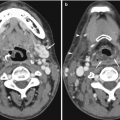
Fig. 4.1
A 65-year-old man with esophageal carcinoma. Tc-99m diphosphonate bone scintiscans done for staging show abnormal soft tissue visualization of the stomach as well as the thyroid gland, consistent with free dissociated pertechnetate
4.2.1.2 Drug Interactions with Radiopharmaceuticals
It is well known that various drugs or substances in vivo can cause scan deviations and artifacts. Some of the well-documented interactions are listed below:
In bone scan imaging using Tc-99m diphosphonates, it is well known that increased kidney uptake of bone tracer and prominent renal visualization can be due to various types of administered cytotoxic drugs such as cisplatin, doxorubicin, and cyclophosphamide, as well as the presence of aluminum and ferrous ions. Increased liver visualization may be due to iron excess.
In thyroid imaging using Tc-99m pertechnetate or I-123 or I-131 iodide, exogenous thyroxine and high iodine-containing substrates such as intravenous (IV) contrast agents and amiodarone can suppress uptake. In I-123 or I-131 MIBG imaging, various drugs are documented to affect the uptake of MIBG. These include tricyclic antidepressants, phenothiazines, opiates, calcium channel blockers, and angiotensin-converting enzyme inhibitors (Bomardieri et al. 2010).
For labeling of red blood cells with Tc-99m pertechnetate for MUGA or gastrointestinal bleeding studies, it is known that reduced efficiency of red cell labeling has been reported with heparin, tin overload, aluminum, prazosin, methyldopa, hydralazine, digoxin, quinidine, beta-blockers, calcium channel blockers, nitrates, anthracycline antibiotics, and IV contrast agents. In particular, it has been advised that red cell labeling be performed prior to IV contrast administration as labeling efficiency may be severely affected (Corbett et al. 2006).
For PET imaging, FDG uptake in tumors may be reduced in the presence of high blood glucose or use of steroids.
4.2.2 Technical Pitfalls: Scanning Procedure and Scanner Factors
Scan technical factors may give rise to pitfalls in images. These are related to the scanning procedure and scanner and include inadvertent deposition of tracer on parts of the body, clothing, scanner, metallic objects causing attenuation artifacts, scanner defects such as defective photomultiplier tube, erroneous setting for pulse height analyzer leading to image degradation, counts overflow, patient motion artifacts, attenuation artifacts, presence of other radiotracers, use of inappropriate collimator, poor ECG gating, and misaligned center of rotation. Some of these factors are discussed further below.
4.2.2.1 Unintended Tracer Deposition in Body, Clothing, and Scanner
This is one of the most common pitfalls in nuclear medicine imaging, causing scan artifacts that resemble focal lesions. Deposition of tracer can occur due to inadvertent spray of tracer during injection at an improperly secured injection port or due to urinary contamination or salivary secretions. A common occurrence is the appearance of a focal uptake seen in the chest in a radioiodine (I-123 or I-131) whole body scan, in which the abnormality is not to any structural lesion but from a small collection of swallowed activity in the esophagus. Tracer contamination has been observed in the hair, ears, chest wall, abdominal wall, and pelvic regions as well as in the extremities (Fig. 4.2). Occasionally, these cause interpretive challenges that may have to be resolved by re-scanning the patient after the tracer contamination is removed (e.g., by washing). A very common occurrence is the presence of a focus of tracer activity in the extremities, due to slight tracer extravasation at the injection site or a collection in a tortuous vessel. Another scan artifact is due to tracer in a long peripheral line or central line that had not been adequately flushed with normal saline after tracer injection. This may occasionally cause confusion in scan interpretation or obscure structures.
