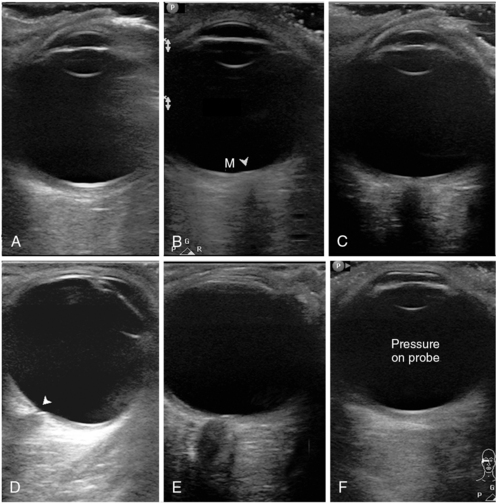
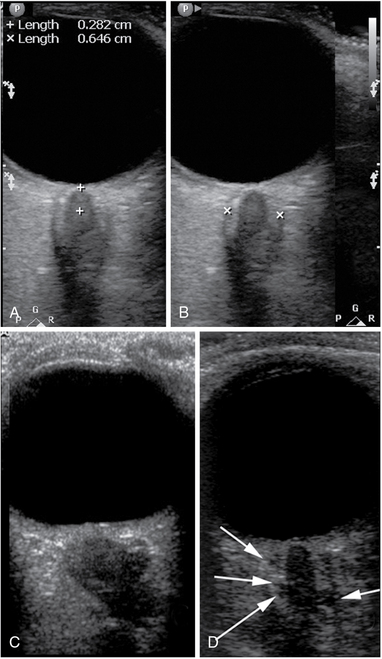
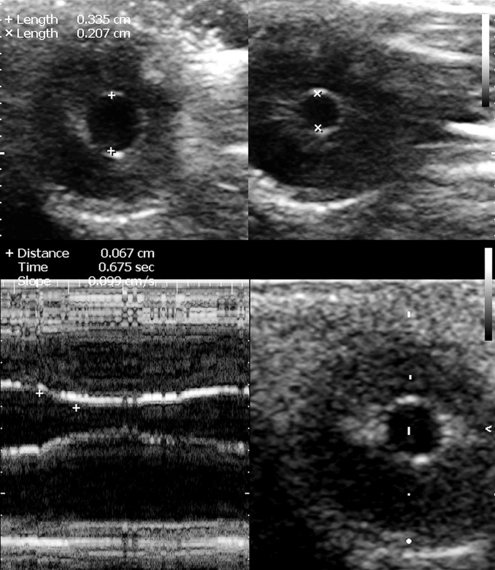
6 Multipurpose ultrasound systems offer a variety of eye and orbit imaging techniques relevant to critical care. Bedside ocular ultrasound can be used for the following purposes: (1) timely identification of threats to ocular health and vision and prevention of vision-related disability in trauma,1–4 (2) assessment of nontraumatic acute change in vision and the need for immediate ophthalmologic consultation,1 (3) measurement of the diameter of the optic nerve sheath (ONSD) as a surrogate measure for intracranial pressure (ICP),5–9 (4) assessing the integrity of the bony orbit and periorbital tissues in severe craniofacial trauma,10 and (5) assessing the pupillary reactivity when visual access to the pupil is impeded.11 However, ocular ultrasound applications are somewhat unique and not standardized at this time, whereas only ONSD measurements have been partially studied in the intensive care unit (ICU) environment. This chapter illustrates specific guidance for ultrasound equipment choice and adjustment, general ocular scanning techniques, and tips to maximize the utility of the ultrasound method for eye and orbit imaging. Equipment controls most frequently used in eye/orbit imaging are gain, TGC (time gain compensation), focus, and power output (see Chapter 1). Additional optimization techniques can be invoked as dictated by specific circumstances. We highly recommend creating a customized eye/orbit preset that could be selected within seconds from the preset menu of the machine. This will save valuable time; ensure standardization; and serve as a safety, training, and quality assurance mechanism. An example is (1) select the factory-made thyroid preset from the preset menu; (2) adjust depth to 4 cm; (3) move the focus marker to 2.5 cm; (4) adjust MI to 0.2312,13 with the power output control; (5) set TGC rheostats at their midrange; (6) scan a patient with indications for ocular ultrasound (e.g., to measure ONSD), and after identifying the terminal optic nerve, adjust gain appropriately; (7) save current settings under a new custom preset name (e.g., “eye-orbit”); (8) scan several patients to “fine-tune” the preset, and resave it with improved settings every time; (9) when satisfied, copy the preset to all machines in the department (if same model), or reproduce its features manually if machines are different. Make sure that additional setting changes do not increase MI; if they do, reduce power output accordingly. Note that perfect presets do not exist, and machine adjustments (at least, gain and TGC) will still be necessary in most patients. Eye and orbit scanning in the ICU is done with closed eyelids. The scope of the examination will depend on patient’s history, status, and open clinical questions. An ICU patient may need only a limited posterior pole and optic nerve examination. However, in trauma patients, the scope of the examination may be broader (see Chapters 1, 51, and 57), and thus a holistic approach (HOLA) ultrasound ocular protocol would include scanning of the eyelids, globe and orbital contents, as well as investigation of the frontal, temporal, zygomatic and nasal bones and overlying tissues. The eye examination proper, in its turn, may be directed at checking the overall integrity of the globe or at a more thorough scrutiny of its entire volume. The AP views (sagittal and axial) are used for ocular anatomy survey and allow viewing practically all ocular structures to rule out macroscopic pathology (Figure 6-1A-C). The oblique sagittal view of the optic disk and terminal optic nerve is used to assess the shape of the optic disk, the terminal optic nerve with its meninges, and as a backup approach to measure ONSD in a sagittal plane (Figure 6-1E). This view may offer a possibility to visualize a longer span of the optic nerve by using a small rotation of the imaging plane. Note that the transducer is placed laterally to the cornea so that the imaging plane bypasses the anterior structures (cornea, anterior chamber, ciliary body, and the lens). The axial view from lateral approach allows avoiding the edge-shadowing artifact that in AP views obscures the peripheral zones of the vitreous humor and the globe wall near the equator (Figure 6-1D). The oblique axial view with optic disk and optic nerve head is the quickest and the most reproducible way to measure ONSD (Figure 6-2). The transducer position is on the upper eyelid (preferably with a downward gaze) with the marker to the right (for both eyes), and the plane bypasses the anterior structures. The resulting target image is similar to the sagittal view (see Figure 6-1E). The coronal view of the iris is used to assess the circular symmetry of the iris and the pupillary reactivity to light (Figure 6-3). Figure 6-1 Standardized primary views in eye ultrasound. A, Anteroposterior (AP) view bisecting the globe sagittally from the corneal vertex to the macula (nerve not in view). Note eyelashes with trapped air affecting most of the inferior (right) part of the image. B, AP axial view with the disk area (arrowhead) and macular area (M). C, Similar to A; however, the imaging plane is shifted medially to pass through the optic nerve head. Although the nerve is visible, this image cannot be used for optic nerve sheath diameter (ONSD) measurement. D, Axial view, lateral approach with a good depiction of the equatorial areas. Note the cup of the optic disk (arrowhead). E, Oblique axial view through the upper lid, bypassing the anterior segment. This is an excellent image for ONSD measurement. F, Same plane as in A, with undue pressure on the probe. Note the flattened cornea. Figure 6-2 Optic nerve sheath diameter (ONSD) measurement technique and examples. A, Determination of the measurement location (3 mm from the vitreoretinal interface). B, Caliper placement for ONSD measurement. C, A posteriorly flattened globe; tortuous and edematous optic nerve and a severely dilated, hypoechoic, and kinked sheath with ONSD greater than 10 mm. D, An image of the optic nerve with a prominent (>7.5 mm) optic nerve sheath. Note the multiple anechoic fluid-filled spaces that have become visible as their size exceeded the resolution limit of the given probe at the given depth. Figure 6-3 The coronal view of the globe in the plane of the iris at baseline (top left) and upon consensual response to contralateral stimulation with light (top right). Below, M-mode cursor is placed over the middle of the iris to record the reflex against time and measure the degree of constriction, the time of response, and its velocity (slope).
Ocular ultrasound in the intensive care unit
(CONSULTANT LEVEL EXAMINATION)
Overview
Equipment and settings
General scanning technique and primary views
Radiology Key
Fastest Radiology Insight Engine