Case presentation
A 9-year-old female seeks care after falling from her bicycle. She states that she was riding her bike and attempted to “pop a wheelie.” In doing so, she fell backward, separating herself from the bike, landing initially on her buttocks, but then onto her back. There is no reported loss of consciousness and she was wearing a helmet. She denies neck pain. She did not strike the handlebars and has no chest or abdominal pain.
Her physical examination reveals no fever, a heart rate of 100 beats per minute, a blood pressure of 105/54 mm Hg, and room air oxygen saturations of 99%. She has no outward signs of trauma. There is no chest or abdominal tenderness. Her pelvis is stable and nontender. She complains of diffuse tenderness around her mid-thoracic spine but cannot pinpoint a precise location of pain. There are no obvious external signs of trauma (i.e., no hematoma, bruising, or abrasion) and there are no step-offs, crepitus, or deformities. Her extremities have no signs of trauma. She is able to ambulate but complains of mid-thoracic back pain. She is grossly neurovascularly intact.
Imaging considerations
Plain radiography
Plain film radiography is the initial imaging modality of choice. A two-view study (anteroposterior and lateral) is sufficient, and a complete view of the segment of interest is essential. Which spinal segments should be initially imaged can be based on history and clinical examination findings.
Computed tomography (CT)
CT is often utilized as an adjunct study to better visualize fractures identified on plain imaging, especially complex fractures, as CT gives excellent visualization of bony elements of the spine and depicts retropulsion of fracture fragments. CT is also used to evaluate the spine when a patient is undergoing body CT as part of a trauma evaluation. Reconstruction of the included spine is useful for fracture detection and is performed with no additional radiation exposure. In such cases, the reconstructed spine CT imaging will include only those areas included in the body scan. For example, spine reconstruction imaging from an abdomen and pelvis CT will include the lower thoracic spine, but not the upper thoracic spine. Routine use of CT as an initial imaging test should be discouraged.
Magnetic resonance imaging (MRI)
MRI is utilized when there are signs or concerns for spinal cord involvement and produces excellent visualization of the spinal canal, spinal cord, and the ligamentous elements of the vertebral bodies. Use of this modality should be reserved for patients with neurologic findings (paraesthesias, numbness, weakness, or paralysis). MRI can also be used to confirm bone marrow edema related to vertebral fracture when imaging with other modalities is negative or equivocal. Loss of more than 50% of the anterior height of the vertebral body should prompt concern for posterior element disruption and MRI should be considered. , Availability and the need for sedation may be obstacles to the use of MRI in the urgent setting.
CT versus MRI
One study specifically comparing CT and MRI for the identification of thoracic compression fractures found agreement between the two modalities with regard to fracture number and distribution. In this study, all patients underwent CT and MRI. CT was found to be highly sensitive compared to MRI, and treatment decisions and outcomes were not changed by the addition of MRI in this study population, suggesting that information obtained from MRI should be weighed against the expense, time, and sedation need.
Imaging findings
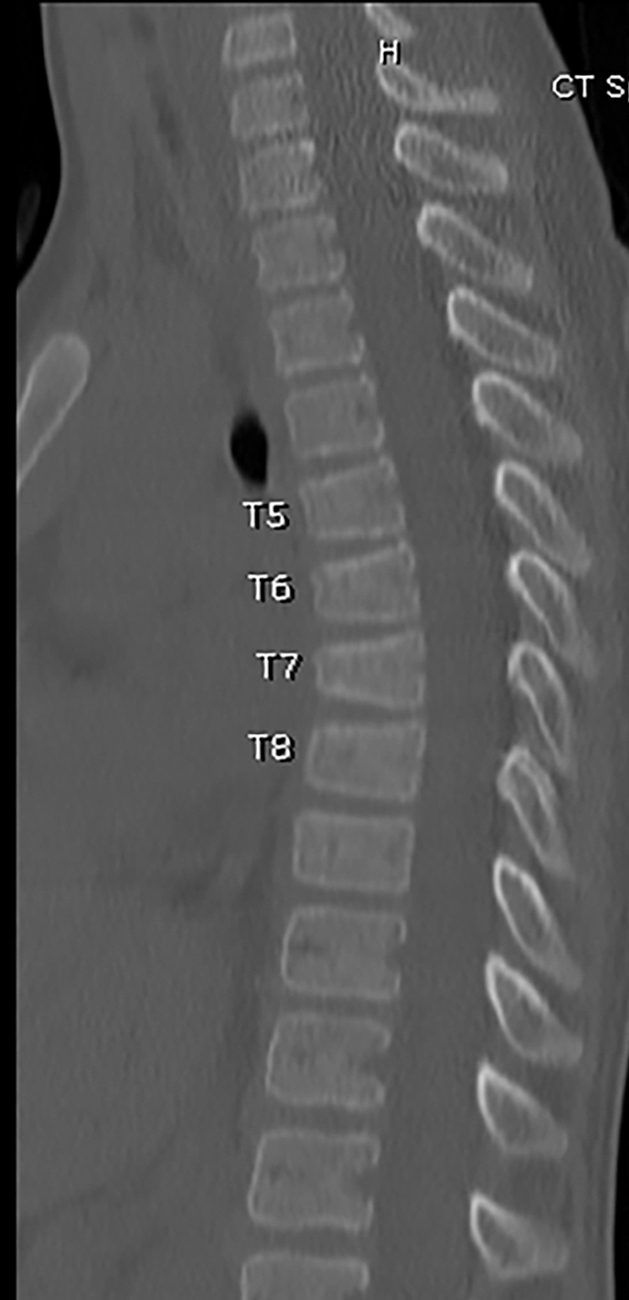
Plain radiography of the thoracic spine was obtained. This demonstrated anterior vertebral body compression fractures of T5 through T8, with approximately 50% loss of anterior vertebral body height of T7, and more mild anterior compression fractures of T5, T6, and T8 ( Figs. 49.1 and 49.2 ).


Case conclusion
Once the fractures were identified, the child underwent additional imaging. Pediatric Orthopedics was consulted. Plain radiography of the cervical spine was obtained and no additional fractures were found. Since there was 50% loss of vertebral body height at T7, associated contiguous fractures, and no neurologic symptoms, the child underwent noncontrast CT of the thoracic and lumbar and a selected sagittal image is provided. CT confirmed the T5–T8 compression fractures, greatest at T7 with 50% height loss, with no retropulsion of fracture fragments ( Fig. 49.3 ). The child was admitted for pain control and bedrest and was fitted with a thoracolumbosacral orthosis (TLSO) brace. She was discharged with careful follow-up and return precautions, specifically for the development of neurologic symptoms, such as incontinence, weakness, or numbness. She recovered uneventfully.
A comparison case is presented here, with a selected image. This child fell approximately 6 feet while playing on monkey bars. He landed on his buttocks and presented complaining of lower back pain only. There were no neurologic symptoms. Imaging revealed an anterior wedge compression fracture of T12 with less than 25% loss of vertebral body height and there is a possible subtle buckle of the anterior cortex of L1 ( Fig. 49.4 ). He underwent further plain radiography of the spine, including cervical and thoracic segments and no further fractures were found. Pediatric Orthopedics was consulted and the child was admitted for pain control, bedrest, and TLSO bracing.