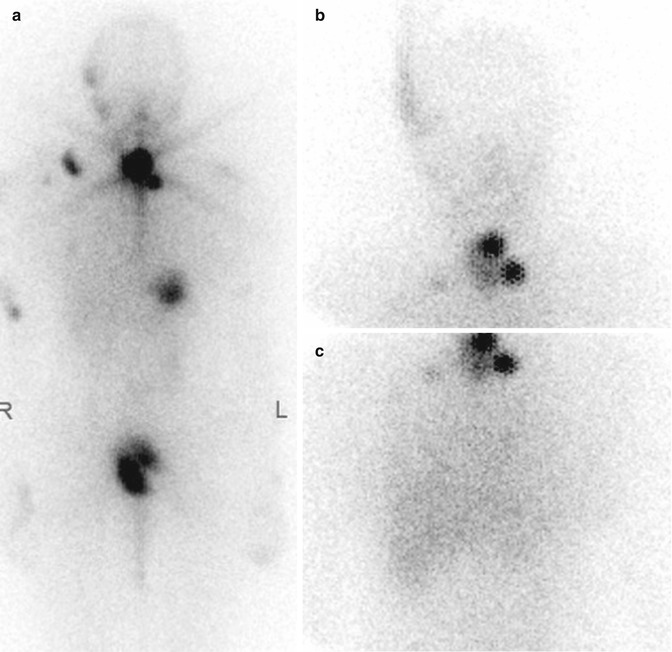
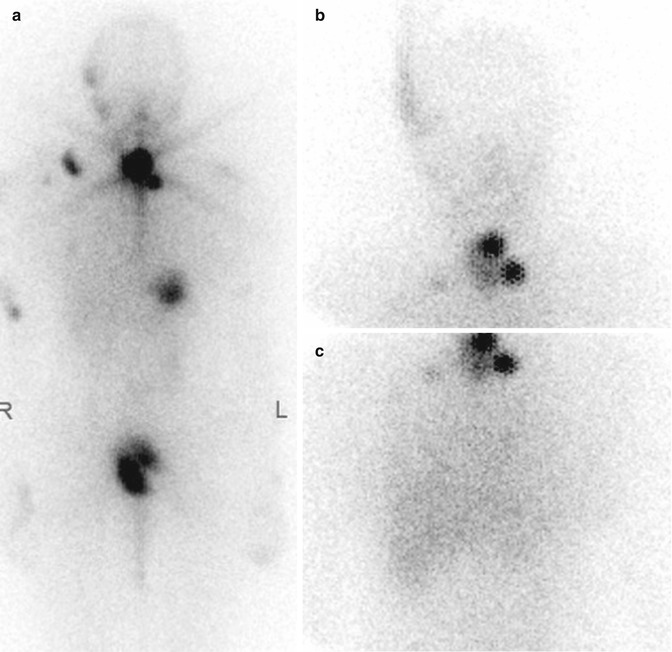
Fig. 4.2
A 33-year-old woman with papillary thyroid carcinoma, status post total thyroidectomy with left neck dissection. Recent neck CT showed left TEG recurrence. Redo left TEG clearance and neck dissection were performed. (a) Whole body Tc-99m diphosphonate bone scintiscan shows artifacts due to iodine-131 contamination in the hair, face, and chest. (b, c) Subsequent images repeated 1 day later, after washing and cleaning, show much less contamination and disappearance of most of the scan artifacts
4.2.2.2 Metallic Objects
Photopenic (photon-deficient) defects can be seen on the various kinds of nuclear medicine scans, more commonly in bone scans, due to attenuation from metallic or dense objects. These include pacemakers (Fig. 4.3), buttons, buckles, jewelry bangles, coins in pockets, breast prostheses, and orthopedic prostheses. Patients should be informed to remove these objects if clinically possible before the scan is started. Occasionally, they cause confusion with osteolytic lesions or obscure parts of the scan.
