Localization: The lesion is almost exclusively localized in the shaft of the tibia, occasionally involving the ipsilateral fibula, too. Exceptionally it is bilateral in tibias and fibulas.
Clinical: The symptoms are moderate expansion of the bone, anterior or valgus-varus bowing of the diaphysis. The lesion is painless. Stress and pathologic fractures are not uncommon, but pseudoarthrosis is exceptional.
Imaging: It shows a typically intracortical osteolysis, more frequently involving the anterior (occasionally valgus-varus) cortex, and often associated to an anterior bowing of the diaphysis. The cortex is regularly and moderately expanded, very thin, and with a smooth surface. Toward the medulla, instead, the osteolysis is bordered by a rim of sclerotic bone, so that the medullary canal is frequently narrowed or closed. The osteolysis can be multiple and having a multilocular or bubbly appearance. Some of the osteolyses are veiled by a tenuous ground-glass radiodensity.
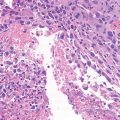
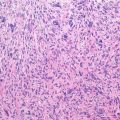
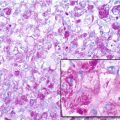
Pathology: Histologically, it is characterized by a fibrous tissue, embedding small trabeculae of woven bone, rimmed by cubic osteoblasts. The fibrous component is less cellular as compared to active fibrous dysplasia, with delicate collagen, occasionally with a storiform pattern, or focally fibro-myxoid. The bone trabeculae tend to be sparse, thin, and woven in the center of the lesion, and to gradually become more abundant, anastomosing, and lamellar toward the periphery, where both the trabeculae and the fibrous tissue blend with the surrounding host bone (zonal architecture). Exceptionally, small foci of hyaline cartilage have been found. The immunohistochemical studies may show isolated cells, small nests, or microscopic tubes stained with the keratin antibodies. These cells are not obvious in the hematoxylin-eosin stain.
Course and Staging: The lesion may progress considerably in the first years of life, and thereafter stabilizes and, after 10–12 years of age, slowly repairs through peripheral bone thickening. The pathologic fractures do regularly united. Congenital pseudoarthrosis is not a feature of this disease.
Treatment and Prognosis: Attempts to intralesional excision before the lesion has stabilized are regularly followed by local recurrence. Surgery (not even biopsy) is usually not indicated. The child should be protected, when indicated, by bracing, and monitored, until spontaneous repair occurs. The prognosis is good, except for the more severe cases ending up with leg deformity and shortening. A small subset of these patients can develop into adamantinoma. This exceptionally occurs in children, rarely in adolescent and young adults.
Key Points
Clinical
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|