Outline
Indications and Contraindications, 805
Protocols, 807
Patient and Probe Preparation, 808
Imaging Technique, 808
Pelvic Anatomy, 811
Vascular Anatomy, 816
The Uterus, 821
The Ovaries, 826
The Fallopian Tube, 827
The Urinary Bladder, Distal Ureters, and Urethra, 829
The Rectosigmoid Colon, 829
Conclusions, 832
Summary of Key Points
- •
Transabdominal sonography (TAS) and transvaginal sonography (TVS) are often complementary, providing different diagnostic information. TAS provides a wider field of view and better visualization of superficial structures and large pelvic masses but has limited resolution. The transvaginal approach allows the probe to be placed closer to the “target organs,” providing higher resolution imaging, but has a limited field of view.
- •
Because of the ability to use higher frequency probes, TVS usually provides the best anatomic detail. Therefore, TVS is considered the optimal sonographic technique with the highest diagnostic yield and should be incorporated into the sonographic examination of the female pelvis unless there are reasons that the transvaginal approach should be avoided.
- •
Not all patients are appropriate candidates for transvaginal examination. The examination should not be performed on any patient who does not or cannot willingly consent to the procedure, as well as on most virginal patients and those who experience marked discomfort with probe insertion.
- •
The appearance of the normal endometrium and ovary varies significantly throughout the menstrual cycle in women of reproductive age. It is important to be cognizant of the expected changes in order to avoid misinterpreting physiologic changes as pathologic.
- •
Transperineal, translabial, and transrectal sonography should be considered alternative approaches for imaging the female pelvis and are particularly useful for evaluation of the postmenopausal uterus, the cervix, and the lower urinary tract.
Pelvic sonography is considered the initial imaging tool of choice for assessing suspected gynecologic disorders in patients of all ages. Sonography offers the advantages of widespread availability, low cost, and lack of exposure to ionizing radiation and is often the only imaging examination necessary for diagnosis of uterine, ovarian, and adnexal disease. In addition, sonography is extremely useful in the evaluation of pathologic changes affecting the pelvic portions of the urinary system, gastrointestinal tract, and musculoskeletal structures that may mimic the clinical presentation of gynecologic disease. In many ultrasound laboratories, the standard protocol for ultrasound examination of the female pelvis begins with TAS using the filled urinary bladder as the acoustic window, followed by TVS after emptying the bladder and placing the patient in the lithotomy position. The two imaging techniques are complementary, often providing different diagnostic information. TAS provides a wider field of view than the transvaginal approach and provides better visualization of superficial structures and structures remote from the vagina. However, by placing the probe closer to the “target organs,” the transvaginal approach requires less depth of penetration and bypasses the attenuating soft tissues overlying the pelvic organs, allowing utilization of a higher frequency probe, which provides higher resolution and anatomic detail of the uterus, ovaries, and adnexa ( Fig. 26-1 ). The normal sonographic anatomy described in this chapter reflects a combined transabdominal and transvaginal approach and is weighted, as in clinical practice, to emphasize the positive attributes of both TVS and TAS.

Indications and Contraindications
High-resolution TVS has been widely available since the mid-1980s and is considered an integral part of gynecologic as well as early obstetric sonographic examinations. TVS typically provides more anatomic detail of the uterus, endometrium, ovaries, and adnexa than does TAS. This is because the probe is placed closer to the organs of interest and requires less depth of penetration; therefore, a higher frequency probe with ensuing higher resolution can be utilized ( Figs. 26-2 and 26-3 ).


An additional advantage of TVS is the capability of using the probe tip to assess pelvic structures for tenderness. By applying gentle pressure with the transducer tip to pelvic structures, it is possible to localize the region of tenderness with greater specificity than with TAS or bimanual examination. Hence, TVS is considered the optimal sonographic technique for imaging the female pelvis and should be incorporated into the sonographic examination in all situations for which it will provide additional clinically useful diagnostic information, barring contraindications to the transvaginal approach (see later).
Indications for pelvic sonography include but are not limited to the following :
- •
Evaluation of pelvic pain and pelvic masses
- •
Evaluation of endocrine abnormalities, including polycystic ovaries
- •
Evaluation of dysmenorrhea, amenorrhea, abnormal vaginal bleeding, and delayed menses
- •
Evaluation, monitoring, and treatment of infertility patients
- •
Evaluation of pelvic anatomy in the setting of a limited clinical examination
- •
Evaluation of suspected pelvic infection
- •
Further characterization of a pelvic abnormality noted on another imaging study
- •
Evaluation of congenital uterine and lower genital tract anomalies
- •
Evaluation of excessive bleeding, pain, or signs of infection after pelvic surgery, delivery, or abortion
- •
Localization of an intrauterine contraceptive device
- •
Screening for malignancy in high-risk patients
- •
Evaluation of incontinence or pelvic organ prolapse
- •
Evaluation for possible ectopic pregnancy
- •
Evaluation of a first trimester gestation for viability, growth, and anomalies
- •
Evaluation of the placenta, cervix, and other pelvic structures in second and third trimester gestations
- •
Evaluation of fetal anatomy in second and third trimester gestations
- •
Guidance for interventional or surgical procedures

Although TVS offers superior resolution to TAS, TVS maybe compromised by sound attenuation (e.g., by large or calcified leiomyomas in the lower uterus) or by positioning of the ovaries or other lesions high in the pelvis beyond the field of view of the transvaginal probe. Large uterine size and fixation of the uterus to the anterior abdominal wall by adhesions, such as after cesarean delivery, can also limit the ability of TVS to assess the entire uterus for pathologic change or to perform accurate measurements. In these situations, TAS provides a wider field of view than the transvaginal approach and thus allows better visualization of structures in the upper pelvis or in a superficial location. Furthermore, TAS can provide a more panoramic view of the entire pelvis, which is helpful in the setting of a large pelvic mass ( Fig. 26-5 ). TAS also allows assessment of related intra-abdominal disease and structures, such as quantification of free intraperitoneal fluid in the hepatorenal space and paracolic gutters, hydronephrosis in the setting of a large pelvic mass or malignancy, and, more rarely, identification of peritoneal implants.

Protocols
Protocols for pelvic sonography vary between institutions and can be tailored according to the specific clinical indication. In some institutions, it is routine to perform a complete transabdominal pelvic sonogram using the distended urinary bladder as an acoustic window, followed by a complete transvaginal pelvic sonogram with an empty bladder. In other institutions, women are not asked to fill their bladders before routine pelvic sonograms, but initially have a limited transabdominal examination, irrespective of the fullness of the urinary bladder, to screen for large pelvic masses and to measure the uterus. Subsequently, the patient is asked to void and a complete transvaginal sonogram is performed. At other sites, patients initially undergo TVS with an empty bladder, because this examination alone will provide diagnostic imaging in the majority of cases. In this scenario, if TVS does not provide adequate imaging, most commonly because one or both of the ovaries are not visualized or there is incomplete visualization of an enlarged uterus or pelvic mass, TAS with an empty or partially filled urinary bladder is then performed. In a small minority of patients, the combination of these two examinations will still fail to visualize an ovary or the entire pelvic anatomy, and the patient is then asked to fill her bladder and the transabdominal examination is repeated with a distended bladder.
Patients who undergo serial pelvic sonography for specific targeted indications, such as follicle monitoring, are often only examined by TVS. When pelvic sonography is performed in emergent clinical situations, TAS may be initially and quickly performed in the setting of an empty or incompletely filled bladder to assess for the presence of hemoperitoneum, a large pelvic mass, or other pathologic features, and TVS is then performed if considered necessary as guided by the clinical scenario ( Fig. 26-6 ).

Patient and Probe Preparation
As with all ultrasound applications, it is standard practice to use the highest possible transducer frequency that allows visualization of the target organs. During TAS, visualization of the pelvic organs is typically limited by sound attenuation by the intervening anterior abdominal wall and subcutaneous and preperitoneal fat, as well as fat in the mesentery and omentum. As a result of this attenuation and the distance of the area of interest from the anterior abdominal wall, it is often not possible to use transducers with frequencies above 6 MHz for TAS, unless the patient is very thin. TVS is typically performed using a probe of 7.5 MHz or higher frequency, taking advantage of the ability to place the probe closer to the pelvic organs because of fewer intervening structures and resulting in less sound attenuation.
The patient should void immediately before the transvaginal examination so that the urinary bladder is as empty as possible. This will improve visualization of the reproductive organs, especially the adnexal structures, which may be displaced out of the pelvis when the bladder is distended, and will reduce patient discomfort. The sonologist or sonographer should obtain a pertinent history from the patient, explain the rationale for performing the TVS as well as how the examination is performed, and obtain verbal consent before beginning the examination. If a male sonologist or sonographer is to perform the examination, a female staff member (an aide, nurse, or other staff member) should be present in the room for the entire transvaginal examination to act as a chaperone. Consideration of having a chaperone present for all TVS, even if performed by a female, should be in accordance with local policy and is recommended in some institutions. The patient should be positioned as comfortably as possible in the lithotomy position using either a gynecologic examination table with stirrups or by placing cushions or folded linens underneath the buttocks to elevate and abduct the hip region. The patient should be appropriately covered and draped, and the examination should be conducted with the same respect for privacy afforded patients during the performance of a bimanual pelvic examination.
To prevent the spread of infectious disease, the transvaginal probe should be appropriately disinfected using high-level disinfection protocols between uses according to the manufacturers’ and Occupational Safety and Health Administration (OSHA) recommendations. Following disinfection, the probe is wiped clean, and either a small amount of transducer coupling gel is placed inside a probe cover or a pregelled probe cover is placed over the probe. Because of concern for latex allergies, many laboratories use nonlatex probe covers for all patients. Care is taken to minimize air bubbles over the transducer face when applying the probe cover, and if they are noted, the probe cover should be readjusted. The final step in the process of probe preparation is to lubricate the tip of the covered probe with a sterile, nonspermicidal lubricant. Individual packets are preferred over large multiuse containers to minimize the potential for contamination of the gel and reduce the risk of transmission of infection. The sonographer should wear gloves while preparing the probe and performing the examination.
Imaging Technique
The patient, the sonographer, or the physician may introduce the transvaginal transducer, preferably under real-time monitoring. After insertion, the sonologist should position the probe to optimize imaging of the pelvic organs, usually by placement of the probe in the anterior or lateral vaginal fornix and by the application of gradually applied firm pressure against the vaginal wall as tolerated by the patient. The orientation of the image is controlled by probe rotation and angulation ( Fig. 26-7 ). Before recording any images, many sonologists will perform a pelvic survey by slowly sweeping the ultrasound beam in a long-axis orientation from the midline through the adnexa continuing out to the pelvic sidewalls on each side. The probe is then rotated 90 degrees counterclockwise into the short axis, and the beam is swept from the cervix to the fundus of the uterus. The probe is then angled to each side of the pelvis, and scanning is performed by sweeping both superiorly and inferiorly through each adnexal region. The survey quickly ascertains the relative positions of the uterus and ovaries and identifies any obvious disease. Additionally, the probe can be advanced or withdrawn, which will move adjacent pelvic viscera and displace bowel and allow structures to be placed in the focal zone of the transducer or moved out of regions with near-field artifact. In response to gentle pressure with the transvaginal probe, the pelvic organs should normally slide over one another. Any restriction to normal motion may indicate the presence of adhesions. Visualization of the pelvic anatomy can also be facilitated by applying pressure on the patient’s anterior abdominal wall with the sonologist’s nonscanning hand, thereby pushing a mobile ovary or a mass down into the field of view of the transvaginal probe. In addition, the bimanual approach is extremely helpful in localizing pelvic tenderness or pain, allowing the sonographer to focus on the region most likely to harbor some pathologic problem.
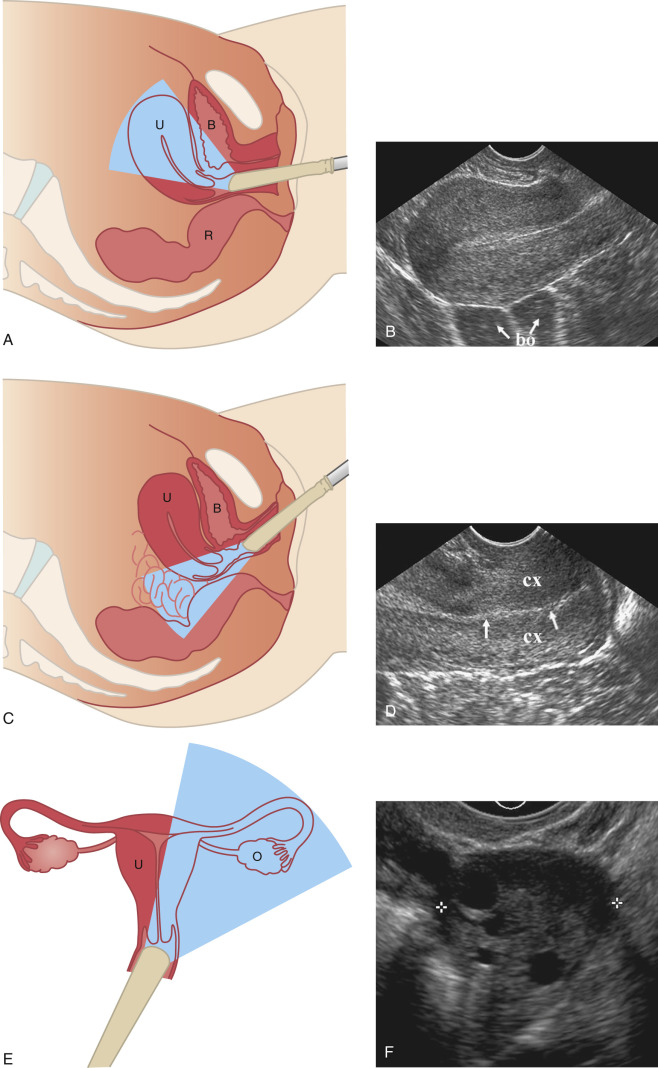
After the survey, a set of static images (or video clips) is obtained and each is appropriately labeled to indicate the anatomic structure or region imaged, as well as the orientation of the probe. In many patients, the long axis of the uterus and the ovary may be slightly oblique with respect to the long axis of the patient’s body, and the probe should be oriented along that same obliquity to image in the uterus and ovary each along its long axis. The long-axis TVS view is usually referred to as a sagittal imaging plane, and the short-axis view as a coronal or transverse imaging plane. At our institution, the imaging protocol includes one or more static sagittal views of the posterior cul-de-sac, cervix (including the endocervical canal from internal to external os), midline uterus with and without the maximum anteroposterior (AP) dimension and length measured, parasagittal right and left uterine body, midline sagittal endometrium with and without the maximum AP dimension measured, and right and left ovaries with and without the maximum AP dimension and length of each measured. Coronal or transverse static images include posterior cul-de-sac; cervix; uterus at the fundal, midbody, and lower uterine segment levels with and without the maximum width measured; midbody and fundal endometrium; and right and left ovaries with and without the maximum width measured ( Fig. 26-8 ).

Additionally, any disease or variant of normal must be assessed and appropriate additional images recorded. Most laboratories now include cine clip acquisition in addition to static images. Color Doppler, power Doppler, and pulsed Doppler are often added to the protocol depending upon the clinical situation and abnormality demonstrated on gray-scale imaging. The use of three-dimensional (3D) sonography also has become standard in many laboratories ( Fig. 26-9 ). By capturing a volume of data, 3D imaging permits a display of any desired plane through the uterus, cervix, ovaries, and adnexa and optimizes assessment of the entire endometrial canal. 3D imaging is particularly useful for the assessment of intrauterine device (IUD) positioning and submucosal myomas, as well as uterine fundal contour and morphologic appearance in the setting of suspected congenital anomalies ( Fig. 26-10 ).


Pelvic Anatomy
The pelvis, so-called because of its resemblance to a basin, is divided into two structurally continuous compartments, the true (or lesser) pelvis and the false (or greater) pelvis, by an oblique plane passing from the sacral promontory, the arcuate and pectineal lines, and the superior margin of the symphysis pubis ( Fig. 26-11 ). The circumference of this plane is called the linea terminalis, or pelvic brim. The true pelvis is the lower portion and is bounded anteriorly by the pubis and pubic rami, posteriorly by the sacrum and coccyx, laterally by the fused ilium and ischium, and inferiorly by the muscles of the pelvic floor. The false pelvis is bounded laterally by the flanged portions of the iliac bones, the base of the sacrum posteriorly, and the abdominal wall anteriorly and laterally. In the absence of masses in the nongravid patient, the uterus, ovaries, adnexa, and collapsed urinary bladder are located in the true pelvis. As the urinary bladder fills, the dome of the bladder extends into the false pelvis and displaces the loops of small bowel superiorly, providing an acoustic window for transabdominal imaging. Intracavitary probes (transvaginal and transrectal) allow visualization of the pelvic viscera from within the true pelvis. Translabial and transperineal sonography view the true pelvis from the pelvic floor.
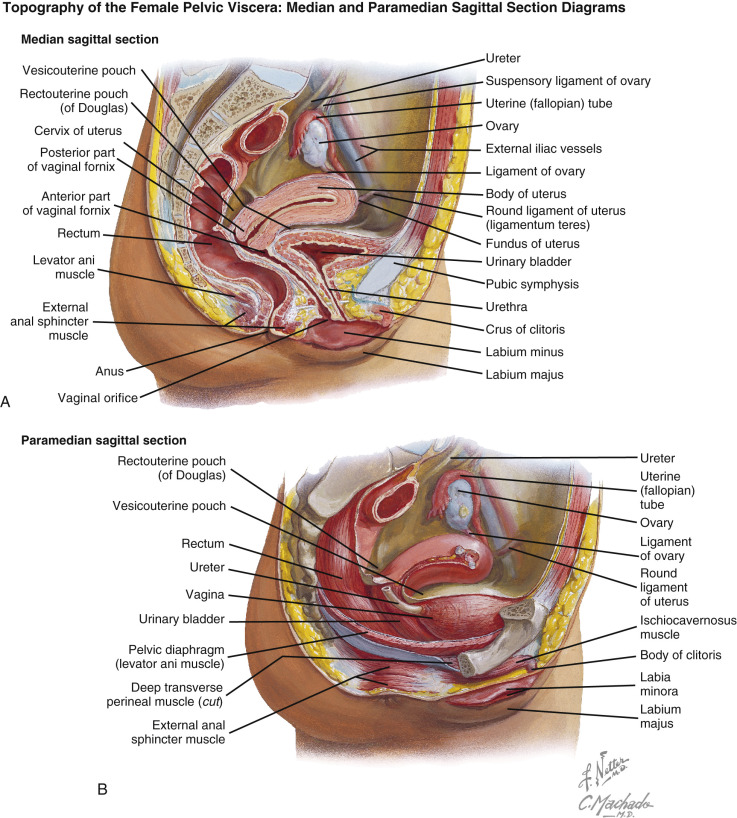
The anterior surface of the uterus is covered with peritoneum to the level of the upper cervix. The peritoneal space anterior to the uterus and posterior to the urinary bladder is the vesicouterine pouch or anterior cul-de-sac ( Figs. 26-11 and 26-12 ). This space is usually empty, but it may contain loops of small bowel. Posteriorly, the peritoneal reflection extends to the posterior fornix of the vagina ( Fig. 26-13 ), forming the posterior cul-de-sac or rectouterine pouch, which is the peritoneal space posterior to the uterus and anterior to the rectosigmoid colon. On transvaginal imaging, a small amount of free fluid is often demonstrated in the posterior cul-de-sac in normal women of menstruating age, likely from fluid released at ovulation. However, the presence of fluid in the anterior cul-de-sac or lateral pelvic recesses, a large amount of fluid in the posterior cul-de-sac, and the presence of pelvic fluid in nonovulatory female patients all raise concern for intraperitoneal disease ( Fig. 26-14 ).



Laterally, the peritoneal reflection forms the broad ligaments, which extend from the lateral aspect of the uterus to the lateral pelvic side walls bilaterally ( Fig. 26-15 ). The broad ligaments divide the pelvic cavity into anterior and posterior compartments. The free border of the broad ligaments contains the fallopian tubes. The broad ligaments may be identified sonographically when they are outlined by free intraperitoneal fluid ( Fig. 26-16 ). The ovary is attached to the posterior layer of the broad ligament by reflections of peritoneum referred to as the mesovarium (see Fig. 26-12 ). The superior margin of the portion of the broad ligament containing the fallopian tube is referred to as the mesosalpinx. The superior margin of the broad ligament lateral to the fimbriated end of the fallopian tube is the suspensory ligament of the ovary (infundibulopelvic ligament), through which the ovarian vessels and nerves course. The round ligaments arise at the uterine cornua, anterior to the fallopian tubes in the broad ligaments, and extend anterolaterally to run beneath the inguinal ligament and insert into the fascia of the labia majora. The ovarian (utero-ovarian) ligaments arise from the uterine cornua posterior to the fallopian tubes and attach to the inferior extremity of the ovary. In the absence of free intraperitoneal fluid, the fallopian tubes, mesovarium, mesosalpinx, and ovarian and round ligaments are not usually identified sonographically ( Fig. 26-17 ). The suspensory ligament of the ovary is usually not directly visible. However, the ovarian artery within the suspensory ligament of the ovary is often identified with color Doppler on TAS or TVS ( Fig. 26-18 ). The base of the lateral margin of the broad ligament is continuous with the dense connective tissue of the pelvic floor, which unites with the supravaginal portion of the cervix. The lower medial margin of the broad ligament is widely attached to the connective tissues adjacent to the cervix known as the parametrium. The uterosacral ligaments extend posterolaterally from the supravaginal cervix, encircle the rectum, and insert into the fascia over the sacrum. The uterosacral ligaments form the lateral boundaries of the rectouterine pouch.