRI, the corresponding findings would be nodules within the cystic masses. However, during pregnancy, development of mural nodules due to decidual reaction of the endometrial lining in the cysts has been described (Tanaka et al. 2002; Poder et al. 2008). The authors were able to differentiate the malignant nodules was based on similarities in the signal characteristics of these benign nodular changes with the normal endometrium. An example of a benign ovarian tumor mimicking malignancy is the ovarian fibroma which may be associated with ascites and pleural effusion (Meigs’ syndrome).