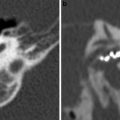
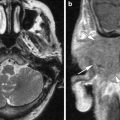
Fig. 1
Normal asymmetry of the jugular foramen. a CT bone window. The right jugular foramen (large arrow) is larger than the left (small arrow, due to the asymmetry of the intracranial venous drainage. b MRI 3d GRE T1 W 1 mm without contrast. The left foramen (large arrow) is larger than the right foramen (small arrow). Notice also the difference in signal intensity of both foramina due to flow-related artefacts
Several anatomical structures goes through the jugular foramen: the sigmoid sinus, jugular bulb, the inferior petrosal sinus, the meningeal branches of the ascending pharyngeal and the occipital arteries, the glossopharyngeal, vagus and accessory nerves, the tympanic branch of the glossopharyngeal nerve (Jacobson’s nerve) and the auricular branch of the vagus nerve (Arnold’s nerve) (Fig. 2a) (Rhoton 2000; Sen et al. 2001).
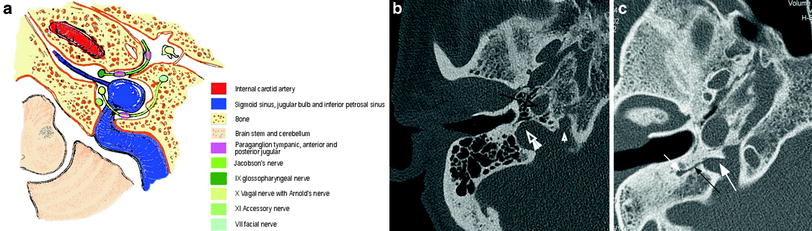
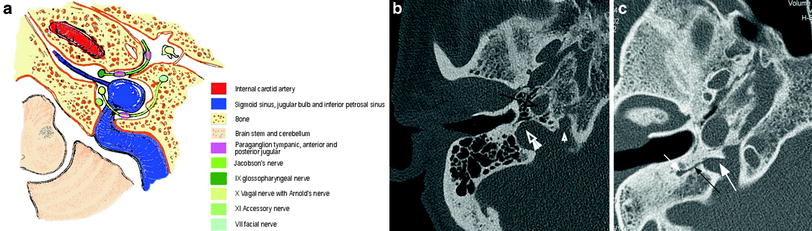
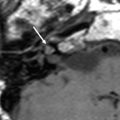
Fig. 2
Normal anatomy of the jugular foramen. a Scheme; b axial CT of the left jugular foramen at the level of the horizontal part of the carotid canal; c axial CT at the level of the vertical part of the carotid canal (black arrow). The jugular foramen is divided into a medial small pars nervosa (small with arrow) and a larger lateral part, the pars vascularis (large white arrow), separated by a bony and fibrous septum. In c the mastoid canaliculus (black arrow), containing the Arnold’s nerve, is visible running from the lateral wall of the jugular foramen (large white arrow) towards the mastoid segment of the facial canal (small white arrow)
Despite several studies, the exact anatomy of the jugular foramen is uncertain, mostly because of the great variations from person to person (Rubinstein et al. 1995). Hovelaque in 1934 described two compartments: the pars nervosa (anteromedial) and the pars venosa (posterolateral). Rhoton (2000) proposes a division in three parts at the intracranial orifice: a small petrosal compartment anteromedially, containing the inferior petrosal sinus, a large lateral sigmoid part containing the sigmoid sinus and an intrajugular part, containing the cranial nerves IX, X and XI. Within the foramen, there is a bony and fibrous septum between the sigmoid and petrosal part. It is through this area that the cranial nerves pass (Fig. 2a, b, c).
The nerve of Jacobson is the tympanic branch of the glossopharyngeal nerve, originating at the external orifice of the jugular foramen. It traverses the tympanic canaliculus to enter the tympanic cavity where it gives rise to the tympanic plexus providing the sensory innervation of the middle ear and the parasympathetic innervation via the otic ganglion to the parotid gland (Fig. 2a).
The nerve of Arnold, the auricular cutaneous branch of the vagus nerve, arises at the level of the superior vagal ganglion. This branch goes to the lateral wall of the jugular foramen to enter the mastoid canaliculus (Fig. 2c), and ascends towards the mastoid segment of the facial canal to exit the temporal bone via the tympanomastoid fissure.
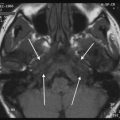
The inferior petrosal sinus enters the jugular bulb between the IXth and Xth cranial nerves, as single or multiple venous channels (Sen et al. 2001) (Fig. 3).
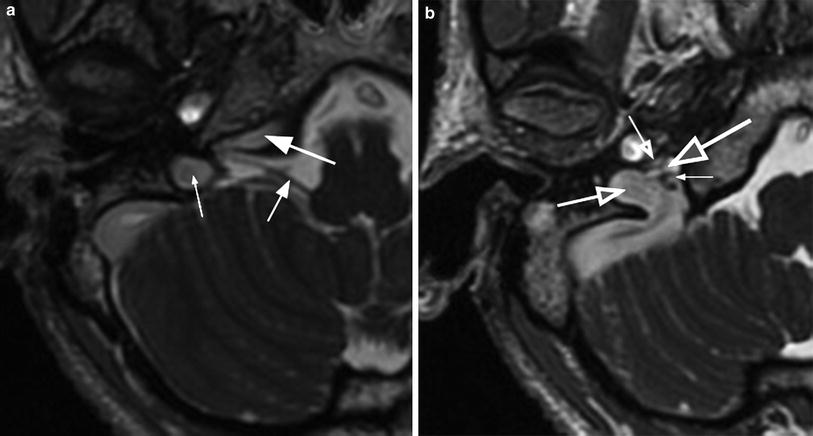
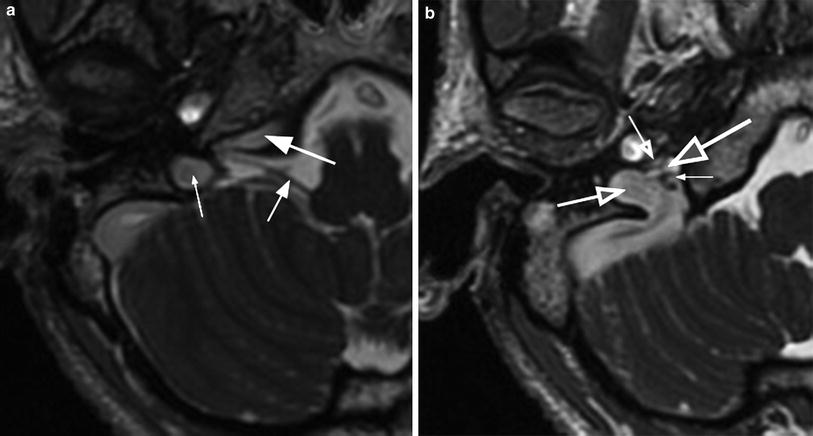
Fig. 3
The inferior petrosal sinus enters the jugular bulb between the IXth and Xth nerves. a high-level trough inferior petrosal sinus; 3D FIESTA with gadolinium. Large white arrow the inferior petrosal sinus. Small white arrow the cisternal segment of the IXth nerve, going to the nervosal part of the foramen. Small white arrow the jugular bulb in the vascular part of the foramen. b entrance of the inferior petrosal sinus in the jugular bulb. 3D FIESTA with gadolinium. The inferior petrosal sinus (largest white arrow) enters the jugular bulb (second largest arrow) between the IXth (second smallest arrow) and Xth nerves (smallest arrow)
The cranial nerves remain fasciculated within the foramen, with the vagus nerve containing multiple fascicles and the glossopharyngeal and accessory nerves containing one and two fascicles, respectively (Sen et al. 2001).
2 Radiological Examination of the Jugular Foramen
The evaluation of the jugular foramen and the temporal bone, especially in tumours requires high-quality cross-sectional imaging with both CT and MR to fully answer all the detailed preoperative questions. For the anatomical variants, CT imaging alone is preferable.
The CT examination is best done with a multidetector spiral CT (when available) making ultra thin sections (0.7 mm) in the axial plane with coronal and sagittal reconstructions. When both CT and MR are used, the task of CT is not to explore the soft tissue extension, but to show the bony anatomy, the condition of the bony margins of the foramen and other structures in the neighbourhood, the extend of the bony destruction of the skull base and to detect some lesion characteristic features that are not visible on MR, like the intratumoral calcifications or the hyperostosis of a meningioma.
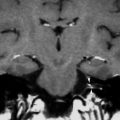
Modern MR techniques allow the identification of the complex anatomy of the jugular foramen and can demonstrate the cranial nerves IX–XII in the foramen. This can be done by using 3D FIESTA (Fast Imaging Employing Steady-State Acquisition) after gadolinium (General Electric). The enhancement of the jugular vein and associated venous plexus surrounding the cranial nerves provided excellent contrast of the small structures within the jugular foramen on FIESTA images after gadolinium, not obtained on 3D FIESTA without gadolinium (Davagnanam and Chavda 2008; Linn et al. 2009) (Fig. 4). Other useful MR techniques are: contrast-enhanced MR angiography, contrast-enhanced 3D T1W, balanced fast-field echo (b-FFE) (Aydin et al. 2011). The contrast-enhanced 3D T1W sequence is somewhat inferior.
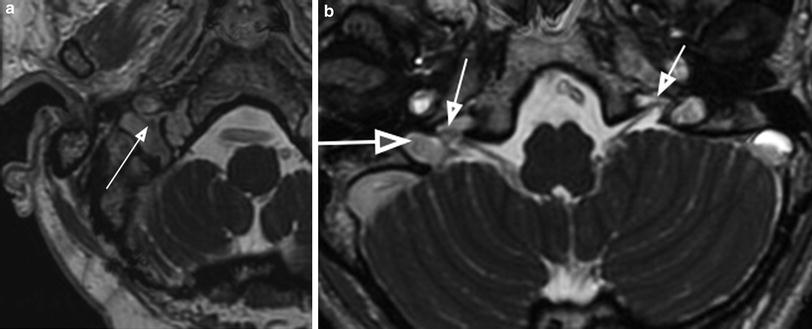
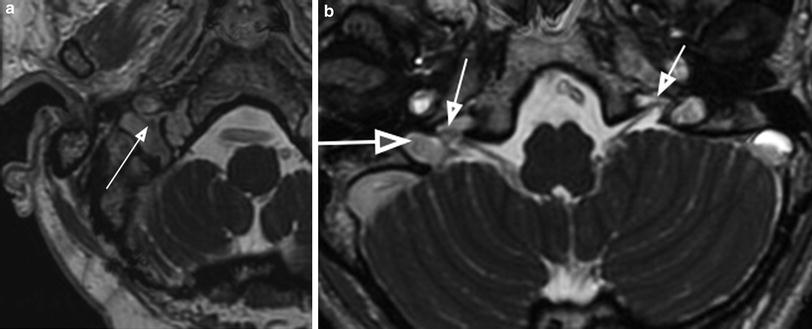
Fig. 4
The cranial nerves in the jugular foramen. a 3D FIESTA with gadolinium. Arrow shows the cranial nerve X in the vascular part of the foramen. b 3D FIESTA with gadolinium. Small arrows show the cranial nerve IX on the right and left side in pars nervosa of the foramen. Large arrow pars vascularis of the foramen
The primary task of MR is to evaluate the soft tissue extension of the disease, to interpret the signal intensity characteristics and to find additional features not visible on CT like the presence of intratumoral vessels in a paraganglioma. Our MR imaging protocol for the jugular foramen (on a GE 1.5 or 3 T) consists of (1) a nonenhanced axial 3D gradient echo T1W sequence with contiguous slice thickness of 1 mm, starting at C2 level until above the internal auditory canal; (2) this sequence is repeated after the administration of gadolinium in the axial plane with coronal reconstructions; (3) a 3D FIESTA after gadolinium with slice thickness of 1 mm; (4) a 2D TSE T2 W sequence in the axial plane 3 mm. starting at the level of C2. In addition, an evaluation of the neck can be necessary in case of a paraganglioma, to find multiplicity. MR venography in the coronal plane can be used to study the patency or invasion of the internal jugular vein, and the sigmoid sinus. In the postoperative situation, after an infratemporal approach with filling up the defect with a fat/muscle graft, the use of a fat-saturated contrast-enhanced T1W image is important to detect recurrent paraganglioma. The diagnosis of recurrent paraganglioma in a previous operated patient can be very difficult.
Angiography is seldom needed for diagnostic purposes, but plays a role in the preoperative embolization (see the chapter on the vascular lesions of the temporal bone).
3 Overview of the Lesions of the Jugular Foramen
The jugular foramen is a complex region of the skull base with an extensive differential diagnostic list of possible lesions.
It is important to recognize the “pseudo-lesions” like the normal asymmetry of the foramen, the anatomical vascular variants (see the chapter on vascular temporal bone lesions) and the modality-dependent pitfalls like the flow-related artefacts on MR (Fig. 1b) (Swartz and Loevner 2009) (Table 1).
Table 1
“Do not touch lesions/pseudo lesions” of the jugular foramen
1. Normal asymmetrically enlarged jugular foramen on CT |
2. Normal asymmetrically enlarged jugular bulb on MRI |
3. Flow-related artefacts of the jugular bulb on MRI |
4. High jugular bulb on CT or MRI |
5. Dehiscent jugular bulb on CT |
6. Jugular bulb diverticulum on CT |
The true lesions can be divided into primary lesions located in the foramen and secondary extensions to the jugular foramen. (Weber and McKenna 1994; Lowenheim et al. 2006; Vogl and Bisdas 2009; Kang Ong and Fook-Hin Chong 2009). The possibilities are different for adults (Table 2), compared to children (Table 3).
Table 2
True lesions of the jugular foramen in adults
Traumatic | Fracture |
CSF lekkage | |
Arterial/venous damage | |
Infectious | Abscess |
Cholesterol granuloma | |
Cholesteatoma | |
Malignant otitis externa | |
Tumoral intrinsic | Paraganglioma |
Schwannoma | |
Meningioma | |
Peripheral primitive neuroectodermal tumour | |
Leptomeningeal metastasis | |
Tumoral extrinsic | Endolymphatic sac tumour |
Chordoma | |
Chondrosarcoma | |
Giant cell tumour | |
Metastasis: bone metastasis | |
Osteosarcoma | |
Temporal bone carcinoma | |
Nasopharyngeal carcinoma |
Table 3
True lesions of the jugular foramen in children
Congenital | Craniosynostosis |
Achondroplasia | |
Meningocoele | |
Congenital vascular variants | |
Infectious | Abscess |
Cholesteatoma | |
Tumour | Meningioma |
Osteosarcoma | |
Ewing’s sarcoma/Peripheral primitive neuroectodermal tumour | |
Rhabdomyosarcoma | |
Vascular | Thrombosis of the jugular bulb |
Dural A-V fistula |
A practical starting point for the differential diagnosis is to look at the dimension and the bony margin of the jugular foramen on CT. There are four possibilities: (1) the jugular foramen is normal; (2) the foramen is enlarged with an intact cortical outline; (3) the foramen is enlarged with an erosion, destruction of its cortical outlines; (4) the foramen has a normal size but its bony margins are destroyed. In the first category, one must think on pseudo lesions like flow-related artefacts on MR, on a dural A-V fistula and on a thrombosis of the jugular bulb or sigmoid sinus. The possibilities in the second category are: normal asymmetry, schwannoma, meningioma, dural A-V fistula, cholesteatoma. The differential diagnostic list in the third category consists of: paraganglioma, metastasis, Ewing sarcoma, giant cell tumour. The lesions of the fourth category are secondary extensions to the foramen from lesion originating elsewhere like: malignant otitis externa, cholesteatoma, metastasis, chondrosarcoma, chordoma, nasopharyngeal carcinoma, endolymphatic sac tumour (Table 4).
Table 4
Differential diagnosis of the jugular foramen lesions, based on the size and the cortical outline of the jugular foramen on CT
A | B | C | D |
|---|---|---|---|
MR flow-related artefacts | Normal asymmetry | Paraganglioma | Malignant otitis externa |
Thrombosis | Schwannoma | Metastasis | Metastasis |
Dural A-V fistula | Meningioma | Ewing sarcoma | Chordoma |
Leptomeningeal metastasis | Dural A-V fistula | Giant cell tumour | Chondrosarcoma |
Nasopharyngeal carcinoma | |||
Endolymphatic sac tumour | |||
Cholesteatoma |
Name | Relationship |
|---|---|
1. Tympanic | The cochlear promontory in the middle ear |
2. Anterior jugular | Jacobson’s nerve (IX) in jugular foramen |
3. Posterior jugular | Arnold’s nerve (X) in jugular foramen |
4. Adventitia of the jugular bulb | Jugular bulb in jugular foramen |
5. (a) Intravagale (b) Extravagale | Ganglion nodosum of the vagal nerve Along the vagal nerve in the carotid space |
6. Facial | Mastoid segment of the facial canal or ganglion geniculi |
7. Carotid body | Carotid bifurcation |
8. Superior laryngeal | Superior laryngeal nerve |
9. Inferior laryngeal | Recurrent laryngeal nerve |
10. Orbital | Ganglion ciliare in the orbit |
11. Fossa pterygopalatina | Pterygopalatine ganglion |
12. Nasopharynx | |
13. Buccal mucosa |
4 Vascular Lesions
These are discussed in the chapter on vascular temporal bone lesions.
5 Common Tumours
5.1 Paraganglioma
Paragangliomas, also called glomus tumours, are neuroendocrine neoplasm’s composed largely of paraganglion chief cells (Burger and Scheithauer 2007). These tumours arise from glomus bodies also named paraganglia. A paraganglion possesses unique regulatory function and is part of the extra adrenal neuroendocrine system. Normal paraganglia occur in the head and neck region at several places (Table 5), frequently located near nerves and vessels (Petrus and Lo 1992; Rao et al. 1999; Lowenheim et al. 2006). Within the jugular foramen, the paraganglioma can arise from paraganglia located in the adventitia of the jugular bulb or at Jacobson’s nerve (nerve IX) or at Arnold’s nerve (nerve X). In the middle ear normal paraganglia are found at the cochlear promontory. Of all paragangliomas, 80 % are either glomus jugulare tumours or carotid body tumours (Lowenheim et al. 2006). Glomus jugular tumours are not encapsulated and tend to infiltrate connective tissue planes (Vogl and Bisdas 2009).
Type | Description |
|---|---|
A | Glomus tympanicum confined to the tympanic cavity of the middle ear |
B | Glomus tympanicum extending into the the mastoid bone but leaving the cortical outline of the jugular foramen intact |
C | Glomus jugulare. The letter C describes the variable extension into the infralabyrinthine portion of the temporal bone and along the carotid canal |
C1 | Minimal erosion of the vertical segment of the carotid canal |
C2 | Extensive erosion of the vertical segment of the carotid canal |
C3 | The erosion extends into the horizontal segment of the carotid canal |
C4 | The tumours reaches the foramen lacerum and may extend into the cavernous sinus |
D | Glomus jugulare with intracranial extension |
De1 to De3 | Extradural extension, depending on the size |
Di1 to Di3 | Additional intradural extension, depending on the size. Di3 means inoperable intracranial extension |
Table 7
Radiological hallmarks of paraganglioma
Modality | Hallmark | Remark |
|---|---|---|
CT | Enlargement of the foramen | Not in type A & C |
Destruction of cortical outline of the foramen | Contrary to schwannoma | |
Isodense without contrast | ||
No hyperostosis | Contrary to meningioma | |
No intratumoral calcification | Contrary to meningioma | |
MRI | Intratumoral vessels | Contrary to schwannoma |
No vascular pedicle | Contrary to paraganglioma | |
Jugular bulb compression, no invasion | Contrary to paraganglioma, meningioma | |
CT and MRI | Necrotic parts possible parts | Contrary to meningioma |
Strong enhancement | ||
Fixed extension pattern |
Paragangliomas restricted to the middle ear are called glomus tympanicum tumours. Glomus jugulotympanicum and glomus jugulare tumours involve, respectively, the middle ear plus the jugular foramen or the jugular foramen alone. Endocrinological functional activity is rare in head and neck paragangliomas, 93 % of the functioning tumours are pheochromocytomas (also a tumour of paraganglionic tissue) and only 7 % occurs at other sites (Maffe et al. 2000).
Paragangliomas may be multiple, either synchronously or metachronously in 3 % for sporadic cases to 26 % for the familial cases (Fig. 5). They can occur in association with pheochromocytoma, thyroid carcinoma, Carney triad (gastric leiomyosarcoma, pulmonary chondroma and paraganglioma) and other endocrine disorders. Familial paragangliomas have a prevalence of 7–9 %, with 90 % of the cases arising from the carotid body (Rao et al. 1999).


Fig. 5
Multiple paragangliomas. a CT-angiography, sagittal MIP reconstruction of axial contrast-enhanced thin sections from a multislice spiral CT examination. A large carotid paraganglioma (large arrow) is situated at the bifurcation of the common carotid artery, displacing the internal carotid artery backwards and the external carotid artery anteriorly. In the higher cervical region, a small vagal paraganglioma (midsize arrow) is typically situated behind the internal carotid artery, witch is displaced anteriorly. At the skull base, a jugular paraganglioma (small arrow) is visible with its extension in the carotid loge below the skull base. b and c MRI axial T1W after gadolinium shows bilateral vagal and jugulotympanical paraganglioma
The symptoms depend on the primary site of origin and the extension of the tumour and include: a vascular tympanic membrane, conductive hearing loss, pulsatile tinnitus, bruit, vertigo, sensorineural hearing loss, cranial nerve deficit.
Paragangliomas are benign, but local invasive and very vascular tumours. From its origin in the middle ear, the glomus tympanicum first invades the bone between the hypotympanum and the jugular foramen. With further growth they are indistinguishable from a glomus jugulare, hence the term glomus jugulotympanicum. The differentiation between a simple glomus tympanicum and a glomus jugulotympanicum is an important radiological task, because there is a big difference in the operative approach, with the latter requiring extensive skull base surgery. From the jugular foramen the tumour can extend laterally with destruction of the mastoid segment of the facial canal and invasion of the facial nerve. Anteriorly, the tumour grows into the total middle ear and further along the petrous bone to the foramen lacerum and the cavernous sinus. Inferior spread produces infiltration of the internal jugular vein and further growth in the carotid loge below the skull base. The intracranial extension is first situated extra-axial in the cerebellopontine angle and in advanced cases not only extra-axial, but also intra-axial in the cerebellum. Glomus vagale tumours, arising from the ganglion nodosum or extravagal, may secondary extend into the jugular foramen.
The neuroradiological evaluation requires both CT and MRI (Table 7). Thin section CT in the axial and coronal plane with bone window gives information about the surrounding bony structures, such as the enlargement and erosion of the jugular foramen, the infiltration of the petrous bone, the carotid canal, the facial canal, the hypoglossal canal and the inner ear structures. It also helps in the differential diagnosis with lesions that do not erode the bone like schwannoma, meningioma (Fig. 6). MR shows the soft tissue extension of the tumour in the ear and below the skull base and intracranially (Fig. 7). MR is equally important in the differential diagnosis by showing the characteristic intratumoral vessels (signal void) and the frequent presence of subacute intratumoral haemorrhage with a high signal in the T1W and T2W image. The combination of both features gives a salt and pepper appearance in the T1W images without contrast. This feature is limited to the larger paragangliomas (>1 cm) and is not pathognomonic, as it is also seen in other hypervascular lesions like metastasis. Use of contrast is necessary to find the smaller tumours like the glomus tympanicum and for the demonstration of the soft tissue extent in the larger tumours. All paragangliomas have a strong enhancement. MR venography provides information about the jugular vein occlusion and collateral venous drainage. Two hallmarks of this tumour are the bony erosion and the rich vascularisation (Fig. 6). The latter poses special problems of blood loss during operation. Preoperative embolisation is needed in the larger tumours (see the chapter on the vascular lesion of the temporal bone).
Table 8




Classification of jugular foramen schwannoma (Samii et al. 1995)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree