CHAPTER 18 Normal Vascular Anatomy
EMBRYOGENESIS OF INTRACRANIAL VASCULATURE
Normal Fetal Development
The aortic arch, great vessels, and their branches approach their adult configuration by the eighth week of gestation.1 These vessels arise from paired embryonic aortic arches, which connect the aortic sac with the dorsal aorta. The initial embryonic arterial circulation is symmetric and consists of paired aortic arches connecting to paired dorsal aortae. As segments of the paired arches and dorsal aortae selectively persist or involute, the aorta and its branches take their adult form.2
Involution of the first and second aortic arches occurs by day 29 of gestation. The third, fourth, and sixth arches persist and eventually give rise to the aortic arch, pulmonary arteries, subclavian arteries, common carotid, and proximal internal carotid arteries (ICAs).3 The fifth arches may give rise to rudimentary vessels that eventually degenerate or may fail to develop.4
Dorsally, the vertebral arteries arise from paired plexiform longitudinal anastomoses that interconnect the six cervical intersegmental arteries. The basilar artery arises from paired plexiform arterial arcades designated the dorsal longitudinal neural arteries. The two dorsal longitudinal neural arteries eventually fuse to form the single basilar artery, so, in the adult, the two vertebral arteries unite to form one basilar artery.5
Internal Carotid Arteries
The cervical portions of the ICAs arise from the third aortic arch. The intracranial portions of the ICAs develop as an extension of the dorsal aortae.3
During embryologic development, the distal ICAs consist of cranial and caudal divisions. The paired cranial divisions initially terminate as the primitive olfactory arteries. These arteries give origin to the anterior cerebral arteries (ACAs), the anterior choroidal arteries, and the middle cerebral arteries (MCAs).6 The caudal divisions of the ICAs initially anastomose with the paired dorsal longitudinal neural arteries to form temporary connections between the vertebrobasilar circulation and the ICA. Portions of the caudal divisions anastomose with the cranial ends of the dorsal longitudinal neural arteries to give rise to the posterior communicating arteries (PCoAs). The remaining portions typically regress and disappear.2 On occasion, other portions of these caudal anastomoses persist into adulthood, giving rise to a group of unusual primitive carotid-basilar anastomoses.
Anterior Cerebral Arteries
At days 41 to 48 of gestation, the primitive olfactory artery gives off two branches, one directed toward the nasal fossa and the other directed medially. The medially directed vessel gives rise to the ACA. By the sixth week of gestation, both ACAs course toward the midline and connect to each other through a plexiform anastomosis.7 This plexus ultimately forms the anterior communicating artery (ACoA). The medial lenticulostriate arteries and the recurrent artery of Huebner are thought to arise from the primitive olfactory artery or the anastomosis between this artery and the primitive ACAs.6
Middle Cerebral Arteries
The MCAs develop from the primitive ICAs proximal to the ACAs. Branches of the MCAs extend over the cerebral hemispheres during days 47 to 48 of gestation. Initially, the MCA branches ascend almost vertically over the lateral surfaces of the early hemispheres. As the brain matures, and the opercula fold progressively over the insula, the MCA branches are constrained to fold with the brain, creating the looping adult course of the MCA across the insula, along the inner wall of the opercula, and then upward around the frontal and parietal opercula and downward over the temporal operculum.1
Posterior Cerebral Artery
The posterior cerebral arteries (PCAs) develop as continuations of the PCoAs. After the caudal divisions of the ICAs anastomose with the cranial ends of the dorsal longitudinal neural arteries, both regress to form the early PCoAs. Embryonic vessels arise from the caudal end of these PCoAs and then coalesce into the proximal segments of the PCAs. Over time, concurrent with the development of the vertebrobasilar system, the early PCoAs involute into the small adult PCoAs.1,3 In 20% to 30% of individuals, the PCoAs do not regress, so the posterior cerebral circulation continues to be supplied from the ICAs rather than from the vertebrobasilar system.8 In these cases, the PCoAs remain large in caliber and are designated “persistent fetal PCAs.”
Vertebrobasilar System
A series of longitudinal anastomoses connect six cervical intersegmental arteries, eventually giving rise to the vertebral arteries. Proximal connections to the dorsal aortae regress, except for the paired sixth intersegmental arteries.9 The sixth intersegmental arteries give rise to the subclavian arteries.9 Distally, the paired VAs supply the paired longitudinal neural arteries, which ultimately coalesce to form the single definitive basilar artery.
Connections between the carotid and basilar system exist in early fetal development. These connections are named for the cranial nerves with which they course and include the trigeminal artery, otic artery, and hypoglossal artery. An additional proatlantal intersegmental artery also connects the carotid with the vertebral arteries.10 In normal fetal development, these connections involute after the PCoAs form from the caudal ICAs.1
The branches of the vertebrobasilar system develop relatively late compared with the normal cerebral vasculature. The major cerebellar branches develop “top down,” first the superior cerebellar arteries (SCAs), then the anterior inferior cerebellar arteries (AICAs), and last the posterior inferior cerebellar arteries (PICAs). The vascular plexus supplying the primitive hindbrain persists late into embryologic development, allowing them time to develop a broad range of final vascular configurations.11
ARTERIAL SYSTEM
Anterior Arterial Circulation
Internal Carotid Artery
The ICAs originate at the bifurcation of the common carotid arteries in the neck, most commonly at the C3-4 or C4-5 level. Variability in the level of bifurcation of the common carotid arteries has been described, ranging from C1 to T2.12 The ICAs course upward through the anterior neck to the skull base and ascend through carotid canals within the petrous temporal bones to enter the intracranial space. The ICAs then pass forward over the intracranial surface of the foramen lacerum, course lateral to the sphenoid bone and sella turcica, ascend medial to the anterior clinoid processes, and enter the subarachnoid space just superior to the anterior clinoid processes. The ICAs terminate in the suprasellar cistern by bifurcating into the ACAs and MCAs. The long course of the ICA is typically subdivided into seven anatomic segments (Table 18-1 and Fig. 18-1).13
TABLE 18-1 Internal Carotid Artery Segments
| Segment | Course |
|---|---|
| C1 (cervical) | Extends from the origin of the internal carotid artery to its entry into the skull base |
| C2 (petrous) | Portion of the artery within the carotid canal of the petrous temporal bone |
| Initially, ascends vertically within the canal (vertical portion) and then turns anteriorly, medially, and superiorly within the canal (genu) and continues horizontally (horizontal portion) toward the petrous apex, where it exits the temporal bone | |
| C3 (lacerum) | Begins where the internal carotid artery exits from the carotid canal and extends up to the level of the petroclinoid ligament |
| C4 (cavernous) | Begins at the superior aspect of the petroclinoid ligament and includes the portion of the internal carotid artery that courses through the cavernous sinus |
| C5 (clinoid) | Short segment; courses through the dural reflections related to the anterior clinoid process |
| C6 (ophthalmic) | Begins at the distal dural reflection around the anterior clinoid process and extends to the level of the posterior communicating artery |
| C7 (communicating) | Begins just proximal to the origin of the posterior communicating artery and terminates where the internal carotid artery bifurcates into the anterior and middle cerebral arteries |
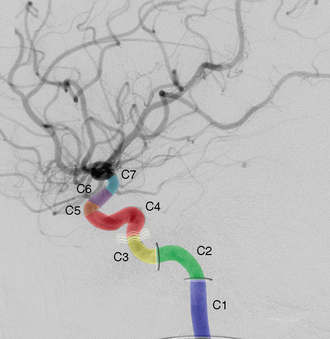
FIGURE 18-1 Lateral view of a carotid artery angiogram showing the seven segments of the internal carotid artery (ICA) from its origin to the bifurcation of the anterior and middle cerebral arteries. The cervical segment (C1) extends from the origin of the ICA to the petrous bone. As the ICA enters the petrous bone and carotid canal (horizontal oval) it becomes the petrous segment (C2). The artery then exits the carotid canal (vertical oval) and travels superior to the foramen lacerum as the lacerum segment (C3) extending to the level of the petrolingual ligament (curved lines). At the superior aspect of the ligament the ICA becomes the cavernous segment (C4). This segment has two vertical segments with an intervening horizontal segment. As the ICA courses through the dural reflections at the level of the anterior clinoid process it is termed the clinoid segment (C5). The distal portion of the dural reflection at the anterior clinoid gives rise to the ophthalmic segment (C6), which extends to the level just proximal to the origin of the posterior communicating artery. The communicating segment (C7) extends from the origin of the posterior communicating artery and terminates at the bifurcation of the ICA.
C1
The cervical segment of the ICA (C1) extends from the origin of the ICA to its entry into the skull base. C1 can be further subdivided into the proximal carotid bulb and the ascending segment distal to the bulb. The carotid bulb is a focal dilatation at the origin of the ICA. It commonly demonstrates turbulent flow dynamics at angiography.14 The ascending portion of C1 passes superiorly through the carotid space, accompanied, for parts of its course, by the external carotid artery (ECA), internal jugular vein, and cranial (CN) nerves IX, X, XI, and XII to the level of the skull base. No consistent anatomic branches arise from the ascending cervical segment of the ICA, although anomalous vessels have occasionally been reported to arise there. The ascending cervical ICA arises posterolateral to the ECA but gradually passes medial to the ECA as it ascends superiorly.
C2
The petrous segment of the ICA (C2) spans the course of the artery through the carotid canal of the petrous temporal bone. Initially, the petrous ICA ascends vertically within the canal (vertical portion of C2). It then turns anteriorly, medially, and superiorly within the canal (genu) and continues horizontally (horizontal portion) toward the petrous apex, where it exits the temporal bone.15 The petrous segment of the ICA lies just anterior and inferior, to the tympanic cavity and cochlea, separated only by a thin bony plate.16,17 The vidian artery and caroticotympanic artery may (variably) arise from the petrous ICA and may provide collateral flow from the ECA in cases of more proximal ICA occlusion.18
An aberrant petrous ICA segment may reflect a defect during embryogenesis. Abnormal involution or underdevelopment of the petrous ICA, and consequent collateral flow between the caroticotympanic artery and an augmented inferior tympanic artery, may establish an aberrant course of the ICA through the middle ear.19 Such an aberrant ICA may be confused with a vascular tumor, particularly a glomus tympanicum tumor.19,20 A persistent stapedial artery may arise from the vertical portion of the petrous ICA as an uncommon anomalous branch. The stapedial artery passes into the middle ear, courses across the footplate of the stapes, and terminates as the middle meningeal artery. The stapedial artery is typically not identified at digital angiography but may be seen on CT angiography as a focal defect in the lateral wall of the carotid canal, an enlarged geniculate fossa, and irregularity of the anterior epitympanic recess. An additional, indirect sign is hypoplasia or absence of the ipsilateral foramen spinosum.21,22
C4
The cavernous segment of the ICA (C4) begins at the superior aspect of the petroclinoid ligament and includes the sinuous portion that courses through the cavernous sinus. C4 initially ascends into the cavernous sinus (first vertical segment), where it lies medially. It then turns (first genu) to course horizontally within the cavernous sinus (horizontal segment), turns upward (second genu), and ascends as a shorter more lateral ascending vertical segment (second ascending segment).13 The posterior genu characteristically lies medial to the anterior genu. The cavernous portion of the ICA lies in close proximity to numerous anatomic structures. The sella turcica and sphenoidal sinus lie medial and inferomedial to the cavernous segment of the ICA. CN VI courses forward through the cavernous sinus along the lateral wall of C4, so it is often the first cranial nerve affected by aneurysms of the cavernous carotid artery. CN III, IV, V1, and V2 course within the lateral wall of the cavernous sinus lateral to C4. Meckel’s cave and the trigeminal ganglion lie just inferolateral to the cavernous sinus.23
Several important branches originate from the cavernous segment of the ICA. The meningohypophysial artery, also called the posterior trunk, arises from the posterior genu of C4 and gives rise to three major branches: the inferior hypophysial artery, the marginal tentorial artery, and the dorsal clival (meningeal) artery.24 The inferolateral trunk commonly arises from the horizontal portion of C4 and courses laterally to supply CN III, IV, and VI in addition to the trigeminal ganglion and the dura covering the cavernous sinus (Fig. 18-2).25 The inferolateral trunk also arises from C4. It gives off branches that anastomose with branches from the external carotid circulation, so the inferolateral trunk provides a route for collateral ECA-to-ICA flow around stenoses/occlusions of the cervical ICA.26
C6
The ophthalmic segment of the ICA (C6) begins at the distal dural reflection about the anterior clinoid process and extends to the level of the PCoA. The major branches arising from the C6 segment include the ophthalmic artery and the superior hypophysial artery. The ophthalmic artery typically arises from the medial aspect of the C6 segment and courses with the optic nerve through the optic canal into the orbit (Fig. 18-3).27 Occasionally, the ophthalmic artery may arise, instead, from the C5 segment of the ICA or from the middle meningeal artery.1 The ophthalmic artery gives rise to multiple ocular, orbital, and extraorbital branches. The ocular branches include the central retinal artery and ciliary arteries. The orbital branches include the lacrimal artery and muscular branches. The recurrent meningeal artery is a small branch of the lacrimal artery, which courses through the superior orbital fissure to anastomose with branches of the middle meningeal artery.28 The extraorbital branches include the supraorbital, anterior, and posterior ethmoidal, dorsal nasal, palpebral, medial frontal, and supratrochlear arteries.27 These generally anastomose with branches of the ECA, providing another route for collateral flow from the ECA to the ICA. The C6 segment also gives rise to the superior hypophysial artery. This artery arises from the medial aspect of C6, anastomoses with its contralateral counterpart, and forms a vascular plexus about the pituitary stalk. This plexus supplies the anterior pituitary gland, tuber cinereum, optic nerve, and optic chiasm.28
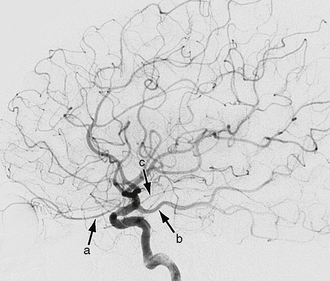
FIGURE 18-3 Lateral view from an internal carotid artery (ICA) angiogram shows three major branches of the distal ICA. The ophthalmic artery (a) is the first major branch that arises from the C6 or ophthalmic segment of the ICA. The communicating or C7 segment of the ICA gives rise to the posterior communicating artery (b) and anterior choroidal artery (c).
C7
The communicating segment of the ICA (C7) begins just proximal to the origin of the PCoA and terminates where the ICA bifurcates into the MCAs and ACAs. The first major branch of C7 is the PCoA. This arises from the posterior wall of the ICA and courses posteriorly through the suprasellar cistern to anastomose with the PCA (see Fig. 18-3). The size of the PCoA varies widely from aplastic to hypoplastic to enlarged. Large size suggests that the PCoA directly supplies the PCA territory as a persistent fetal PCA (Fig. 18-4).8 The origin of the PCoA often exhibits a focal enlargement, designated the infundibulum. To be considered an infundibulum, rather than an aneurysm, the focal dilatation must lie precisely at the origin of the PCoA, must be widest at its base, must not measure greater than 3 mm at its base, and must give rise to the rest of the vessel exactly at its apex (Fig. 18-5).29 CN III courses through the suprasellar cistern close to the PCoA, so it is often affected by aneurysms of the PCoA. The anterior thalamoperforating arteries arise from the PCoAs and course superiorly to supply portions of the medial hypothalamus, thalamus, and lateral aspect of the third ventricle.1
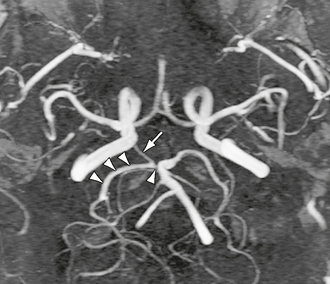
FIGURE 18-4 Collapsed maximal intensity projection (MIP) of a time-resolved contrast-enhanced MR angiogram. The right posterior communicating artery (arrow) is shown to provide dominant blood supply to the right P2 segment of the posterior cerebral artery (triple arrowheads). The P1 segment is hypoplastic (single arrowhead).

FIGURE 18-5 Lateral view of a carotid artery angiogram shows a focal conical dilatation (arrowhead) at the origin of the posterior communicating artery (arrow) representing an infundibulum.
The second major branch of C7 is the anterior choroidal artery. This arises from the posterior aspect of C7 just above the PCoA and proximal to the bifurcation of the ICA (see Fig. 18-3). Its long course is divided into three segments. The anterior choroidal artery first courses through the suprasellar cistern just medial to the uncus of the temporal lobe (cisternal segment). It then turns laterally and passes through the choroidal fissure to enter the temporal horn of the lateral ventricle. Within the ventricle, the anterior choroidal artery supplies the choroid plexus and courses posterosuperiorly with the choroid plexus up to and around the pulvinar of the thalamus. The point at which the anterior choroidal artery enters the choroid fissure is termed the plexal point. The segment of the artery distal to the plexal point is termed the plexal segment. The plexal segment is typically associated with the vascular blush of the choroid plexus on angiography.12 In its course, the anterior choroidal artery supplies the medial temporal lobe, the optic tract and lateral geniculate body, the dorsal globus pallidus, the inferior half of the posterior limb of the internal capsule, the lateral aspect of the cerebral peduncle, the tail of the caudate nucleus, and the choroid plexus.28
The circle of Willis is a vascular “ring” at the base of the brain, interconnecting segments from multiple individual vessels. When complete, it is made up of the two ICAs (C7 segments), the two precommunicating A1 segments of the ACAs, the ACoA, the two PCoAs, the two precommunicating (P1) segments of the PCAs, and the distal segment of the basilar artery (Fig. 18-6). The circle of Willis is complete in approximately 70% of patients and exhibits numerous anatomic variants of variable clinical significance.
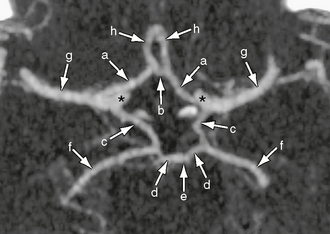
FIGURE 18-6 Axial maximum intensity projection image from a CT angiogram shows a complete circle of Willis, which interconnects segments from multiple individual arteries at the base of the brain. A complete circle of Willis is formed by two internal carotid arteries (asterisk), the two precommunicating A1 segments of the anterior cerebral arteries (a), the anterior communicating artery (b), the two posterior communicating arteries (c), the two precommunicating (P1) segments of the posterior cerebral arteries (d), and the basilar artery (e). The posterior cerebral (f), middle cerebral (g), and anterior cerebral (h) arteries are shown.
Anterior Cerebral Artery
The ACA is typically divided anatomically into three segments: the horizontal or precommunicating segment (A1), the vertical or postcommunicating segment (A2), and the more distal cortical branches (A3). The A1 segment follows an anteromedial, relatively horizontal course toward the midline interhemispheric fissure. It typically passes very close to the superior surface of the optic chiasm and/or the prechiasmal optic nerves. In the midline, A1 anastomoses with the ACoA. Distal to the ACoA, the A2 segment ascends through the cistern of the lamina terminalis and the interhemispheric fissure and gives rise to the pericallosal artery, callosomarginal artery, and distal branches (Table 18-2).
TABLE 18-2 Anterior Cerebral Artery Segments
| Segment | Course |
|---|---|
| A1 (precommunicating) | From the internal carotid artery bifurcation to the anastomosis of the anterior communicating artery |
| A2 (postcommunicating) | From anastomosis of the anterior communicating artery to termination into cortical branches |
| A3 (cortical branches) | Terminal cortical branches |
Perforating Branches
The ACA gives rise to numerous named perforating branches. Small branches from the ACoA supply the optic chiasm, infundibulum, hypothalamus, corpus callosum, septum pellucidum, and fornix.30 The medial lenticulostriate arteries arise from the A1 segment and pass superiorly into the brain via the anterior perforated substance. The recurrent artery of Huebner arises variably from A1, ACoA, or A2 and passes laterally and superiorly to enter the anterior perforated substance.31 As a group, the perforating branches of the ACA supply the head of the caudate nucleus, portions of the basal ganglia, and the anterior limb of the internal capsule. Additional perforating branches of the pericallosal artery supply portions of the corpus callosum.
Cortical Branches
The A2 segment gives rise to numerous cortical branches (Table 18-3). The orbitofrontal artery is the first cortical branch of the pericallosal artery. It supplies the undersurface of the frontal lobe, including the gyrus rectus, medial orbital gyrus, and olfactory bulb and tract. The frontopolar artery is the next cortical branch of the pericallosal artery. It supplies the anterior portion of the medial and lateral aspects of the superior frontal gyrus. The branching pattern of the more distal ACA is highly variable, with multiple different patterns of pericallosal and callosomarginal segments. In general, the pericallosal artery courses anterior to the lamina terminalis within the interhemispheric fissure to the level of the genu of the corpus callosum and continues posteriorly within the pericallosal cistern to the splenium, where it anastomoses with the posterior pericallosal branches of the posterior circulation.28 The pericallosal artery supplies cortical branches to the medial surface and convexities of the frontal and parietal lobes. Perforating branches arising from the pericallosal artery give blood supply to the corpus callosum, septum pellucidum, and fornix.
TABLE 18-3 Cortical Branches of the Anterior Cerebral Artery
| Division | Gives Supply to: |
|---|---|
| Orbitofrontal artery | Undersurface of frontal lobe—gyrus rectus, medial orbital gyrus, and olfactory bulb and tract |
| Frontopolar artery | Anterior portion of the medial and lateral aspects of the superior frontal gyrus |
| Terminal pericallosal and callosomarginal artery branches | Variable; supply cortical branches to the medial surface and convexities of the frontal and parietal lobes |
A callosomarginal artery is seen in approximately 50% of cerebral angiograms and passes posteriorly along the cingulate sulcus.1 It provides numerous cortical branches to the medial surfaces of the frontal and parietal lobes with variable extension onto the superior convexities.28
The ACA territory is substantial and typically includes at least the anterior two thirds of the medial interhemispheric cortex, in addition to a variable distribution along the cerebral convexities (Fig. 18-7).1,28
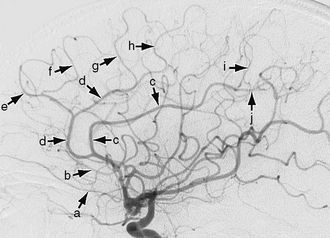
FIGURE 18-7 Lateral view of a carotid artery angiogram shows branches of the anterior cerebral artery (ACA). The orbitofrontal (a), frontopolar (b), pericallosal (c), callosomarginal (d), anterior internal frontal (e), middle internal frontal (f), posterior internal frontal (g), paracentral lobule artery (h), superior internal parietal (i), and inferior internal parietal (j) branches of the ACA are seen.
The ACA shows multiple anatomic variations. The A1 segment may be absent or hypoplastic. In such cases, the contralateral ACA provides blood supply to both hemispheres via two A2 segments (Fig. 18-8). Uncommonly, the ACA may arise from the C6 (ophthalmic) segment of the ICA and pass beneath, not above, the optic nerve. This infraoptic origin of the ACA has been associated with an increased incidence of intracranial aneurysms.32,33 The A2 segment may be hypoplastic or absent, with the single contralateral A2 supplying both A2 vascular distributions. Azygos ACA is seen in 0.2% to 3.7% of humans. The azygos portion of the ACA may run as a short or long trunk, with the short trunk bifurcating at the genu of the corpus callosum and the long trunk coursing nearly the entire extent of the corpus callosum.34 A completely azygous ACA is a single midline vessel supplying the ACA distributions bilaterally.35 This may be seen in association with holoprosencephaly and in association with aneurysmal dilatation of the azygous artery within a callosal lipoma.1,
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




