SPECT generates transverse images depicting the distribution of x- or
γ-ray-emitting nuclides in patients. Standard planar projection images are acquired from an arc of 180° (most cardiac SPECT) or 360° (most non-cardiac SPECT) about the patient. Although these images could be obtained by any collimated imaging device, the vast majority of SPECT systems use one or more camera heads that revolve around the patient. The SPECT system’s digital computer then reconstructs the transverse images using either filtered backprojection or an iterative reconstruction method, which are described later in this chapter, as does the computer in an x-ray CT system.
Figure 19-1 shows a variety of SPECT systems.
Image Acquisition
The camera head or heads of a SPECT system revolve around the patient, acquiring projection images. The head or heads may acquire the images while moving
(continuous acquisition) or may stop at predefined evenly spaced angles to acquire the images (“step and shoot” acquisition). If the camera heads of a SPECT system produced ideal projection images (
i.e., no attenuation by the patient and no degradation of spatial resolution with distance from the camera), projection images from opposite sides of the patient would be mirror images, and projection images over a 180° arc would be sufficient for transverse image reconstruction. However, in SPECT, attenuation greatly reduces the number of photons from activity in the half of the patient opposite the camera head, and this information is greatly blurred by the distance from the collimator. Therefore, for most non-cardiac studies, such as bone SPECT, the projection images are acquired over a complete revolution (360°) about the patient. However, most nuclear medicine laboratories acquire cardiac SPECT studies, such as myocardial perfusion studies, over a 180° arc symmetric about the heart, typically from the 45° right anterior oblique view to the 45° left posterior oblique view (
Fig. 19-2). The 180° acquisition produces reconstructed images of superior contrast and resolution because the projection images of the heart from the opposite 180° have poor spatial resolution and contrast due to greater distance and attenuation. Although studies have shown that the 180° acquisition can introduce artifacts (
Liu et al., 2002), the 180° acquisition is more commonly used than the 360° acquisition for cardiac studies.
SPECT projection images are usually acquired in either a 642 or a 1282 pixel format. Using too small a pixel format reduces the spatial resolution of the projection images and of the resultant reconstructed transverse images, due to too large physical pixel dimensions. (A zoom factor of ˜1.5 is often employed for 642 cardiac SPECT, to reduce the pixel dimensions, thereby improving spatial resolution.) When the 642 format is used, typically 60 or 64 projection images are acquired and, when a 1282 format is chosen, 120 or 128 projection images are acquired. Using too few projections creates radial streak artifacts in the reconstructed transverse images.
The camera heads on older SPECT systems followed circular orbits around the patient while acquiring images. Circular orbits are satisfactory for SPECT imaging of the brain, but cause a loss of spatial resolution in body imaging because the circular orbit causes the camera head to be many centimeters away from the surface of the body during the anterior and perhaps the posterior portions of its orbit (
Fig. 19-3). Modern SPECT systems provide non-circular orbits (also called “body contouring”) that keep the camera heads in close proximity to the surface of the body throughout the orbit. For some systems, the technologist specifies the non-circular orbit by placing the camera head as close as possible to the patient at several angles, from which the camera’s computer determines the orbit. Other systems perform automatic body
contouring, using sensors on the camera heads to determine their proximity to the patient at each angle.
In brain SPECT, it is usually possible for the camera head to orbit with a much smaller radius than in body SPECT, thereby producing images of much higher spatial resolution. In many older cameras, a large distance from the physical edge of the camera head to the useful portion of the detector often made it impossible to orbit at a radius within the patient’s shoulders while including the base of the brain in the images. These older systems were therefore forced to image the brain with an orbit outside the patient’s shoulders, causing a significant loss of resolution. Most modern SPECT systems permit brain imaging with orbits within the patient’s shoulders, although a patient’s head holder extending beyond the patient table is generally necessary.
Transverse Image Reconstruction
After the projection images are acquired, they are corrected for non-uniformities and for center-of-rotation (COR) misalignments. (These corrections are discussed below, “Quality Control in SPECT.”) Following these corrections, transverse image reconstruction is performed using either filtered backprojection or iterative methods.
As described in
Chapter 10, filtered backprojection consists of two steps. First, the projection images are mathematically filtered. Then, to form a particular transverse image (also known as a slice), simple backprojection is performed of the row of each projection image corresponding to that transverse image. For example, the fifth row of each projection image is backprojected to form the fifth transverse image. A SPECT study produces transverse images covering the entire field of view (FOV) of the camera in the axial direction from each revolution of the camera head or heads.
Mathematical theory specifies that the ideal filter kernel, when displayed in the spatial frequency domain, is the ramp filter (
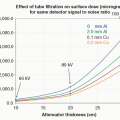
Fig. 19-4). (The spatial frequency domain is discussed in Appendix G, Convolution and Fourier Transforms.) However, the actual projection images contain considerable statistical noise, from the random nature of radioactive decay and photon interactions, due to the relatively small number of counts in each pixel. If the images were filtered using a ramp filter kernel and then backprojected, the resultant transverse images would contain an unacceptable amount of statistical noise.
In the spatial frequency domain, statistical noise predominates in the highfrequency portion. Furthermore, the spatial resolution characteristics of the gamma camera cause a reduction of higher spatial frequency information that increases with the distance of the structure being imaged from the camera. To smooth the projection images before backprojection, the ramp filter kernel is modified to “roll-off” at
higher spatial frequencies. Unfortunately, this reduces the spatial resolution of the projection images and thus of the reconstructed transverse images. A compromise must therefore be made between spatial resolution and the statistical noise of the transverse images.
Typically, a different filter kernel is selected for each type of SPECT study; for example, a different kernel would be used for Tc-99m HMPAO brain SPECT than would be used for Tc-99m sestamibi myocardial perfusion SPECT. The choice of filter kernel for a particular type of study is determined by the amount of statistical noise in the projection images (mainly determined by the injected activity, collimator, and acquisition time per image) and their spatial resolution (determined by the collimator and distances of the camera head(s) from the organ being imaged). The preference of the interpreting physician regarding the appearance of the images also plays a role. Projection images of better spatial resolution and less quantum mottle require a filter with a higher spatial frequency cutoff to avoid unnecessary loss of spatial resolution in the reconstructed transverse images, whereas projection images of poorer spatial resolution and greater quantum mottle require a filter with a lower spatial frequency cutoff to avoid excessive quantum mottle in the reconstructed transverse images. Although the SPECT camera’s manufacturer may suggest filters for specific imaging procedures, the filters are usually empirically optimized in each nuclear medicine laboratory.
Figure 19-5 shows a SPECT image created using three different filter kernels, illustrating too much smoothing, proper smoothing, and no smoothing.
Filtered backprojection is computationally efficient. However, it is based upon the assumption that the projection images are perfect projections of a three-dimensional object. As discussed in the previous chapter, this is far from true in gamma camera imaging, mainly because of attenuation of photons in the patient, the inclusion of Compton scattered photons in the image, and the degradation of spatial resolution with distance from the collimator.
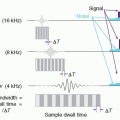
In SPECT, iterative reconstruction methods are increasingly being used instead of filtered backprojection. In iterative methods, an initial activity (typically uniform) distribution in the patient is assumed. (Alternatively, an activity distribution created by simple backprojection could be used.) Then, projection images are calculated
from the initial assumed activity distribution, using a model of the imaging characteristics of the gamma camera and the patient. The calculated projection images are compared with the actual projection images and, based upon this comparison, the assumed activity distribution is adjusted. This process is repeated several times, with successive adjustments to the assumed activity distribution, until the calculated projection images approximate the actual projection images (
Fig. 19-6).
As was stated above, in each iteration, projection images are calculated from the assumed activity distribution. The calculation of projection images can incorporate the system resolution point spread function (PSF) of the gamma camera, which takes into account the decreasing spatial resolution with distance from the camera face. If a map of the attenuation characteristics of the patient is available, the calculation of the projection images can include the effects of attenuation. Furthermore, the PSF can be modified to incorporate the effect of photon scattering in the patient. Alternatively,
modeling scatter within the photopeak based on either secondary energy window images (dual- or triple-energy-window method) or projection using the photopeak transverse images and attenuation and material density maps (effective scatter source estimation) is now more commonly applied. If all this is done, iterative methods will partially compensate for the effects of decreasing spatial resolution with distance, as well as attenuation and photon scattering in the patient. Iterative reconstruction can be used to produce higher quality tomographic images than filtered backprojection, or it can be used to produce images of similar quality to those produced by filtered backprojection, but with less administered activity or shorter acquisition times.
Iterative methods are computationally less efficient than filtered backprojection. However, the increasing speed of computers, the small image matrix sizes used in nuclear imaging, and the development of computationally efficient algorithms, such as the ordered-subset expectation maximization method (
Hudson and Larkin, 1994), have made iterative reconstruction feasible for SPECT. Since iteratively reconstructed SPECT transverse images will contain substantial noise due to relatively poor counting statistics, three-dimensional spatial filtering is commonly applied after reconstruction for noise reduction.
Attenuation Correction in SPECT
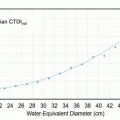
Radioactivity whose x- or
γ-rays must traverse long paths through the patient produces fewer counts, due to attenuation, than does activity closer to the surface of the patient adjacent to the camera. For this reason, transverse slices of a phantom with a uniform activity distribution, such as a cylinder filled with a well-mixed solution of radionuclide, will show a gradual decrease in activity toward the center (
Fig. 19-7, on the left). Attenuation effects are more severe in body SPECT than in brain SPECT.
Approximate methods are available for attenuation correction. One of the most common, the Chang method, presumes a constant attenuation coefficient throughout the patient (
Chang, 1978). Approximate attenuation corrections can overcompensate or undercompensate for attenuation. If such a method is to be used, its proper functioning should be verified using phantoms before its use in clinical studies.
These methods are only appropriate for filtered backprojection reconstruction. Furthermore, attenuation is not uniform in the patient, particularly in the thorax, and these approximate methods cannot compensate for non-uniform attenuation.
In the 1990s, several manufacturers provided SPECT cameras with sealed radioactive sources (commonly containing Gd-153, which emits 97 and 103-keV γ-rays) to measure the attenuation through the patient. The sources were used to acquire transmission data from projections around the patient. After acquisition, the transmission projection data were reconstructed to provide maps of tissue attenuation characteristics across transverse sections of the patient, similar to x-ray CT images. Finally, these attenuation maps were used during an iterative SPECT image reconstruction process to provide attenuation-corrected SPECT images.
The transmission sources were available in several configurations. These included scanning collimated line sources that were used with parallel-hole collimators, arrays of fixed line sources used with parallel-hole collimators, and a fixed line source located at the focal point of a fan-beam collimator.
The transmission data were usually acquired simultaneously with the acquisition of the emission projection data because performing the two separately can pose significant problems in the spatial alignment of the two data sets and greatly increases the total imaging time. The radionuclide used for the transmission measurements was chosen to have primary γ-ray emissions that differed significantly and were lower in energy from those of the radiopharmaceutical. Separate energy windows were used to differentiate the photons emitted by the transmission source from those emitted by the radiopharmaceutical. However, scattering of the higher energy emission photons in the patient and in the detector caused some cross-talk in the lower energy window.
Major manufacturers of nuclear medicine imaging systems now provide systems combining two camera heads capable of planar imaging and SPECT and an x-ray CT scanner, with a single patient bed. These systems have supplanted systems with radioactive transmission sources, and are referred to as SPECT/CT systems. In SPECT/CT systems, the x-ray CT attenuation image data can be used to correct the radionuclide emission data for attenuation by the patient. This is discussed in more detail later in this chapter.
Attenuation correction using radioactive transmission sources and x-ray CT-derived attenuation maps has been extensively studied in myocardial perfusion SPECT, where attenuation artifacts can mimic perfusion defects. These studies have shown that attenuation correction reduces attenuation artifacts and produces modest improvement in diagnostic performance when the studies are read by experienced clinicians (
Hendel et al., 2002;
Masood et al., 2005). However, other studies have shown that attenuation correction can cause artifacts, particularly when there is spatial misalignment of the emission data with respect to the attenuation maps determined from the transmission information. Furthermore, a period of transition is required, for even experienced clinicians to retrain themselves to interpret attenuation-corrected images. Therefore, it remains common for SPECT myocardial perfusion imaging to be performed without attenuation correction, although that may change with the increasing implementation of cardiac SPECT/CT.
Generation of Coronal, Sagittal, and Oblique Images
The pixels from the transverse slices may be reordered to produce coronal and sagittal slices. For cardiac imaging, it is desirable to produce oblique images oriented either parallel (vertical and horizontal long-axis images) or perpendicular (short-axis images) to the long axis of the left ventricle. Because there is considerable anatomic variation among patients regarding the orientation of the long axis of the left ventricle, the long axis of the heart must be determined before the computer can create the oblique images. This task is commonly performed manually by a technologist, although the software on most systems is now capable of correct automatic reorientation of myocardial perfusion images, with operator verification and override.
Collimators for SPECT
Most SPECT is performed using parallel-hole collimators. However, specialized collimators have been developed for SPECT. The fan-beam collimator, shown in
Figure 19-8, is a hybrid of the converging and parallel-hole collimator. Because it is a parallel-hole collimator in the
y-direction, each row of pixels in a projection image corresponds to a single transaxial slice of the subject. In the
x-direction, it is a converging collimator, with spatial resolution and efficiency characteristics superior to those of a parallel-hole collimator (see
Fig. 18-12). Because a fan-beam collimator is a converging collimator in the cross-axial direction, its FOV decreases with distance from the collimator. For this reason, the fan-beam collimator is mainly used for brain SPECT; if the collimator is used for body SPECT, portions of the body are excluded from the FOV, which can cause artifacts, called “truncation artifacts,” in the reconstructed images. One manufacturer offers a variable-focal-length converging collimator for cardiac imaging, where the focal length increases from the center outward, ending up as a parallel-hole collimator at the edge (to eliminate truncation artifacts), in both the transaxial and axial directions. Along with a heart-centric camera head orbit, an approximate factor of four improvement in sensitivity in the region of the heart is achieved (
Fig. 19-9).
Multihead SPECT Cameras
To reduce the limitations imposed on SPECT by collimation and limited time per view, camera manufacturers provide SPECT systems with two camera heads that revolve around the patient (
Fig. 19-1) and, in the past, SPECT systems with three heads were commercially available from at least two manufacturers. The use of multiple camera heads permits the use of higher resolution collimators, for a given level of quantum mottle in the tomographic images, than would a single head system. However, the use of multiple camera heads poses considerable technical challenges for the manufacturer. It places severe requirements upon the electrical and mechanical stability of the camera heads. In particular, the
X and
Y offsets and
X and
Y magnification factors of all the heads must be precisely matched throughout the rotation about the patient. Today’s multihead systems are very stable and provide high-quality tomographic images for a variety of clinical applications.
Multihead gamma cameras are available in several configurations. Double-head cameras with opposed heads (180° head configuration) are good for head and body SPECT and whole-body planar scans (
Fig. 19-1A and B). Triple-head, fixed-angle cameras are good for head and body SPECT, but less suitable for whole-body planar scans because
of the limited width of the crystals. Double-head, variable-angle cameras are highly versatile, capable of head and body SPECT and whole-body planar scans with the heads in the 180° configuration and cardiac SPECT in the 90° configuration (
Fig. 19-1C and D). (The useful portion of the crystal does not extend all the way to the edge of a camera head. If the two camera heads are placed at an angle of exactly 90° to each other, both heads cannot be close to the patient without parts of the patient being outside of the FOVs. For this reason, one manufacturer provides the option of SPECT acquisitions with the heads at a 76° angle to each other, as well as zoom from the corner where the two heads meet instead of in the center of the two detectors’ FOVs.)
Multielement Detector SPECT Cameras
SPECT systems that employ a multitude of small or curved detectors and alternative scanning techniques, as opposed to conventional rotating gantry SPECT scanners with two or three large FOV detectors, are now commercially available. Spectrum Dynamics Medical’s Veriton is a general-purpose (energy range 40-220 keV) scanner that has twelve detectors equally spaced over 360° around the patient. Each detector consists of a 6-mm-thick rectangular CZT crystal with 16 (transaxial dimension) × 128 (axial dimension), 2.46 mm × 2.46 mm detector elements, and an integrated parallel-hole tungsten collimator. Scanning of each (31.5 cm axial) SPECT FOV is achieved by a combination of detector swivel, rotation, and auto-contouring, with an increase in volume sensitivity on the order of 3 times compared to a conventional large FOV, dual-detector rotating gantry SPECT with LEHR collimation (
Fig. 19-10). A scanner dedicated to cardiac SPECT, the NM530c from GE Healthcare, contains nine 8 cm × 8 cm and 5-mm-thick CZT crystals with 2.46 mm × 2.46 mm elements, equally spaced along a stationary L-shaped gantry. Strategic orientation of each detector and pinhole collimation allows all views to be acquired simultaneously without detector motion, resulting in an approximate fivefold increase in counting efficiency compared to conventional NaI(Tl)-LEHR (
Fig. 19-11A and B). Spectrum Dynamics Medical also developed a dedicated cardiac CZT SPECT scanner (D-SPECT) Cardio, with nine 4 cm × 16 cm and 6 mm thick crystals, with 2.46 mm × 2.46 mm elements and parallel-hole tungsten collimation, in an L-shaped gantry, where scanning of the heart is achieved by translation and swivel of each detector, resulting in an approximate eightfold increase in sensitivity (
Fig. 19-11C and D). A
third, NaI(Tl)-based dedicated cardiac SPECT scanner is CardiArc Inc.’s CardiArc, which employs three adjacent curved crystals and an array of PMTs. “Slit-hole” scanning is performed, whereby one series of lead sheets with horizontal gaps remains stationary while a curved lead sheet with six vertical slits rotates back and forth in electronic synchrony with six corresponding regions of the crystals, resulting in a sensitivity gain of about four.