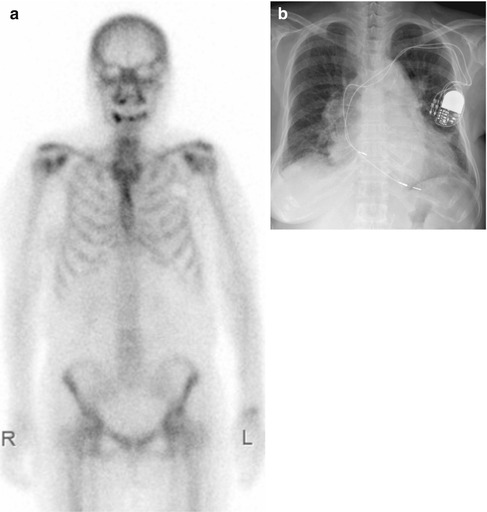
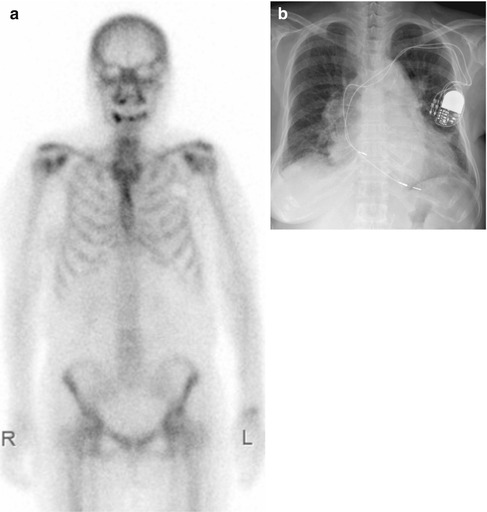
Fig. 4.3
A 74-year-old woman with left breast carcinoma, status post simple mastectomy and axillary clearance. (a) Tc-99m diphosphonate bone scintiscan shows a photopenic defect over the left upper chest wall that is due to a pacemaker. (b) The corresponding chest radiograph confirms presence of the pacemaker
4.2.2.3 Patient Motion Artifacts
Patient motion may introduce loss of resolution of the image and scan artifacts. This is particularly important in myocardial perfusion imaging and renography imaging. Patient motion in a renography study will typically cause artifactual abnormalities on the time-activity curves, and care must be exercised in reducing this possibility. In myocardial perfusion imaging, patient motion may give rise to apparent perfusion defects. Patient motion can be detected by cine displays, sinograms, and summed planar images. There are a number of software algorithms for correcting patient motion, but the best way to avoid this pitfall is to be aware of its possible occurrence and minimize patient motion or to repeat the study if suspected.
4.2.2.4 Presence of Other Tracers
Occasionally, a patient may have performed two nuclear medicine imaging studies within a short period of time, such that the images superimpose. This produces the occasional unusual scan appearance that can be misleading. For example, a Tc-99m diphosphonate bone scan that is performed within 24 h of a myocardial perfusion imaging using Tc-99m sestamibi will show apparent cardiac, hepatic, thyroid, and bowel uptake of “bone” tracer. Sometimes, when a bone scan is performed 1 week after a patient has received therapeutic activity of I-131 for thyroid remnant ablation, the high energy photons of iodine-131 will cause septal penetration and obscure the Tc-99m bone scan image.
4.2.2.5 Misalignment of the Center of Rotation in SPECT
Center of rotation error occurs when the point of reference used by the scanner in reconstructing images is not aligned with the mechanical axis of the SPECT scanner. If the center of rotation is properly calibrated, a radioactive point source placed at the center of the camera orbit should project to the center of the reconstructed image. Errors of misalignment of the center of rotation may manifest as areas of reduced counts or ring artifacts which may mimic true defects. It is important for nuclear medicine technologists to properly calibrate the center of rotation for the scanner on a routine basis as a quality control procedure.
4.2.3 Clinical/Interpretation Pitfalls
Clinical/interpretation pitfalls include failure to recognize variation of normal (including age-related normal variations), effects due to clinical conditions (such as right–left systemic shunt, ectopic organs, or presence of other concomitant disorders) or drugs, effects due to prior treatment such as radiotherapy and chemotherapy (such as flare response), and specific interpretative false-positives and false-negatives in various types of nuclear medicine imaging.
4.2.3.1 Age-Related Factors (Including Children)
Nuclear medicine imaging in the young can be fraught with subtleties. For example, bone scans in the young up to 20 years old typically demonstrate increased epiphyseal plate activity, and this requires care in interpretation as some of these may mimic trauma or conceal subtle changes of trauma. In younger subjects, increased tracer uptake at the manubriosternal junction is often a normal variant. In some patients, a small photopenic defect in the inferior aspect of the sternal body due to incomplete fusion of the cartilaginous bars can be seen. This photopenic area, called the sternal foramina, is typically surrounded by uniform radioactivity and should not be mistaken for an osteolytic lesion. Horizontal lines of uptake in the sternal body can also be seen in younger subjects, and these are often very uniform, regular spaced, and are in keeping with bone fusion centers in a growing sternum.
Radiotracer changes due to degeneration can often be seen in the older subjects. Focal irregularities in uptake of bone tracer can be seen at the knees due to osteoarthritis or in the lumbar spine due to spondylosis. They tend to have usual appearance of distribution at the joint surfaces and at the margins of the vertebrae or facet joints. Most of these pattern if equivocal on planar imaging can be further characterized with SPECT-CT.
The uptake of FDG or radiotracers for cerebral amyloid imaging by the cerebral hemispheres and deep cerebral structures may show age-related changes, and experience and care should be exercised. Cortical FDG uptake decreases with age, particularly in the frontal lobes. In contrast, metabolic activity of the basal ganglia, visual cortices, and cerebellum remains unchanged. The normal thymus may be visualized on a routine FDG PET-CT as an FDG-avid anterior mediastinal mass in a young person. Occasionally, the normal thymus or lactating breasts can be visualized on the I-123/I-131 whole body scan (Fig. 4.4).
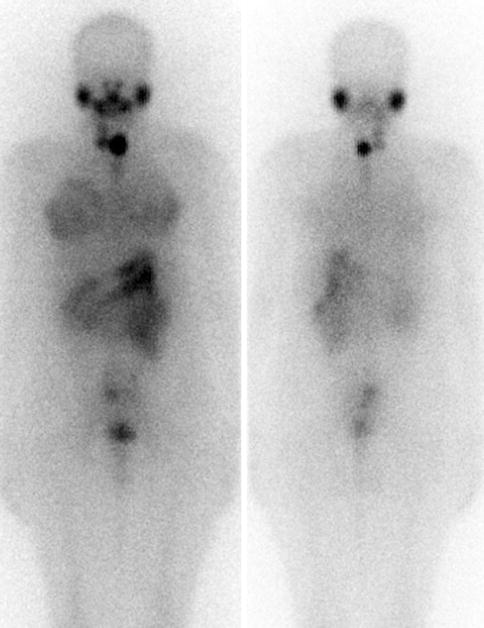
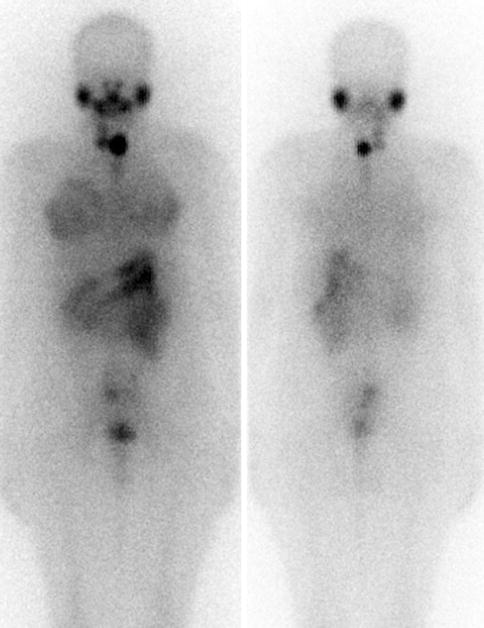
Fig. 4.4
A 27-year-old woman with papillary thyroid carcinoma with nodal metastases, status post total thyroidectomy, central neck and right modified radical neck dissection. She was 3 months’ postpartum when this post-therapy whole body Tc-99m diphosphonate bone scintiscan was performed and had stopped breastfeeding for at least 1 month prior. The images show I-131 uptake projected over the chest due to lactating breast uptake
4.2.3.2 Right–Left Systemic Shunt
In V/Q lung scanning, the radiotracers used are typically Xe-133 gas, Tc-99m Technegas, or Tc-99m DTPA aerosol for ventilation and Tc-99m MAA for perfusion. The particle size for Tc-99m MAA is usually 20–80 μm and largely trapped in the pulmonary capillary vasculature. Only less than 4 % of administered MAA activity escapes into the systemic circulation. This small amount of radioactivity is usually not visually detectable. Routinely, minimal or no kidney activity is visualized in both the ventilation and perfusion images. The visualization of the kidney, thyroid, and brain cerebral hemispheres after the injection of Tc-99m MAA is thus highly indicative of a right–left systemic shunt. Care must be taken in attributing thyroid and kidney uptake to systemic shunting as these may be seen if free pertechnetate is present.
4.2.3.3 Ectopic Locations
Ectopic organs are potential sources of interpretation errors. Examples include ectopic thyroid gland in the lingual or hyoid position (Fig. 4.5), ectopic kidney in the pelvis, and ectopic parathyroid adenomas in the mediastinum. A transplanted kidney seen in the iliac fossa can be missed or mistaken for bone pathology (Fig. 4.6).
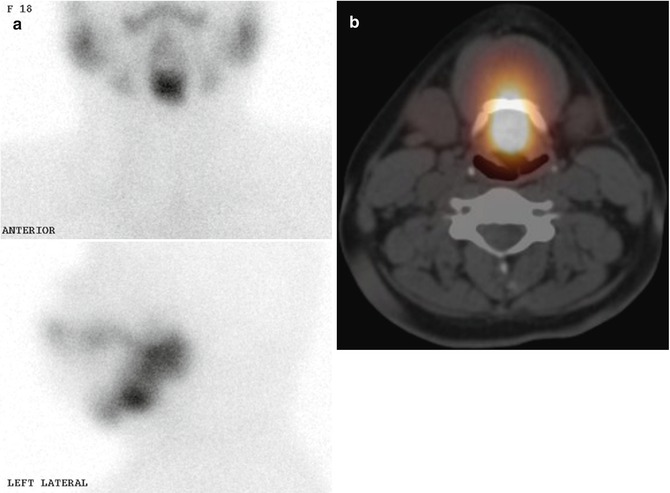

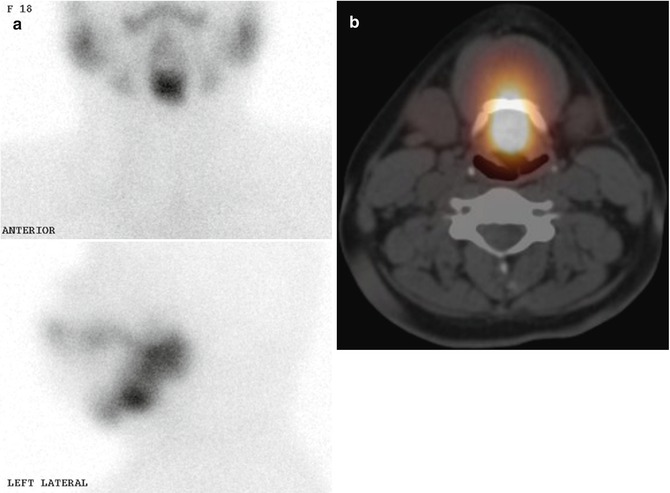
Fig. 4.5
(a) Anterior and lateral planar Tc-99m pertechnetate images show absence of thyroid gland in the usual anatomic position. However, there is a midline upper neck focal uptake (seen between the submandibular glands) which is abnormal. This appearance of focal Tc-99m pertechnetate uptake in this location is highly indicative of ectopic thyroid (lingual or hyoid thyroid). (b) SPECT-CT image shows the submental nodule with tracer uptake, suggestive of a hyoid thyroid

Fig. 4.6
Tc-99m diphosphonate bone scintiscans show a transplanted kidney in the right iliac fossa, partially obscuring the right iliac bone and appearing as a tracer-avid focus. There is also non-visualization of the native kidneys likely related to renal failure, bilateral femoral prostheses, and spondylitic changes in the lumbar spine
4.2.3.4 Clinical Conditions Causing Possible Interpretative Errors During Bone Scans
Extraosseous Uptake
For bone scans, extraosseous uptake can occasionally be identified and is important for correct interpretation. Common causes of extraosseous uptake have been well tabulated by Gnanasegaran et al. (2009). Foci of soft tissue bone tracer uptake causing interpretive difficulties may be caused by non-osseous metastases from osteosarcoma and liposarcoma or even in primary tumors such as breast carcinoma. Additionally, extraosseous uptake of bone tracer may occasionally cause interpretative pitfalls and difficulties, including:
Cardiac focal uptake – caused by myocardial necrosis, myocardial contusion, ventricular aneurysm, and diffuse uptake can be seen in amyloidosis, hypercalcemia, alcoholic cardiomyopathy, and pericarditis.
Skeletal muscle uptake can be observed in trauma, excessive muscular activity, polymyositis, dermatomyositis, scleroderma, and heterotopic ossification after trauma or paralysis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree