Age (years)
Chinese a, f (%)
Japanese b, g (%)
Latin American c, g (%)
European d, g (%)
American (white) e, g (%)
50 ~ 59
2.7
6.9
6.3
60 ~ 69
10.8
13.8
10.2
11.7
14.5
70 ~ 79
17.4
17.5
18
20.9
22
80+
29.5
27.8
33.9
It has been shown that the relative risk of new vertebral fracture increases with the number of baseline vertebral fractures (Black et al. 1999; Siris et al. 2007). Therefore, determining vertebral fracture status in addition to BMD, provides practical information when predicting fracture risk in post menopausal women (Siris et al. 2007). Over an 8-year period, subjects with pre-existing vertebral fractures had a 5-fold increased risk of further vertebral fractures and a 3-fold increased risk of proximal femoral fracture compared to those without a pre-existing vertebral fracture (Black et al. 1999). Incident vertebral fractures also increase risk of future vertebral fractures especially in the year following the fracture; 20 % of women with incidental vertebral fracture experience another fracture within a year (Lindsay et al. 2001). This demonstrates the need for identification and intervention of at-risk patients, especially as early treatment with appropriate anti-fracture medication significantly reduces the occurrence of new vertebral and nonvertebral fractures (Ensrud and Schousboe 2011).
Despite the importance of early vertebral fracture, under diagnosis is an appreciable problem worldwide. There are many reasons. First, vertebral fractures are often asymptomatic with only one-third of retrospectively diagnosed vertebral fractures relating to a clinically symptomatic period (Cooper et al. 1992). Second, the typical clinical symptoms of back pain and restricted movement are usually attributed to spondylosis rather than vertebral fracture so that most patients with vertebral fracture do not seek medical attention. Third, about one-third to one-half of vertebral fractures are under diagnosed in radiology reports (Delmas et al. 2005). Many vertebral fractures are clinically asymptomatic, and radiologists and clinicians who review imaging studies should look specifically for vertebral fractures (Lenchik et al. 2004; Adams et al. 2010). If a vertebral fracture is present, then it is imperative that it is reported clearly as a “vertebral fracture” and not with ambiguous descriptions such as “vertebral collapse”, “compressed vertebral body”, “loss of vertebral height”, “wedging of vertebral body”, “wedge deformity”, “biconcavity” or “codfish deformity”. The location and severity of any vertebral fracture should also be clearly stated.
2 Pathophysiology of Vertebral Fracture
Unlike the diaphyses of long bones, the vertebral body mainly relies on trabecular bone for its strength rather than cortical bone. However, trabecular bone surface area and thinness makes it particularly responsive to change in its microenvironment and, therefore, vertebral bodies are one of the first bones to be affected in osteoporosis (Griffith et al. in press). The vertebral body is particularly prone to early osteoporotic fracture. The weakest parts of the vertebral body are the central and antero-superior components of the endplates where lower BMD is not compensated by higher trabecular strength (Banse et al. 2002). Other features such as microarchitecture, collagen composition, microdamage, mineralization, and osteocyte function may also play a role, although their relative contributions to vertebral strength remain ill-defined (Christiansen and Bouxsein 2010). Beside BMD, vertebral strength largely depends on vertebral size. An increase in vertebral body cross-sectional area will increase vertebral body strength (Griffith et al. in press). With age, vertebrae undergo periosteal apposition with resultant outward cortical displacement as a response to diminishing BMD. This enlarges the cross-sectional surface of the vertebral body and increases its resistance to compressive forces. These changes in vertebral body cross-sectional area can help somewhat to offset other changes occurring with age which have a cumulative deleterious effect, such as increased endocortical resorption, increased cortical porosity, and especially, decreased trabecular vertebral BMD (Riggs 2004). A greater lifelong decrease in trabecular and cortical vertebral bone mass coupled with a smaller bone size in women at the end of puberty compared to men helps to explain why osteoporotic fractures are more common in elderly women than in elderly men (Riggs 2004).
