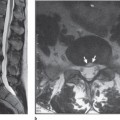
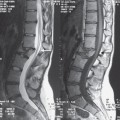
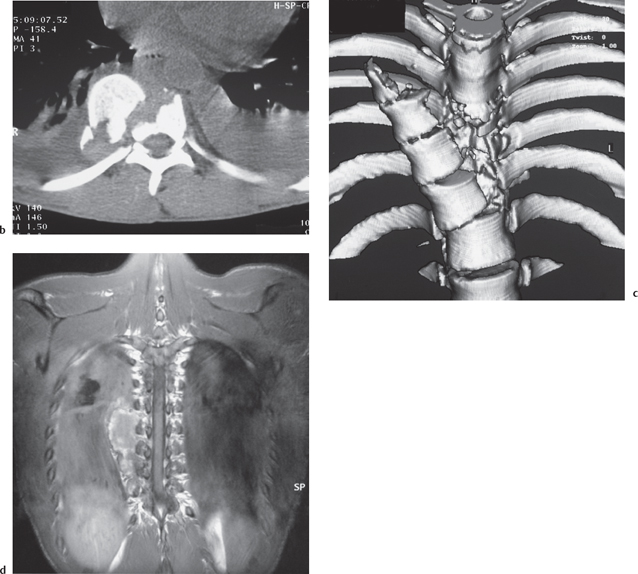
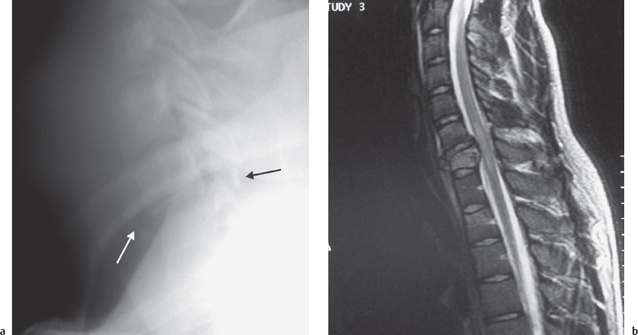
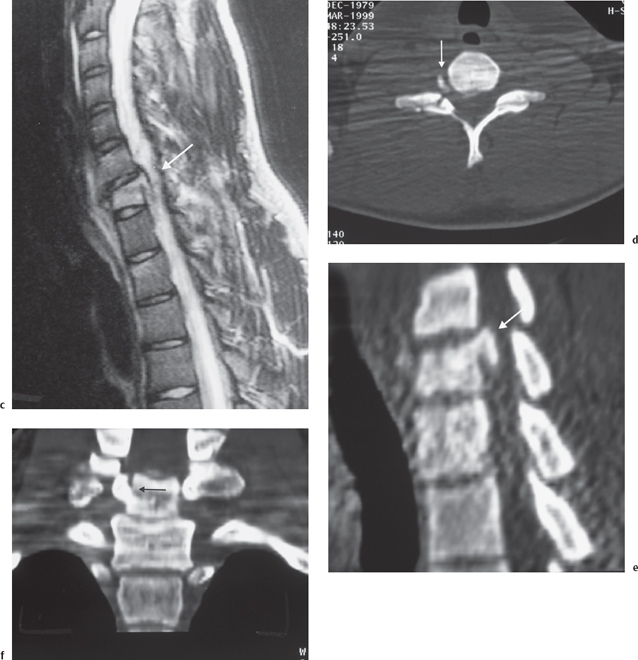
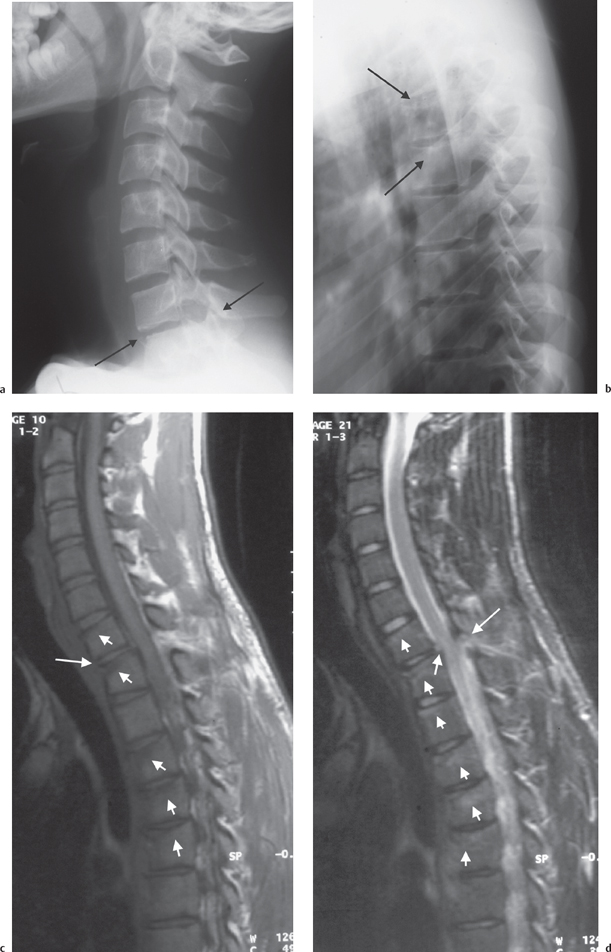
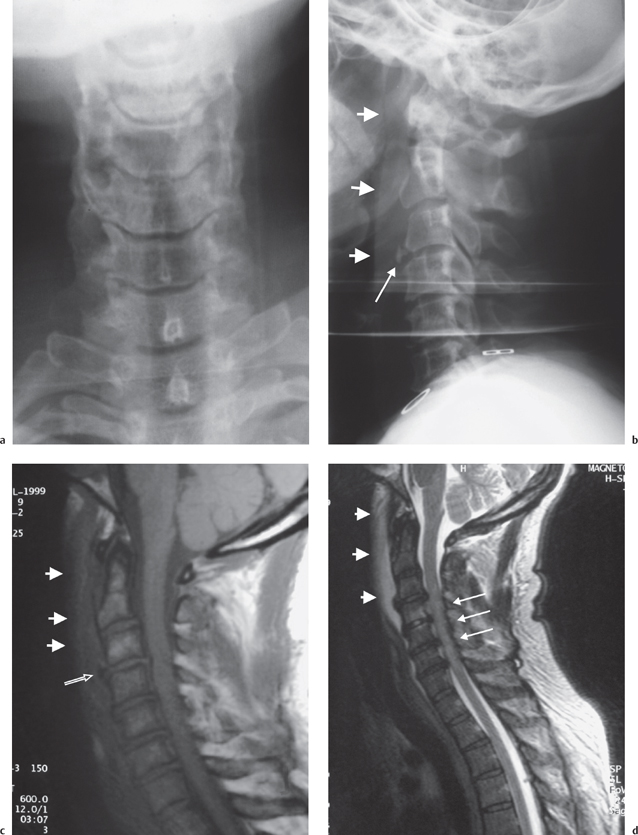
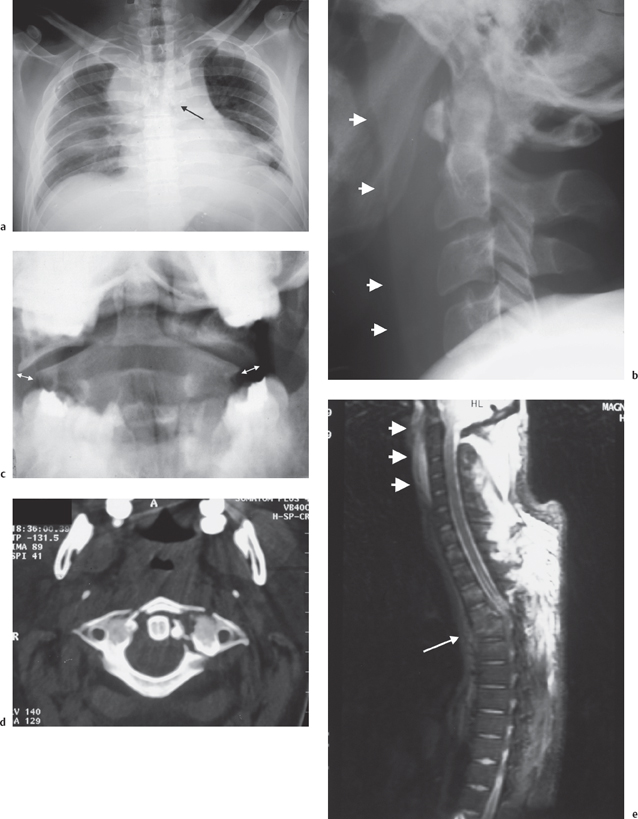
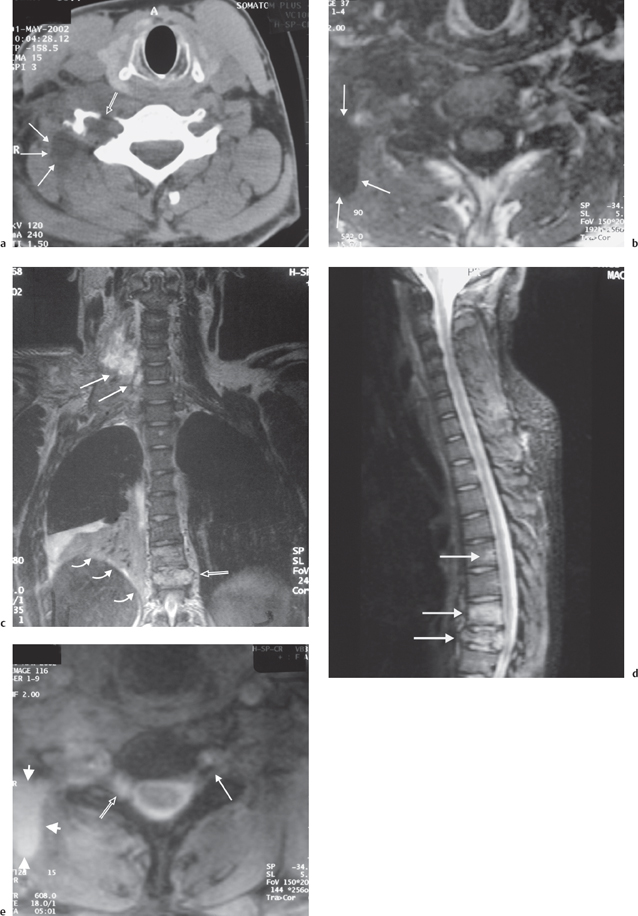
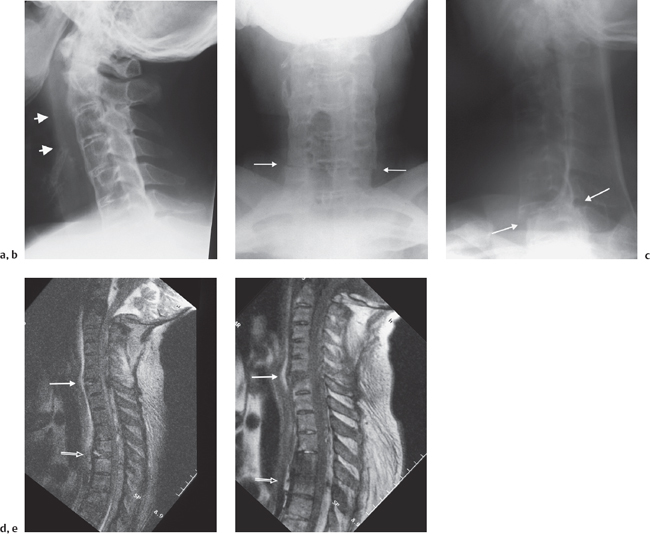
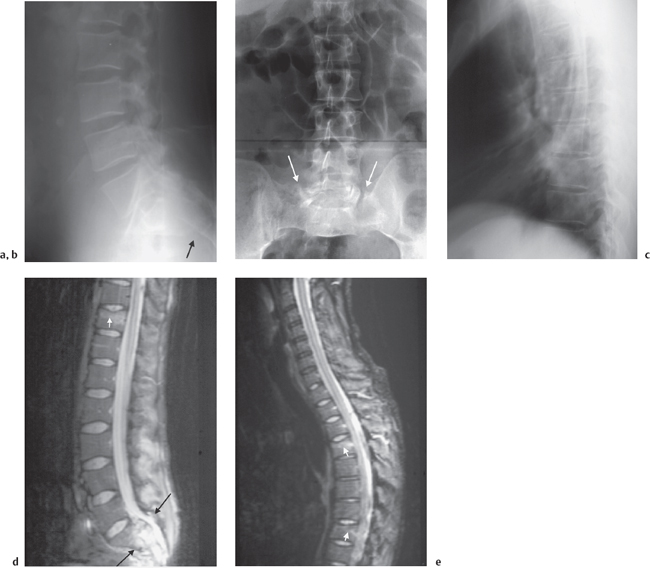
Introduction Spinal injuries are potentially devastating for the patient and pose a challenge for the clinicians involved in patient care. They require a conjoined approach of several clinical specialties. Imaging plays an important role in establishing the diagnosis, giving a prognosis, aiding treatment, and in the further follow-up of spinal injury patients. The imaging approach will vary with the clinical scenario. An unconscious polytraumatized patient with head, thoracic, and abdominal injuries will probably undergo multi-detector row CT of head, neck, thorax, abdomen, and pelvis with dedicated reconstructions of the spine.1–4 On the other hand a patient who could be classed as “walking wounded” with minor trauma and perhaps some neck ache will probably be assessed according to the guidelines of the Canadian C-spine rule (Tabs. 3.1–3.3, p. 46) to establish whether any imaging investigation is indicated.1, 5 The guiding principle for any assessment of the spine is to diagnose or exclude significant spinal injury utilizing the imaging modalities available in a cost-effective manner while keeping the radiation dose to the patient as low as possible. Missing a significant spinal injury can have disastrous consequences with neurological deterioration reported in as many as 10 to 50% of missed spinal injuries.6–9 Earlier studies on patients with significant spinal injuries found that in between 4.6% and 10.5% of patients significant spinal injuries were initially missed.6–9 This emphasizes the importance of a diligent approach to the diagnosis of spinal injuries. The role of the radiologist does not commence with image interpretation but before that by helping to determine an optimized imaging strategy for a given clinical scenario. Frequently the radiologist will be asked to establish whether a spinal injury is present but he or she might also be asked specific questions as for example the state of a particular nerve root or the extent of cord damage (Figs. 3.1, 3.2). The imaging approach will vary in these circumstances and the radiologist needs to be aware of the advantages and disadvantages of the various imaging modalities in different phases of patient work-up and treatment. This subject is reviewed fairly regularly in the radiological and trauma care literature and this chapter tries to distill the recent trends for the reader.10–13 This chapter does not offer a dogmatic, overly prescriptive view on imaging of spinal injuries. Any approach will depend on local facilities, philosophy, and expertise. Fig. 3.1 24-year-old male patient after a motorbike accident. Neurologically intact! A radiograph demonstrates a grossly displaced segment of the lower thoracic spine (a). CT demonstrates shearing off of the anterior part of the vertebral body with preservation of the spinal canal (b). This is well demonstrated on surface-shaded reconstructions (c). Coronal MRI demonstrates the intact spinal cord (d). Imaging confirmation of an intact spinal canal and cord resulted in conservative treatment only with an uneventful recovery. Fig. 3.2 21-year-old male, road traffic accident. Right-sided C7 and C8 weakness. A lateral radiograph (a) demonstrates a C7 fracture (arrows) but the injury and its extent are difficult to appreciate. MRI (b) demonstrates a burst fracture of C7 and spinal cord edema. Fig. 3.2c-f The right paramedian plane (c) demonstrates a bone fragment protruding into the spinal canal (arrow) but no further cord compromise. Axial CT (d) and CT reconstructions (e, f) show this fragment to be in the intervertebral foramen (arrows). This was difficult to appreciate on MR and underlines the complementary nature of CT and MR imaging. Radiography was traditionally the mainstay of imaging examinations performed for spinal injuries work-up. Unfortunately, this imaging modality is neither particularly sensitive nor specific. Particularly in the imaging of cervical spine injuries the unreliable nature of radiographs for the diagnosis or exclusion of significant injuries has been well documented. It is now accepted that about 10-20% of significant cervical spine injuries are missed with radiographs.6,14–16 Suboptimal radiographs and errors in image interpretation account for a large number of these but some injuries are missed even in retrospect as they are not visible on the initial radiographs (Fig. 3.3).6–9,14,15,17–19 Compared to CT, the diagnostic performance of radiographs is relatively poor in the cervical as well as the remainder of the spine.23–28 About 10-20 % of significant injuries of the cervical spine are missed radiographically when compared with CT, but the absolute number of missed injuries is even higher and most studies quote a number of around 60%.16,20,29–32 For single detector row CT, conventional rather than helical acquisition was found to be more sensitive33 while more recently multi-detector row CT was found to be superior in fracture detection to single-slice CT with its increased speed and z-axis resolution.34 MRI is particularly useful in diagnosing soft tissue spinal injuries including the spinal cord, and injuries to vertebral bodies by demonstrating marrow edema (Fig. 3.4). Injuries to cortical bone are not well depicted unless there is displacement (Figs. 3.5, 3.6). MRI is cumbersome for immobile patients and patients needing close medical supervision. It is also much more time consuming than radiographs and CT. Imaging protocols have to be tailored for specific areas unlike CT where the new generation scanners can image almost the entire body in less than a minute. Recently multi-detector row CT (MD-CT) has been increasingly advocated for C spine clearance also in obtunded patients.35,36 Flexion and extension views of the spine have been studied for cervical spine clearance of obtunded and alert patients. In alert patients there is no role for this technique in the acute phase due to muscle spasm.37,38 However, they are useful for delayed imaging for persistent complaints at about two weeks after an injury when the initial radiographs are normal.38–42 Their use in obtunded patients is controversial. There is no supportive literature (and no role) for the use of flexion/ extension views in the acute diagnosis of lumbar or thoracic spinal injuries. Fig. 3.3 20-year-old male. He was ejected from his vehicle > during a high-speed traffic accident. Radiographs were taken, no injury was seen and he was discharged from hospital. Two weeks later he presented to a GP for persisting numbness and weakness of his lower limbs. A lateral radiograph (a) demonstrates anterior subluxation of C7 (arrows). This injury is easily (and was initially) missed if the cervicothoracic junction is not included on the view. The lateral view of the thoracic spine (b) demonstrates mild wedging of upper thoracic vertebrae (arrows) but they are not well visualized. T1W (c) and T2W (d) MR images demonstrate the complete disruption of the ligamentous structures at the C7/T1 level (arrows) and infraction of the superior endplates of C7, T1-T5 (arrowheads). Post-traumatic cord signal change. Only mild soft tissue swelling 2 weeks after the injury. Radiography is universally available, familiar to doctors of all specialties and experience level and can be performed in the trauma room. It can be difficult though to obtain images of adequate quality, the interpretation requires skill and experience (more than often appreciated), soft tissue trauma is often missed (unless associated with significant bony malalignment or soft tissue swelling), and bone trauma is also frequently missed. The upper cervicocranial junction and the upper thoracic spine are notoriously difficult to image (Figs. 3.3, 3.7).6,14–16,20–28,43 CT is much more sensitive in depicting bone trauma when compared to radiographs and allows for better assessment of the extent and nature of the bone trauma (Fig. 3.2). Two dimensional reformatted images of the spine can be the by-product of CT imaging of head, thorax, abdomen, and pelvis when cranial and visceral injuries are suspected.4,23–28,43 If the C-spine is included in such cases, the entire spine is imaged making radiographs of the spine unnecessary.2,43 Nevertheless, regardless of the technical protocol, CT can miss bony injuries and has been found to perform poorly in the assessment of spinous or paraspinous soft tissues.28,29,39,44–53 More recently MD-CT has been examined as the sole imaging modality for clearance of the cervical spine in obtunded trauma patients.35,36 It was found that MDCT did not miss unstable injuries in either study. Other studies looked at using only MD-CT for clearance of the cervical spine for patients presenting without motor deficit.54 Obtunded patients who were moving all their limbs on admission were assessed.55 It was suggested that CT is sufficient to clear the cervical spine with regard to unstable injuries in these patients. The number of ligamentous injuries in these studies was low. A recent review of the literature on assessing the cervical spine in obtunded trauma patients56 also makes this point and specifically cites a risk of missing about 0.5% of unstable cervical spine injuries in obtunded trauma patients. MD-CT does not image ligamentous injuries directly and relies on secondary signs such as alignment, extent and location of soft tissue swelling, and nature and location of bony injuries to draw conclusions about stability. Another interesting point raised in this review is the relative higher frequency of ligament injuries needing surgical treatment in the MRI and fluoroscopy based studies when compared to CT of the cervical spine. This suggests that CT does miss ligamentous injuries that would receive surgical treatment if imaged and diagnosed with MRI. The good clinical outcome of these limited CT-based studies suggests that despite no treatment ligamentous injuries that would normally be treated surgically do heal without neurologic sequelae. A further diagnostic concern in the obtunded patient not addressed by any imaging modality except MRI, is spinal cord injury without radiographic or CT abnormalities. If the patient is admitted to a center whose treatment policy includes the administration of steroids, then this type of injury must be diagnosed early. However the limited studies of CT-based assessment of the cervical spine in obtunded patients do not suggest a worse outcome. Unless there is a reason to image the entire spine, CT examinations are usually limited to a specific area for radiation protection concerns. Noncontiguous spinal injuries are surprisingly common and are seen in up to 50 % of patients (Figs. 3.5–3.7). They are easily missed if the entire spine is not imaged in a patient with an acute spinal injury.2,16,57–60 MRI does not utilize ionizing radiation. As long as there is no contraindication, there is no detrimental effect to the patient. MRI is excellent for the imaging of soft tissue injuries but relatively poor in the depiction of bony injuries (Fig. 3.6).29,39,44–53,61 This is true particularly for injury to the posterior elements where one study found a sensitivity of MRI compared to CT of only 11.5%.45 The exception is the imaging of bone compression injuries without cortical disruption where marrow edema sensitive sequences frequently find bony injuries not appreciated on radiographs or CT.57 MRI is of prognostic value in the assessment of spinal and spinal cord injuries.62–64 In general though it is not the first line of investigation as it is expensive, access is limited, and the examination of severely traumatized patients or any patient needing close medical supervision is logistically demanding. On the other hand, early exclusion of unstable spine trauma can greatly facilitate further diagnostic and therapeutic planning and nursing care. Usually the role of MRI lies in the exact determination of the extent of spinal injuries initially diagnosed by other imaging methods. Here it is particularly valuable in defining the extent and severity of soft tissue (i. e. ligament and spinal cord) injuries and in identifying bone marrow edema (indicating bone trauma) in other areas of the spine (Figs. 3.5–3.8).57 Cases of neurological deficits with no explanatory imaging evidence have been described48,49 though usually MRI imaging will reveal a spinal cord abnormality (Fig. 3.4).16,39,44,46,48,49,51,52,65 Some patients, however, do have contraindications for MRI imaging, for example cardiac pacemakers, intracranial surgical clips or cochlear implants. CT and in some cases CT myelography might be of help here as well as flexion/extension views of the cervical spine. Fig. 3.4 57-year-old female patient, horse riding accident. Weakness of all extremities, difficulty with bladder and bowel control. Radiographs of the cervical spine (a, b) demonstrate chronic spondylotic change with prevertebral soft tissue swelling (arrowheads) and an avulsed osteophyte (arrow) of the anteroinferior corner of C3. MRI in T1W (c) and T2W (d) one day later confirms prevertebral soft tissue edema (arrowheads). The avulsed osteophyte is visible (arrow) but difficult to appreciate compared to the radiograph. Multi-level high signal change of the spinal cord is seen (open arrow) but no disruption of the spinal column. Diagnosis: central cord syndrome after trauma in a degenerate spine. Fig. 3.5 30-year-old male involved in a road traffic accident. T4 complete paraplegia. A chest radiograph (a) shows mediastinal widening, a large pleural collection, and fractures of the thoracic spine at the T4 and T5 level (arrow). A lateral view of the cervical spine (b) demonstrates prevertebral soft tissue swelling (arrowheads), the peg view (c) shows splaying of the atlas (double arrows). CT confirms the complex fracture of the atlas (d). The C1 fracture was difficult to appreciate on MRI (e), but soft tissue edema and hemorrhage (arrowheads) indicate an upper cervical injury in addition to the T4 and T5 vertebral body fractures (arrow). Bone marrow edema indicating further infraction in multiple further vertebrae. Fig. 3.6 33-year-old male involved in a road traffic accident with signs of right brachial plexus injury. A right-sided transverse process fracture of C6 was well demonstrated on CT (a; open arrow) but difficult to appreciate on MRI (b). The vertebral artery was proven to be intact. Low attenuation/signal areas signify CSF leakage after nerve root injury (arrows in a, b). Multiple nerve root swere affected. This is best appreciated oncoronal MR images (c), which are best suited to imaging the brachial plexus (arrows). These demonstrate a further crush fracture of the T8 vertebral body (open arrow) and marrow edema in T7, right basal lung consolidation(curved arrows) and right-sided pleural collection. A sagittal STIR MR image of the spine (d) confirms the structural integrity of the cervical spine and spinal cord with lower thoracic fractures (arrows). Anaxial MR image (e) of the C7/T1 intervertebral foramen demonstrates the nerve root on the left (arrow) and the absence of the nerve root on the right (open arrow) and adjacent CSF collection (arrowheads). This case demonstrates the association of brachial plexus injuries with spinal injuries. Fig. 3.7 57-year-old male. Known ankylosing spondylitis and thrombocytopenia with complete ossification of the spine. The patient had a history of collapse. A lateral radiograph of the cervical spine (a) demonstrates prevertebral soft tissue swelling (arrowheads) but no obvious fracture. However, the spine is only imaged to the C6 level. An AP (b) and a swimmer’s view (c) demonstrate a C6/7 fracture dislocation (arrows). MRI of the spine in sagittal STIR (d) and T1W (e) images shows the C6/7 fracture dislocation (arrow) and a further fracture/ dislocation at the T4/5 level (open arrow). There is also significant epidural hematoma. Fluoroscopic flexion and extension views of the cervical spine in the acute phase in obtunded patients seem to be able to exclude significant local instability when performed by experienced clinicians in a dedicated setup.56,66,67 Some authors disagree with this view68–70 but the key to success seems to be a dedicated setup and clarity about the aim of this examination. Despite suggestions to the contrary, this type of study should not be performed as radiographs in flexion and extension, and does not exclude all injuries but merely aims at excluding significant instability. As pointed out in a recent commentary72 the studies performed suffer also from small numbers.63 This makes a meaningful assessment of complication rates difficult. Logistically this examination is easier to perform than MRI. However, it cannot demonstrate cord compression by a dorsal disk herniation and cannot exclude or diagnose a cord injury. Hence, its usefulness for patient management is limited and it is potentially detrimental to the spinal cord. An excellent review of the literature concluded that as yet there is no clear evidence to either favor dynamic fluoroscopy or MRI of the cervical spine to assess stability in obtunded patients. The authors suggest that the inherent advantages of MRI favor this examination where available.56 Fig. 3.8 37-year-old male. Motorbike accident. Radiographs (a, b) demonstrate a severe sacral fracture (arrows). Subtle endplate changes in the thoracic spine (c) are difficult to appreciate on the radiograph. MRI (d, e) demonstrates the sacral fracture (arrow) and several noncontiguous thoracic fractures (small arrows). Sacral fractures have a known association with injuries in other areas of the spine. As the facts presented so far show, the biggest problem in the imaging of spinal injury patients is the choice of the appropriate imaging modality in the different stages of patient care. If a spinal injury is identified by any one imaging modality, further imaging with other modalities is often indicated to complement or offset the specific constraints of the modality initially employed. For the clinician in charge of the patient, prognostic information is of particular importance. Older classification systems of spinal injuries such as the Holdsworth and the Louis classification were based on radiographic findings.73 Newer classification systems such as the AO classification and partly the Denis classification are based on radiographic as well as CT findings.73 However, there remain significant shortcomings, and a new classification system based on the combination of all imaging modalities appears necessary.74

Imaging Modalities
Pros and Cons
Imaging Approaches and Dilemmas
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree