Foot and ankle disorders are common in everyday clinical practice. MR imaging is frequently required for diagnosis given the variety and complexity of foot and ankle anatomy. Although conventional MR imaging plays a significant role in diagnosis, contemporary management increasingly relies on advanced imaging for monitoring therapeutic response. There is an expanding need for identification of biomarkers for musculoskeletal tissues. Advanced imaging techniques capable of imaging these tissue substrates will be increasingly used in routine clinical practice. Radiologists should therefore become familiar with these innovative MR techniques. Many such techniques are already widely used in other organ systems.
Key points
- •
Isotropic three-dimensional MR imaging provides comprehensive joint assessment by offering exquisite, submillimeter anatomic detail while maintaining soft tissue contrast comparable with conventional two-dimensional sequences.
- •
MR neurography leverages fast spin echo and diffusion-weighted imaging techniques to provide high-resolution, nerve-selective images for assessing peripheral nerve injuries of the foot and ankle.
- •
Advanced tools for characterizing the structural integrity of cartilage, tendon, and bone include ultrashort echo time MR imaging, quantitative MR imaging, and diffusion tensor imaging.
- •
Sodium imaging with ultrahigh-field-strength MR imaging holds promise for assessing structural properties such as the glycosaminoglycan content of articular cartilage.
Introduction
Disorders of the foot and ankle, both in the setting of acute diagnosis and follow-up of lesions, are an important part of any musculoskeletal imaging practice. The incidence of foot and ankle injuries has been reported to represent as high as 10% of all trauma cases. Costs related to diabetic foot ulcer care are greater than $1 billion annually and increasing, with neuropathy and infection accounting for 90% of related admissions. Although only 3% of osseous neoplasms are found in the foot and ankle, 8% of benign soft tissue tumors and 5% of malignant soft tissue tumors are localized to these regions. Similarly, as reflected in this issue, the breadth of disorders that affect the foot and ankle is substantial. Coupled with the anatomic complexity of the foot and ankle, this presents challenges to clinicians and imagers alike. MR imaging has become established as an invaluable tool for the noninvasive diagnosis and characterization of foot and ankle evaluation because of its soft tissue contrast resolution, high spatial resolution, and multiplanar capabilities. This article discusses the state-of-the-art techniques ( Table 1 ) that are currently available on MR vendor platforms, presenting applications that may aid in diagnosis or characterization of disease. In addition, translational techniques (see Table 1 ) are presented that offer insight into potential future applications that indicate that the true destiny of MR will exceed gross structural evaluation of tissue.
| MR Techniques | Reference |
|---|---|
| Currently Available | |
| Isotropic 3D FSE for 3D rendering | |
| MR neurography | |
| Diffusion-weighted imaging | |
| Diffusion tensor imaging | |
| Novel Translational | |
| Ultrashort TE for invisible tissues | |
| Quantitative MR Biomarkers | |
| Collagen Sensitive | |
| SE T2 | |
| UTE T2* | |
| Proteoglycan Sensitive | |
| T1rho | |
| Sodium | |
| Functional Assessment | |
| Kinematic MR imaging | |
Introduction
Disorders of the foot and ankle, both in the setting of acute diagnosis and follow-up of lesions, are an important part of any musculoskeletal imaging practice. The incidence of foot and ankle injuries has been reported to represent as high as 10% of all trauma cases. Costs related to diabetic foot ulcer care are greater than $1 billion annually and increasing, with neuropathy and infection accounting for 90% of related admissions. Although only 3% of osseous neoplasms are found in the foot and ankle, 8% of benign soft tissue tumors and 5% of malignant soft tissue tumors are localized to these regions. Similarly, as reflected in this issue, the breadth of disorders that affect the foot and ankle is substantial. Coupled with the anatomic complexity of the foot and ankle, this presents challenges to clinicians and imagers alike. MR imaging has become established as an invaluable tool for the noninvasive diagnosis and characterization of foot and ankle evaluation because of its soft tissue contrast resolution, high spatial resolution, and multiplanar capabilities. This article discusses the state-of-the-art techniques ( Table 1 ) that are currently available on MR vendor platforms, presenting applications that may aid in diagnosis or characterization of disease. In addition, translational techniques (see Table 1 ) are presented that offer insight into potential future applications that indicate that the true destiny of MR will exceed gross structural evaluation of tissue.
| MR Techniques | Reference |
|---|---|
| Currently Available | |
| Isotropic 3D FSE for 3D rendering | |
| MR neurography | |
| Diffusion-weighted imaging | |
| Diffusion tensor imaging | |
| Novel Translational | |
| Ultrashort TE for invisible tissues | |
| Quantitative MR Biomarkers | |
| Collagen Sensitive | |
| SE T2 | |
| UTE T2* | |
| Proteoglycan Sensitive | |
| T1rho | |
| Sodium | |
| Functional Assessment | |
| Kinematic MR imaging | |
Applications of currently available sequences
Isotropic Three-Dimensional Fast Spin Echo Acquisition for Three-Dimensional Rendering
Historically, most musculoskeletal MR imaging protocols have relied heavily on two-dimensional (2D) multislice acquisitions, reserving three-dimensional (3D) volumetric sequences for instances in which thinner slice thickness, higher in-plane resolution, reduced volume averaging, and the ability to reconstruct in other planes were desired. The major disadvantages of these sequences were suboptimal soft tissue contrast and long acquisition times. More recently, 3D fast spin echo (FSE) sequences have been developed that achieve tissue contrast similar to 2D FSE sequences, in clinically feasible scan times. Some version of an isotropic 3D FSE sequence is available on the major MR vendor platforms.
Two major advantages have been leveraged in the literature with regard to implementation of the isotropic 3D FSE sequences. First, the approximation of tissue contrast that approaches 2D FSE techniques provides the possibility for a comprehensive joint assessment with markedly decreased overall scan times (scan once and reformat in any plane). Second, the submillimeter, high-resolution source images allow detailed evaluation of small, complex anatomic structures.
Although computed tomography (CT) has traditionally been the imaging method used for the evaluation of bone, both qualitatively and for generating 3D reconstructions, recent developments related to 3D MR imaging sequences suggest a potential new role for MR imaging in this regard. Studies are emerging in the literature that establish that MR provides resolution and contrast that allow equal or superior ability compared with CT to detect osseous disorders such as occult fracture, as well as characterization of fractures required for preoperative planning. A few recent studies have addressed the use of 3D MR sequences to generate 3D renderings of bones, and this is clearly an area of potential development in joints such as the ankle, in which complex trauma, articular surface evaluation, and bone alignment, among other things, may benefit from 3D visualization of bones ( Fig. 1 ). The capability to provide this added information from the MR imaging study establishes a sort of one-stop shop, where the patient can avoid the delay of an added imaging study and the exposure to ionizing radiation, and that also represents a better use of health care dollars.
Magnetic Resonance Neurography
General MR protocols to evaluate peripheral nerves require the ability to detect alteration in nerve signal intensity and morphology, necessitating a combination of sequences that provides high-resolution and sensitivity to mobile water. Acquiring a high-quality peripheral nerve MR study that is clinically helpful requires time and attention to detail. Protocols should be planned with all available clinical information as well as electrodiagnostic test results. In many cases, the field of view must be tailored to cover a broader area initially for the purposes of screening, followed by smaller field of view 2D and 3D imaging targeted to areas of identified abnormalities. Protocols based on a combination of T2 and diffusion-weighted imaging (DWI) neurographic sequences have been proposed. These sequences include T1 FSE, T2 adiabatic inversion recovery, proton density, 3D inversion recovery, and 3D diffusion-weighted reversed fast imaging with steady state precession (DW-PSIF) hybrid pulse sequences. The DW-PSIF hybrid pulse sequences provide nerve-selective images, with suppression of adjacent vascular structures, which can be particularly helpful in the foot and ankle ( Fig. 2 ). Diffusion tensor imaging (DTI) is another technique that has been implemented in peripheral nerve evaluation. It exploits the anisotropic properties of axonal fiber tracts, allowing fiber tract mapping as well as calculation of quantitative parameters such as the absolute diffusion coefficient (ADC). This technique is technically demanding, and has not been broadly adapted for clinical use, but shows great promise for lesion characterization. The ADC is a quantitative descriptor of diffusivity and fractional anisotropy ( Fig. 3 ). The mean diffusivity quantifies the average displacement of water molecules, and fractional anisotropy measures the directional preference of the diffusion of the water molecules. If the fractional anisotropy measurement is zero, diffusion is isotropic and can go in any direction (unrestricted), or can go nowhere (completely restricted). If the fractional anisotropy is 1, it means diffusion occurs along only 1 axis and is fully restricted in all other directions. Neuropathic conditions often result in a decreased fractional anisotropy (increased ADC), in which recovering axons often show increased fractional anisotropy (decreased ADC).
Peripheral nerve injury in the foot and ankle is common and can be related to acute trauma, chronic repetitive microtrauma, entrapment syndromes within fibro-osseous tunnels, and postprocedural iatrogenic lesions. Nerve sheath tumors and systemic neuropathies can also affect the nerves of the foot and ankle. MR criteria ( Box 1 ) for distinguishing a normal versus abnormal nerve include size (using adjacent vascular structures as an internal standard), signal intensity (isointense to skeletal muscle on T1 and T2; may be minimally hyperintense to muscle with T2 fat suppression or inversion recovery), preservation of fascicular pattern, smooth course without deviation, preserved perineural fat, normal diffusion tensor tracts, normal fractional anisotropy values (>0.4–0.5), and symmetric brightness on diffusion tensor images.
MR criteria for a normal nerve
Size, using adjacent vascular structures as an internal standard
Signal intensity isointense to skeletal muscle on T1 and T2 (may be minimally hyperintense to muscle with T2 fat-suppressed or inversion recovery)
Preservation of fascicular pattern
Smooth course without deviation
Preservation of perineural fat
Normal diffusion tensor tracts
Normal fractional anisotropy values greater than 0.4 to 0.5
Symmetric brightness on diffusion tensor images
Diffusion-Weighted Imaging
As indicated earlier, DWI has been studied in the peripheral nervous system, and even more robustly in the central nervous system, for some time. Tissue analysis using DWI is based on assumptions that magnitude and direction of local diffusivity in tissue are influenced by the macromolecular environment of diffusing bulk water. Information on tissue structural property is provided by measuring spatial restriction of diffusivity (in contrast with unrestricted diffusion in free water) according to tissue ultrastructure. With conventional DWI, diffusion-sensitizing gradients are applied in a single direction with the subsequent total diffusion movement registration limited to that direction. By combining DWI with DTI, several diffusion-sensitizing gradient pairs in different noncoplanar directions are applied, allowing determination of degree of diffusional anisotropy as well as main directions of local diffusion in a tissue. DTI is based on the fact that the magnitude and molecular motion of water are restricted by structural elements within the tissue, theoretically lending itself to the evaluation of ordered structures such as cartilage and tendon. It has already been implemented in skeletal muscle, bone, and musculoskeletal soft tissues. DTI has been proposed as a biomarker for cartilage composition and structure because of its sensitivity to proteoglycan content through mean diffusivity and to collagen architecture through the fractional anisotropy. It has recently been used to assess postoperative tendon quality in patients with Achilles tendon rupture, providing information regarding the trajectory and tendinous fiber continuity in the repair tissue.
The advantages of DTI as a potential MR biomarker for assessment of articular cartilage are that it evaluates both proteoglycan and collagen without the need for exogenous contrast material and it does so at a higher resolution than sodium ( 23 Na)-based MR imaging ( Fig. 4 ). In addition, DTI has the ability to assess collagen and proteoglycan independently of each other. The configuration of the collagen fibril network induces anisotropy (measured with fractional anisotropy) of the water molecules. However, the proteoglycan molecules do not show preferred orientation and therefore restrict motion of water molecules equally in all directions. For this reason, proteoglycan content affects only mean diffusivity. However, diffusion cannot provide a quantitative estimation of the absolute proteoglycan or collagen composition. Further, translation of DWI to the musculoskeletal system has proved difficult for 2 reasons. First, the short T2 of articular cartilage (20–40 milliseconds) causes low signal-to-noise ratio in standard DWI techniques that require long echo times (TEs). Second, the sensitivity of DWI to patient motion makes it difficult to achieve the high spatial resolution required for cartilage evaluation. Several recent publications suggest promise for overcoming these technical challenges in patient cohorts.
Novel magnetic resonance pulse sequences
Ultrashort Echo Time MR Imaging
Ultrashort TE (UTE) MR imaging is represented by a group of pulse sequences capable of providing TE values of less than 1 millisecond. Conventional MR imaging sequences use long TEs, resulting in limited opportunity to encode decaying signal of short-T2 tissues before that signal reaches zero. For this reason, biological tissues with intrinsic transverse relaxation times (T2, T2*) that are short (generally considered <10 milliseconds, although subclassification exists within the short category) appear black; that is, void of signal on standard MR pulse sequences. By decreasing the TE to the range of the intrinsic T2/T2* value of short-T2 tissues, signal can be acquired from these tissues, allowing morphologic evaluation. Moreover, UTE sequences can be used for quantitative evaluation of short-T2 tissues (this capability is addressed later).
The application of UTE MR imaging to the musculoskeletal system has been revolutionary, largely because of the short T2 nature of many musculoskeletal tissues. These tissues include the calcified layer of cartilage, fibrocartilaginous structures, ligaments, tendons, and bone. The ability to acquire signal and characterize the infrastructure of short T2 tissues presents a paradigm shift in diagnosis and characterization of structural alteration. Rather than being limited to diagnosis of disorders at a point in time when the short T2 tissue has failed through traumatic tearing or severe degeneration, effectively transforming it into a long T2 tissue, UTE MR imaging affords the opportunity to identify pathologic changes at an earlier stage, which provides the chance for earlier intervention and controlled treatment. The UTE MR imaging sequences currently have limited availability on vendor platforms, but promising results have been introduced in the literature for clinical application of these sequences in the setting of meniscal repair, cartilage repair, and osteoarthrosis.
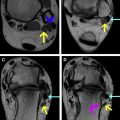
Potential applications for UTE MR imaging include evaluation of osteochondral injury, assessment of degenerative changes, and monitoring of tissue healing. Ankle sprains have an estimated daily occurrence of 27,000 in the United States, with 50% leading to osteochondral lesions. UTE MR imaging allows assessment of the calcified layer of cartilage at the talar dome, helping to characterize osteochondral junction injury acutely and in follow-up ( Fig. 5 ). Further, bone marrow–stimulating techniques (abrasion, drilling, microfracture) are used to treat chondral defects. In such procedures, it is important to assess the presence and nature of fill tissue at the repair site, as well to assess the reconstitution of the cartilage-bone interface.