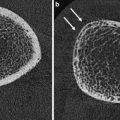
Changes in trabecular bone with age have been studied including assessment of the number and thickness of both vertical and horizontal trabeculae. While both horizontal and vertical trabeculae are removed with age, corresponding to a decrease in trabeculae number, only horizontal trabeculae display significant loss of thickness (Thomsen et al. 2002). The horizontal trabeculae are thought to be lost largely because of strain-adaptive resorption, while vertical trabeculae loss is due to perforation from microdamage resorption followed by rapid strain-adaptive resorption of the remaining unloaded trabeculae (Mc Donnell et al. 2009). The predominant loss of horizontal trabeculae and the preservation of the longitudinal trabeculae can result in the radiographic appearance of longitudinal striation (Fig. 1).


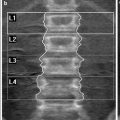
Fig. 1
Radiograph of osteoporotic lumbar vertebrae. The vertical striations of the spongiosa result from the loss of the horizontal trabeculae and preservation of remaining vertical trabeculae
A vertebral fracture occurs when the force sustained by the vertebra exceeds its strength. Unlike long bones where fractures occur as a definite event, vertebral fractures often progress incrementally and this incremental nature is reflected in the overlapping of the various stages of fracture healing seen on histology (Diamond et al. 2007). Depending on the sustained force and inherent vertebral body strength, fracture severity can vary from a minor peripheral fracture to an almost complete vertebral body fracture. Most vertebral fractures occur in the mid-thoracic (T6-T8) and thoracolumbar (T11-L2) regions (Genant et al. 1996). Compressive loading is accentuated in the mid-thoracic spine during flexion when increased kyphosis is present, and also in the thoracolumbar region which is the transition zone between the relatively fixed thoracic, and the more mobile lumbar segments. Osteoporotic vertebral fractures are rare above the T4 level (Genant and Jergas 2003). Loading on the spine is determined by gravitational forces and muscle contracture which, in turn, are influenced by body weight, height, muscle action, coordination, and strength as well as spinal curvature and intervertebral disk characteristics (Christiansen and Bouxsein 2010). Fracture of a single vertebral body, particularly of the anterior wedge type, shifts compressive forces toward the anterior aspects of the vertebral bodies, potentially leading to a vertebral fracture “cascade”, characterized by fractures in adjacent vertebrae occurring in rapid succession (Christiansen and Bouxsein 2010).
3 Clinical Diagnosis of Vertebral Fracture
Vertebral fractures are difficult to identify clinically. Recent large cohort studies of postmenopausal women with low BMD have shown that only about one-fourth of incident radiographic vertebral deformities were clinically diagnosed as new vertebral fractures (Fink et al. 2005). Clinical recognition is better for more severe fractures (30 %) than mild fractures (15 %) (Fink et al. 2005). This low recognition rate can be attributed to the absence of specific symptoms and difficulty in determining the cause of symptoms such as pain or height loss. Less than 1 % of back pain episodes are related to vertebral fracture (Ettinger et al. 1995). Historical height loss is difficult to assess clinically. While some spinal height loss is expected with aging due to degenerative and attritional remodeling of the vertebral bodies, narrowing of intervertebral disks, and postural and scoliotic changes, loss of height can also be the result of vertebral fracture. Height loss is considered an unreliable indicator of fracture status until it exceeds 4 cm (Ettinger et al. 1992). Overall, clinical evaluation of vertebral fracture has poor sensitivity and specificity.
4 Radiographic Diagnosis of Vertebral Fracture
Although radiography of the thoracolumbar spine is the standard imaging approach for assessment of vertebral fracture, there is no agreed upon gold standard to define osteoporotic vertebral fracture. To resolve this issue, the first step is to define clearly what a “normal” vertebral body is, taking into account the wide range of intra- and inter-individual variation in vertebral body size and shape. Technical considerations, such as the oblique projection secondary to malpositioning of the patient, and the parallax effect caused by the divergent X-ray beam are additional factors that can create a misleading appearance (Hurxthal 1968). Once a vertebral body is recognized as “abnormal”, the second step is to decide whether this abnormality actually indicates an osteoporotic fracture (Smith-Bindman et al. 1991; Cooper and Melton 1992; Herss Nielsen et al. 1991). Established methods rely mainly on the reduction of vertebral height to define a vertebral fracture. This is problematic especially for mild pre-existing (prevalent) fracture, since only a longitudinal comparison can identify true change in vertebral height (Ferrar et al. 2005).
Not every deformed vertebral body is a result of osteoporotic fracture. Radiologists should be aware of six common pitfalls that can be confused with mild vertebral fractures:
Physiologic wedging is a normal feature as the spine changes from thoracic kyphosis to lumbar lordosis. All vertebrae, but particularly T5-T9, T12-L1, L4-L5 are physiologically wedged. The vertebral bodies of the lower thoracic and upper lumbar spine (T10-L2) are slightly anteriorly wedged, while the lower lumbar region is posteriorly wedged (L4 & L5) (Fig. 2) (Masharawi et al. 2008).
Fig. 2
Lateral X-rays of the lumbar spine in a 30-year-old woman and 25-year-old man, respectively. a Normal appearance of physiologic posterior wedging of L5. b Physiologic anterior wedging of L1 and L2
Short vertebral height (SVH) is an important physiological feature that occurs with age and is commonly over-diagnosed as osteoporotic fracture. Differentiating SVH from a mild vertebral fracture is probably the most contentious and difficult area in vertebral fracture diagnosis. SVH is independent of osteoporosis and vertebral fracture, and is more important on the anterior aspect of the vertebrae than the middle and posterior parts, particularly with regard to thoracic kyphosis in the elderly (Diacinti et al. 1995). Women between 30 and 70 years of age show a decrease of the combined height of the anterior aspects of the vertebral bodies from T4 to L5 at a rate of about 1.5 mm/year, while the combined middle and posterior heights decline at about 1.2 mm/year (Diacinti et al. 1995). SVH refers to a reduction in vertebral height of up to 20 % of the expected height, but it is sometimes very hard to differentiate from a mild vertebral fracture (20–25 % of height loss). However, the majority of evidence suggests that isolated SVH is not associated with low BMD or irregularity of the vertebral endplate (Ferrar et al. 2007). SVH, when isolated and when not associated with endplate irregularity or other features of fracture, is most likely the result of physiological wedging exacerbated by vertebral remodeling due to increasing age or spondylosis as discussed in the previous section (Fig. 3) (Griffith et al. in press).
Fig. 3
SVH of L1 and L2 exaggerated by degenerative remodeling. Notice the presence of associated anterior osteophytes and L1-L2 disc space narrowing
Scheuermann disease is a disorder that causes back pain in teenagers and young adults, and is likely related to compressive injuries to the cartilaginous endplates. It is identified by these criteria: (i) elongated vertebral bodies affecting at least three adjacent vertebrae; (ii) irregular wavy endplates with Schmorl nodes; (iii) accelerated degenerative changes (Ferrar et al. 2007). It can affect the thoracic or lumbar spine, mostly the former, leading to an exaggerated thoracic kyphosis and a decreased lumbar lordosis or both. An increased anteroposterior diameter of the vertebral body, small intervertebral disk, endplate irregularity, and premature disk degeneration are helpful features for diagnosing Scheuermann disease and distinguishing it from vertebral fracture.
Obliquity of vertebral bodies due to scoliosis may lead to side-to-side discrepancy in vertebral body height. On the lateral projection, this obliquity gives a biconcave outline to the vertebral endplates which may be misinterpreted as a vertebral fracture. On the anteroposterior view, the vertebral body is reduced on the concave side, and of normal height, or even increased, on the convex side. Degenerative-type scoliosis is quite common, particularly in the elderly lumbar spine. With experience, one can determine whether the degree of apparent loss of vertebral height is commensurate with the degree of scoliosis. Unilateral loss of vertebral height due to scoliosis should not be considered a vertebral fracture.
Schmorl node is a displacement of intervertebral disk tissue into the vertebral body. Although Schmorl node is a manifestation of Scheuermann disease, it is far more commonly encountered in isolation (Pfirrmann and Resnick 2001), present in 40–75 % of imaging studies and sometimes associated with degenerative disease of the lumbar spine (Griffith et al. in press). Schmorl node only involves a segment of the endplate, and is seen as well-defined rounded contour, with an intact sclerotic margin (Fig. 4).
Fig. 4
Lateral X-ray of the lumbar spine showing Schmorl nodes of the inferior endplates of T11, T12, and L1. Notice their characteristic rounded contour with sclerotic margin (arrows)
Cupid’s bow deformity is a common developmental endplate contour abnormality, most frequently affecting the inferior endplate of the fourth and fifth lumbar vertebral bodies. The more cephalad lumbar vertebrae, as well as thoracic vertebrae, may rarely be involved (Chan et al. 1997). It results from a lack of cartilage in the parasagittal endplate areas leading to impaired endochondral growth of the vertebral body with concave endplate depressions, resembling Cupid’s bow on the anteroposterior radiograph. The nucleus pulposis tends to be enlarged and bilobed. On the lateral projection, the posterior two-thirds of the inferior endplate are indented, simulating a depressed endplate fracture (Griffith et al. in press) (Fig. 5).
Fig. 5
AP X-ray of the lumbar spine in a 25-year-old woman displaying normal appearance of Cupid’s bow of the inferior endplate of L5 (arrows)
In conclusion, “while all vertebral fractures result in vertebral deformity, not all vertebral deformities represent a vertebral fracture” (Genant and Jergas 2003). Radiologists should be aware of entities other than fracture that can change vertebral body shape. The term deformity is appropriate when reporting such nonfracture etiologies (Link et al. 2005). With careful scrutiny of imaging features, these vertebral deformities can usually be differentiated from vertebral fractures.
5 Spinal Radiography
In clinical practice, radiographic diagnosis is the best way to identify osteoporotic vertebral fracture. The standardized radiographic protocol consists of anteroposterior (AP) and lateral views, including the C7-S1 vertebrae. A focus-film distance of 100 cm and an X-ray beam centered at T7 and L3, for the thoracic and lumbar spines respectively, are necessary for a good radiographic spinal examination. Because of the superimposition of the scapula and shoulder regions, the upper thoracic (T1-T3) vertebral bodies are often not clearly seen on lateral views. However, isolated osteoporotic fractures in this region are extremely uncommon. On the lateral projection, the spine must be parallel to the film so that the vertebral endplates at the level of the central X-ray beam are superimposed and seen as single dense, well-defined cortical lines. Since the X-ray beam is divergent, the endplates distant from the centering point appear concave (“bean can”’ effect) and must not be mistaken for vertebral fractures. Although a lateral view is usually sufficient, an AP projection may help detect scoliosis and determine the anatomical level of a vertebral fracture. For the thoracic spine, both an AP and a lateral projection are often undertaken, since the lateral view in isolation may not display the vertebral body outline as consistently as in the lumbar region. The typical effective doses of ionizing radiation from a single lateral and AP projection of the thoracic spine are 0.3–0.4, while for the lumbar spine they are 0.3–0.7 mSv. By comparison, a 16-hour return transatlantic flight would amount to 0.07 mSv background radiation (Griffith et al. in press; Damilakis et al. 2010).
One global prospective study (the IMPACT study (Delmas et al. 2005)), compared the results of local radiographic reports from five continents with that of subsequent central readings in more than 2,000 postmenopausal women with osteoporosis. This study pointed out the significance of radiological under-diagnosis of vertebral fractures worldwide, with false-negative rates ranging from 27 to 45 %, despite a strict radiographic protocol that provided an unambiguous vertebral fracture definition and minimized the influence of inadequate film quality. It was concluded that the failure was a global problem attributable to either or both lack of radiographic detection and use of ambiguous terminology in reports.
Radiographic examinations of the thoracolumbar spine are usually evaluated by radiologists or clinicians with experience in viewing radiographs to identify vertebral fractures. This said, there is still no universally agreed definition of vertebral fracture. The importance of radiographic evaluation in the identification of vertebral fractures, and the susceptibility of radiographic output to bias, has prompted the quest for a standardized and objective visual assessment method of vertebral fracture identification. Different approaches have been proposed to facilitate both the detection and progression of osteoporotic fracture. These methods are presented in the next section.
6 Visual Assessment of Vertebral Fracture
Since the introduction of the first standardized approach by Smith et al. (1960), which graded only the most severely deformed vertebrae on lateral radiographs, further work has attempted to bring more precision and sensitivity to reporting vertebral fractures. Meunier proposed a grading method according to the shape and deformity of the vertebrae (Meunier 1968) (normal, biconcave, endplate fracture, wedged, or crushed vertebra). A “radiological vertebral index” was calculated as the sum of the vertebral grades, or as a quotient of this sum and the number of vertebrae. Kleerekoper and Nelson (1992) modified Meunier’s radiological vertebral index and introduced the so-called “vertebral deformity score” in which a score was assigned to each vertebrae from T4 to L5 based on the reduction in the anterior, middle, and posterior heights (ha, hm, and hp respectively). A vertebral deformity was defined as a reduction of ha, hm, or hp by at least 4 mm or 15 %. These methods depend on vertebral shape and an incident vertebral fracture could only be detected if vertebral shape changed significantly. Genant et al. proposed a standardized visual approach to vertebral fracture identification and grading known as the semiquantitative (SQ) method (Fig. 6) (Genant et al. 1993, 1996; Genant and Jergas 2003). This method is based on the quantification of vertebral height reduction, as well as qualitative assessment which considers the integrity of the endplate, cortical borders, and other deformities such as biconcave, wedge, and compression. The SQ method is easy to apply and is more objective and reproducible than purely qualitative methods, resulting in better interobserver agreement. These clear advantages have made it a standard in several important epidemiological studies of osteoporosis (Ferrar et al. 2005; Siris et al. 2002; Harris et al. 1999) and in most clinical trials of osteoporosis therapies (Meunier et al. 2009; Matsumoto et al. 2009; Chesnut et al. 2004).
Fig. 6
Genant’s grading scheme for a semiquantitative evaluation of vertebral fracture. The drawings illustrate normal vertebrae (top row) and mild to severe fractures (respectively in the following rows). The size of the reduction in the anterior, middle, or posterior height is reflected in a corresponding fracture grade, from 1 (mild) to 3 (severe) (from Genant et al. 1993)
Genant’s SQ approach consists of visually grading each vertebra from T4 to L4, without direct measurements, based on the apparent degree of vertebral height loss. Relative to either normal appearing adjacent vertebrae or relative to what one would normally expect vertebral height to be at that level, the vertebrae are graded as normal (grade 0), mildly deformed (grade 1, reduction of ~20–25 % of height (Fig. 7), moderately deformed (grade 2, reduction of ~25–40 % of height), and severely deformed (grade 3, reduction ~ >40 % of height). Grade 0.5 is sometimes used and designates a borderline vertebral fracture that shows deformity but cannot clearly be assigned to grade 1. In addition, when using the SQ method, it is requisite that one also considers changes of the vertebral endplate and cortical margin, and lack of consistency with adjacent vertebrae, all of which help to distinguish fracture from SVH (Genant et al. 1993).
Fig. 7
Lateral X-ray of the lumbar spine showing a mild anterior fracture of L1 (grade 1 according to Genant’s SQ assessment) in a 53-year-old man presenting with 1 week history of back pain
The SQ analysis of spinal radiographs for vertebral fracture is faster than other methods of vertebral fracture assessment, easy to implement, and suited to epidemiological research studies, clinical therapeutic efficacy trials, and everyday clinical practice. Vertebral fractures detected by SQ analysis are associated with low BMD and are predictive of future fracture, regardless of BMD (Siris et al. 2002, 2007; Delmas et al. 2005; Griffith et al. in press). For longitudinal studies, serial radiographs should be viewed in chronological order to fully appreciate changes in vertebral morphology. Although visual assessment methods of vertebral fractures are potentially more subjective than morphometric analysis, they do allow the experienced reader to address critical issues such as nonosteoporotic deformity and projectional artifacts. SQ analysis is also better suited to deal with errors introduced by radiographic technique such as magnification effects, which clearly would influence serial vertebral body measurements. The SQ method is a practical and reproducible method of vertebral fracture assessment when performed by trained and experienced readers (Griffith in press; Ferrar et al. 2012; Buehring et al. 2010).
6.1 Vertebral Quantitative Morphometry
Vertebral quantitative morphometry (QM) is only used in a research setting (Guglielmi et al. 2008). The two main advantages of QM over other methods are that it can be performed by relatively inexperienced or nonmedical research staff, and it provides an objective measure of loss of vertebral height on serial images (Griffith in press). While the description and definition of the methodology is straightforward, the application in practice is often rather subjective. Vertebral QM consists of placement of six points delineating each vertebral body from T4 to L4. The four corner points and two additional points in the middle of the upper and lower endplates are used (Fig. 8). This technique was introduced in 1960 by Barnett and Nordin, who used a transparent ruler to measure vertebral heights on lateral radiographs of the thoracolumbar spine. Vertebral morphometry is performed on lateral radiographs (morphometric X-ray radiography or MRX) though it can also be applied to images obtained from dual X-ray absorptiometry (DXA) (morphometric X-ray absorptiometry or MXA). Currently, QM uses digital images displayed on a high-resolution workstation. Digitization allows magnification of images to a specific level, optimization of contrast and brightness levels, and digital archiving. Point placement may be done manually or automatically. Manual placement, proposed by Hurxthal (1968), excludes features such as Schmorl nodes and osteophytes from measurements. When the outer contours of the endplate are not superimposed (due to incorrect positioning or severe scoliosis), the middle point is placed centrally between the upper and the lower endplate contour (Guglielmi et al. 2008). With automatic placement, which brings more precision by reducing operator dependent errors (Nicholson et al. 1993; Kalidis et al. 1992), the endplates and the four corners of the vertebral bodies are highlighted by image post-processing. The software determines the midpoints between the posterior and anterior corner points of the upper and lower endplates, and then the reader selects the true midpoints by moving the caliper along the vertical midline joining the endplates (Guglielmi et al. 2008). Afterward, the computer calculates the posterior, anterior, and middle heights (ha, hm, and hp) of each vertebra from T4 to L5, as well as specific indices reflecting vertebral shape. These indices consist of AH/PH (anterior wedging), MH/PH (endplate concavity), and PH/PH’ of the adjacent normal vertebrae (posterior compression) (Griffith et al. in press; Grados et al. 2009). Prevalent vertebral fracture is defined as a reduction in one or more of the three vertebral height ratios (AH/PH, MH/PH, or PH/PH’) >20 % or 3 standard deviations from the mean of a reference population. Incident vertebral fracture is defined as a reduction in one of the three height ratios (AH/PH, MH/PH, or PH/PH’) >15–20 % or 3–4 mm compared to baseline (Griffith et al. in press; Melton et al. 1993; Eastell et al. 1991). While the reproducibility of QM is good in normal subjects, with an interobserver coefficient of variation of <2 %, it is not as good in the very elderly and in those with osteoporotic fractures where the interobserver and intraobserver coefficients of variation are 5 and 6.3 % for MH (Grados et al. 2001). Although QM parameters are objective, the approach has some significant limitations.