Etiology
Traumatic
Talar neck fracture
Talar body fracture
Nontraumatic
Steroids
Alcohol
Systemic lupus erythematosus
Hyperuricemia
Renal transplantation
Sickle cell anemia
Hyperlipidemia
Pancreatitis
Iatrogenic
56.3 Blood Supply of the Talus
The blood supply comes mainly from the extraosseous and the intraosseous circulation [14, 15]. The extraosseous circulation, with contributions from the anterior tibial, posterior tibial, and peroneal artery, forms a vascular extraosseous ring around the talar neck and sinus tarsi [14, 15]. The artery of the tarsal canal, a branch of the posterior tibial artery, provides the main blood supply to the body of the talus [16, 17] (Fig. 56.1). Deltoid and posterior tubercle branches from the posterior tibial artery enter the medial talar body and posterior tubercle, respectively [15]. The artery of the sinus tarsi, a branch of the peroneal artery, runs from lateral to medial inferior to the talar neck and eventually anastomoses with the artery of the tarsal canal to form a vascular “sling” beneath the neck of the talus [2]. The dorsalis pedis artery contributes to several branches that enter the talus through the superior neck [16]. The intraosseous anastomoses are variable among individuals and may explain why some patients develop osteonecrosis of talus and while others do not [15, 18]. A complete intraosseous anastomosis between all regions of the talus has been found in 60 % of talar anatomic specimens [14–16]. The talar head has an abundant vasculature, supplied primarily by the anterior tibial artery [14, 16].
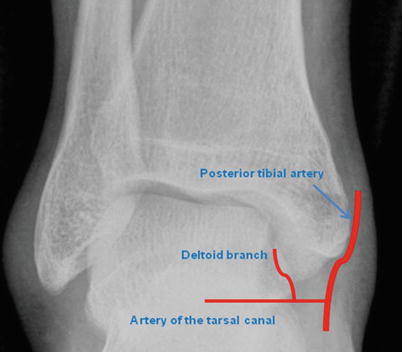
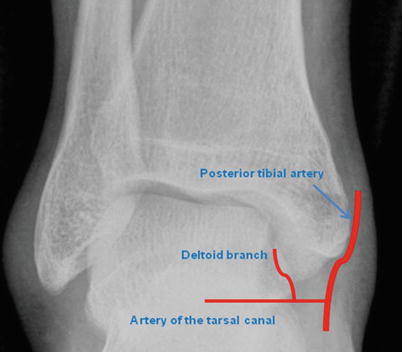
Fig. 56.1
Blood supply of the talus
56.4 Clinical Presentation
Clinicians should obtain information from patients by careful history taking of trauma, medical history, steroid use, systemic disease, and immunologic disorders. In early precollapse period, patients complain of their ankle pain predominantly [2]. With more advanced disease, articular collapse can lead to mechanical symptoms, such as locking and catching. Physical examination may be unremarkable, especially in early precollapse period. In postcollapse period, however, a joint effusion and joint line tenderness usually can be detected. In severe cases that are characterized by talar dome collapse, range of motion is limited and varus or valgus malalignment may be present [2].
56.5 Diagnostic Imaging
56.5.1 Radiographs
Despite the advent of more advanced imaging modalities, radiographs still play a critical role in the evaluation of osteonecrosis of the talus [2]. The body’s response to osteonecrosis is an attempt at repair by means of reossification, revascularization, and resorption of necrotic bone [19]. At initial radiography, necrotic bone and the surrounding viable bone are equal in opacity, and early stages can be missed [20]. As time passes and hyperemia results, healthy bone is resorbed and subsequently becomes osteopenic [20]. Conversely, the lack of blood supply in necrotic bone prevents its resorption, making necrotic bone appear more radiopaque than the surrounding osteopenic bone. At that point, radiographic evidence of osteonecrosis becomes apparent. The opacity of necrotic bone continues to increase as reossification occurs and new bone is laid down over necrotic trabeculae. This process accounts for the typical sclerotic image seen in osteonecrosis of the talus. In addition to reossification, revascularization and resorption also tend to occur around necrotic bone. When these processes occur, a radiolucent rim becomes apparent around the area of osteonecrosis [19, 21]. Radiographs are especially useful following open reduction and internal fixation of displaced talar neck and body fractures [2]. Hawkins’ sign is characterized by subchondral osteopenia on anteroposterior or mortise radiographs [3]. Typically, it is present at 6–8 weeks and results from the resorption of subchondral bone in the setting of disuse and a sufficient vascular supply [3]. Canale and Kelly evaluated the reliability of Hawkins’ sign at 12 weeks postoperatively in 49 patients [4]. They found that 20 of 26 (77 %) fractures that did not have subchondral osteopenia developed osteonecrosis. However, one of 23 cases that had a positive Hawkins’ sign went on to osteonecrosis. Thus Hawkins’ sign is a reliable indicator of talar viability and its presence serves as an early negative predictor of osteonecrosis [2–4]. The absence of Hawkins’ sign, however, does not confirm osteonecrosis, because it has greater sensitivity than specificity [2–4].
56.5.2 MRI
MR imaging is the most sensitive technique for detecting osteonecrosis of the talus, especially in the early stages [20]. In addition, MR imaging is considered more anatomically detailed and accurate than radiographs and scintigraphy in its ability to identify the extent of talar body involvement [22]. On MR imaging, osteonecrosis of the talus typically is characterized by low signal on T1-weighted images [2]. On T2-weighted images, osteonecrosis produces a mixed and variable appearance that depends on the contents of the avascular region [2]. However, MR imaging non-contrast enhanced is a problem due to the confusing picture of bone edema and ONT having a similar appearance [23]. We recommend MR imaging with contrast such as gadolinium enhancement for accurate diagnosis on early stage of ONT and should be combined with the clinical findings.
56.5.3 Computer Tomography
Computer tomography (CT) scans also reveal characteristic osteonecrosis of the talus patterns and can be used to confirm radiographic findings. The CT arthrogram is a especially helpful method to evaluate the volume and location of the remaining dead bone and associated cartilage damage [23]. Coronal CT of the talus is required for viewing the articular surface of the talar dome to rule out subtle depression, collapse, and fragmentation, especially at preoperative assessment [20] (Fig. 56.2).
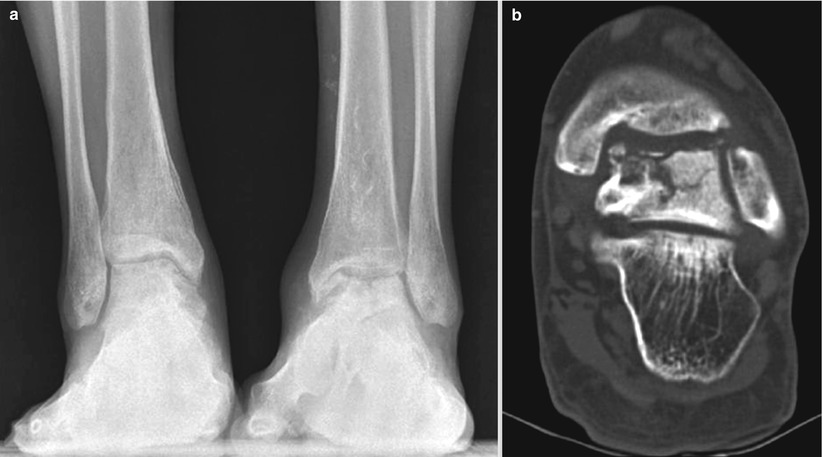
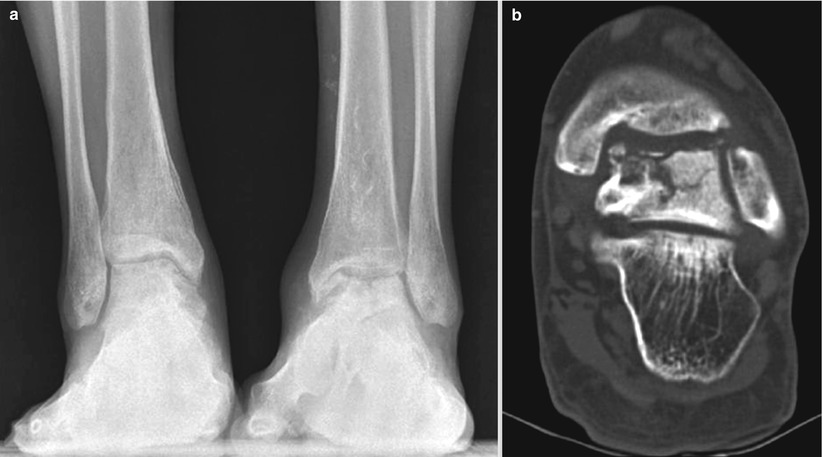
Fig. 56.2
(a) Both ankle anteroposterior radiograph while standing of a 33-year-old woman who had a 1-year history of pain in the ankle and loss of motion. She was receiving steroids for systemic lupus erythematosus more than 10 years with 12.5 mg qd. She underwent total hip arthroplasty bilaterally, because of the osteonecrosis of the femoral head. There is a collapse of the talus and joint space narrowing, subchondral sclerosis of the tibia on her left ankle (stage IV osteonecrosis, according to the system of Ficat and Alert modified for the ankle by Mont), and focal radiolucent lesion, subchondral cyst, and subcondral sclerotic change of the talus were shown in her right ankle (stage II). (b) Coronal CT scan of the left ankle shows collapse of the articular surface of the talar dome, vertical and horizontal split fracture extending from the talar dome into the talar body. Also there is sclerotic line within the talar body that represents necrotic bone
56.6 Classification
Mont et al. [24] classified osteonecrosis of the talus with the system of Ficat and Arlet, as modified for the ankle. A stage I is characterized by normal radiographs, whereas stage II disease is characterized by cystic or osteosclerotic lesions, normal talar contour, and no subchondral fracture. With stage III disease there is a crescent sign or subchondral collapse, and with type IV disease, arthritic changes are present. The investigators used this staging system as a general guide to treatment and divided cases into either “precollapse disease” (stages I and II) or “postcollapse disease” (stages III and IV).
Thordarson et al. [22] went on to develop a classification system of osteonecrosis that is based on the amount of talar body involvement on MR imaging. Type A has homogeneous signal throughout the body of the talus, type B has signal changes in up to 25 % of the body of the talus, type C has 25–50 %, and type D has more than 50 %. This system was used to guide postoperative weight bearing following open reduction and internal fixation of talar neck fractures. If less than 25 % of the body was involved (type A or B), weight bearing was advanced as tolerated. If more than 25 % of the body was involved (type C of D), protected weight bearing for upward of 6 months was recommended.
56.7 Treatment
56.7.1 Conservative Treatment
The presence of osteonecrosis of the talus before collapse is initially treated nonoperatively. The nonoperative treatment options include applying a short-leg cast, ankle-foot orthosis with analgesics, and no weight bearing [25]. Some previous studies recommend extended non-weight bearing [3, 26]. Others have recommended a patella tendon bearing brace until reconstitution of the talar body is complete [27–29]. However, because the creeping substitution of the talar body can require 36 months to occur, patient compliance is rarely possible for 36 months [1, 30]. Penny et al. [31] reported that weight bearing on sclerotic and osteonecrosis of the talus poses no danger for talar dome collapse and found no relation between poor results with osteonecrosis of the talus and time of non-weight bearing. Therefore, the current consensus is to permit weight bearing as soon as tolerable.
56.7.2 Surgical Treatment
Several treatment options are available for osteonecrosis of the talus. However, surgical treatment options for symptomatic osteonecrosis of the talus are limited. These are core decompression, allograft reconstruction, vascularized autograft reconstruction for early precollapse stage, and arthrodesis and arthroplasty for late postcollapse stage [24, 25, 32–38].
56.7.2.1 For Early Precollapse Stage
Core Decompression
Core decompression is a surgical treatment for the early stage of osteonecrosis. The rationale for core decompression is that it decreases intraosseous pressure and may immediately relieve the associated pain [25]. Mont et al. [24] reported on 17 ankles who had core decompression for symptomatic osteonecrosis of the talus before collapse, with 82 % having an excellent or good outcome. The authors concluded core decompression is a viable method of treatment for symptomatic osteonecrosis of the talus before collapse. Recently Marulanda et al. [39] reported that the percutaneous drilling technique appears to be a satisfactory method for treating osteonecrosis of the talus and is associated with low operative morbidity.
Allograft Reconstruction
Osteonecrosis of the talus involving only the talar dome with ankle joint arthritis can be addressed with fresh osteochondral total ankle allograft transplantation [1]. Gross et al. [33] reported nine cases of osteochondral defects of the talus treated with fresh osteochondral allograft transplantation. All underwent partial talar allograft transplantation and the survival rate at 11 years was six out of nine patients. Jeng et al. [34] reported 29 patients that underwent bipolar osteochondral allograft, including two patients with osteonecrosis of the talus treated, and had 50 % success rate. However, there are no long-term results for talar allograft survival rates.
Vascularized Autograft Reconstruction
Hussl et al. [35] reported use of a vascularized bone graft from the iliac crest for revascularization of the talus in posttraumatic osteonecrosis. Gilbert et al. [36] reported 14 fresh-frozen cadaver lower extremities and were able to identify a consistent blood supply to the distal fibula, cuboid, and cuneiforms I and III with reliable nutrient arteries. The transverse pedicle branch of the proximal lateral tarsal artery reached and supplied the cuboid in every specimen. The first cuneiform was found to be supplied by the middle pedicle branch of the distal medial tarsal artery. Basically, the same is true for the next pedicle of the transverse branch to the third cuneiform off the distal lateral tarsal artery. The fourth potential vascular pedicle was a transverse segment of the anterior lateral malleolar artery to the lateral malleolus. The identification of these new rotational vascular pedicle bone grafts could help to treat osteonecrosis of the talus using a vascularized bone graft. Zhang et al. [37] reported on the curative effect of vascularized bone graft in the treatment of 24 cases, with success rate of 83.3 % at 3–5 years follow-up. There are no long-term results yet.
56.7.2.2 For Late Postcollapse Stage
Arthrodesis
Ankle arthrodesis is a reliable treatment for osteonecrosis of the talus with collapse in cases where symptoms are isolated to the ankle joint [32, 40]. Sufficient talus bone stock following debridement of the osteonecrosis is required for adequate fixation of the ankle joint [1]. Structural defects of the talus are filled with a structural auto- or allograft. Standard fixation for ankle arthrodesis includes multiplanar screws or plate fixation [1]. Prior study report a union rate of 96 % with anterior plate fixation [1]. Antegrade nailing of the ankle joint has been described, but with suboptimal results because of bad fixation in the talus [1]. External fixation has also been used to achieve an ankle fusion [41]. A recent systematic review of intermediate and long-term outcomes of ankle arthrodesis noted that nonunion was observed in 10 % of the patients treated with ankle arthrodesis and 9 % of the arthrodesis group underwent revision [42]. Thus, recently, higher success rates have been achieved using various techniques. Success of ankle arthrodesis also depended on patient factors. Ankle arthrodesis is technically challenging for osteonecrosis of the talus comorbid rheumatoid or osteoarthritis because of the difficulty in achieving well-vascularized bony surfaces for fusion [32]. Frey et al. [43] reported that eight of nine patients showed nonunion. Another study also showed low fusion rate, 38 % in such patients [44]. Therefore ankle arthrodesis is technically demanding and requires a longer period of immobilization for patients with rheumatoid or osteoarthritis compared with other patients [32, 43, 44]. In cases of severe talus collapse, tibiocalcaneal arthrodesis with talectomy and tibiotalocalcaneal arthrodesis were some kind of methods for hindfoot arthrodesis [45]. Tibiocalcaneal arthrodesis was needed to remove the entire talar body, so without structural grafting, this method has poor results because it shortens the leg [45, 46].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree