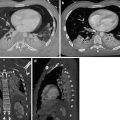
Fig. 1
(a) CXR: pneumothorax is located only in the anteromedial and subpulmonary site. The radiant beam does not tangentially detect any visceral pleural border, and the sign of the “visceral line” is not appreciable; (b) axial CT image shows very clearly the PNX located in the bilateral anterior-basal site
The lung presents compliance alterations (contusion, edema) that may prevent a harmonic collapse toward the ilium; the presence of lung pattern external to the supposed “pleural line” does not rule out the diagnosis of PNX.
The radiological signs to detect a PNX in clinostasis are:
Hyperlucency of the lower part of the chest and the upper quadrants of the abdomen (Fig. 2)
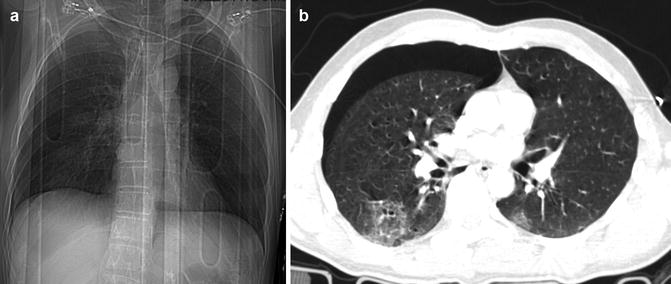
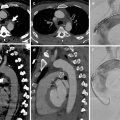
Fig. 2
(a) CXR image shows the hyperlucency of the right basis; (b) axial CT scan confirms the PNX placed in the anterior-basal site
Deep sign of the lateral pleural sinus (the deep sulcus sign) (Fig. 3)
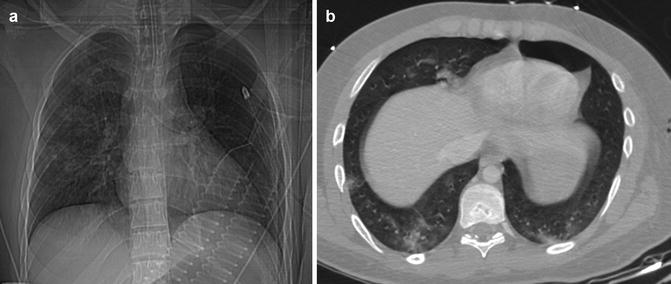
Fig. 3
(a) CXR image: mild deepening of the lateral pleural sinus that allows to suspect the presence of PNX in the lower left part of the chest (deep sulcus sign). (b) Axial CT image clearly shows the PNX located in anterobasal left site
Double-diaphragm appearance
Sharp appearance of the diaphragmatic outline (Fig. 4)
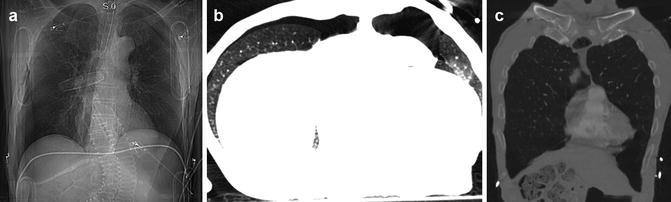
Fig. 4
(a) CXR image: bilaterally appreciable is the sharp appearance of the diaphragmatic outline; also evident is a clear demarcation of the profile of the aortic arch and the cardiac silhouette. (b) Axial CT scan and (c) coronal reconstruction demonstrate the presence of PNX localized in the bilateral anteromedial site
Sharpness of the cardiophrenic fat pad
Sharpness of the inferior surface of the lung
High visibility of the pleural surface of the lung (more frequent in apical position)
Air can, also, separate the edges of the heart, aorta, and vena cava that take an unusual sharp appearance. The air, collected in the posteromedial pleural recess, can be recognized as radiotransparent paraspinal line, alongside the descending aorta and in the posterior costophrenic sulcus. It is essential to carefully inspect the lower lobes of the lung and the upper abdomen to avoid missing such signs. In general, if small flaps of PNX, unrecognized on AP view, have no clinical relevance, they may rapidly expand in intubated patients on positive-pressure ventilation, putting the patient’s life at risk. In such a scenario, the radiographic evidence of rib fractures and homolateral subcutaneous emphysema are considered a sign of PNX even in the absence of sharp intrapleural gas folds.
3 Tension PNX
Tension PNX is an emergency clinical condition that requires an immediate treatment, being associated with a reduction of cardiac filling and compression of the homolateral lung. About one-third of the patients with unrecognized PNX progress into a tension PNX.
If the diagnostic evidence of a simple PNX must be communicated to the trauma leader in real time (and written in the report), the same is even true for the diagnosis of tension PNX (Mirvis et al. 2004, 2005).
3.1 Diagnostic Imaging
The radiological diagnosis of PNX can be guided through the following signs:
Contralateral dislocation of the mediastinum (Figs. 5 and 6)
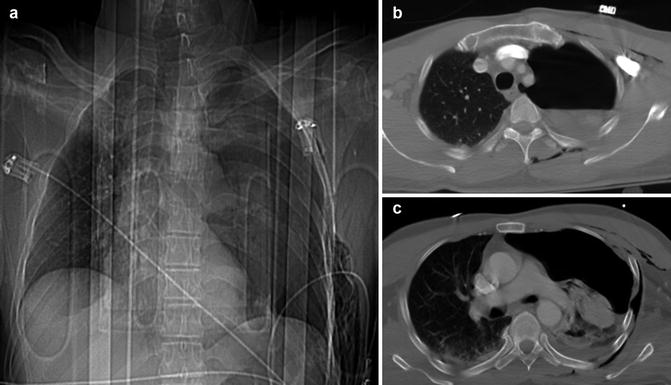
Fig. 5
(a) CXR and (b, c) axial CT images show the presence of large hydro-PNX on the left site caused by multiple rib fractures, resulting contralateral dislocation of the mediastinum. In CXR image, it is also visible the extension of the intercostal spaces

Fig. 6
(a) Axial and (b) coronal CT images demonstrate the presence of large PNX on the right site that causes contralateral displacement of the mediastinum. It is also visible the presence of a pulmonary contusion in the postero-basal right site
Flattening/inversion of the diaphragm (Fig. 7)

Fig. 7
CXR: Tension PNX, double-diaphragm sign. Contralateral dislocation of the mediastinum; flattening and inversion of the diaphragm and extension of the intercostal spaces
Extension of the intercostal spaces (Fig. 7)
Flattening of the cardiac profile (Fig. 8)

Fig. 8
CXR: Tension PNX. The image shows the flattening of the cardiac profile; this sign is related to the cardiovascular and respiratory distress
The mediastinal shift is not a specific sign of tension PNX because it may be visible, to some extent, also in simple PNX; on the other hand, the flattening of the cardiac profile may be the sign better related to the cardiovascular and respiratory distress that markedly characterizes the tension PNX. If tension PNX is persistent despite the correct functioning of the drainage, it is essential to rule out any injury of the main airways.
4 Hemothorax
In polytraumatized patients with blunt chest trauma, pleural effusion is present in approximately 30–50 % of cases, and it is usually hematic in nature (hemothorax) (Brooks et al. 2004).
However, in the acute stage, it is also possible to detect simple serous effusions (due to a reduction of the respiratory mechanics and pleural reabsorption) often associated with atelectasis or homolateral chest wall injuries that reduce the respiratory excursion. On the other hand, it is quite occasional the detection of chylous effusion, due to the rupture of either the thoracic lymphatic ducts (thoracic duct) or of the bile duct, as a result of biliopleural fistula formation that is more common in penetrating trauma.
Bleeding in the pleural cavity often occurs some hours after the trauma; it is sometimes bilateral, and it is often associated with a PNX. The causes responsible for a hemothorax include lacerations of the intercostal vessels, pulmonary contusions, pleural and pulmonary lacerations, and injuries to the diaphragm; iatrogenic lesions, for example, those following a central venous catheter, are also possible causes.
The management of hemothorax depends on its initial quantity, on the amount of blood flow, and on the health condition of the patient.
The initial, usually decisive treatment is the placement of a tube thoracostomy. Patients, who, as soon as the drainage is inserted, evacuate more than 1500 cc, need a surgical or endovascular control of the bleeding.
A hemothorax associated with contusion is usually self-limiting, whereas it may be massive and protracted, when it is associated with pulmonary lacerations or mediastinal lesions.
Venous hemorrhages are self-limited and without mass effect, whereas arterial hemorrhages are under pressure, and they may trigger a significant compression of the pulmonary parenchyma, mediastinum, and heart.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree