and Zdeněk Fryšák1
(1)
Department of Internal Medicine III – Nephrology, Rheumatology and Endocrinology, Faculty of Medicine and Dentistry, Palacky University Olomouc and University Hospital Olomouc, Olomouc, Czech Republic
Keywords
Thyroid lymphomaHashimoto’s thyroiditisThyroid glandExtramedullary plasmacytomaEchogenicityLong-to-short axis ratioHilus sign18.1 Other Malignancies in Thyroid Gland and Cervical Lymph Nodes: Primary Thyroid Lymphoma
18.1.1 Essential Facts
In a large Swedish retrospective study (between 1959 and 1981) of 829 patients with chronic lymphocytic thyroiditis (CLT), the risk of malignant thyroid lymphoma was greatly increased, with an estimated relative risk of 67 (4 observed vs. 0.06 expected). There was no increased risk among patients with colloid goiter [1].
Primary thyroid lymphoma (PTL) is a rare cause of malignancy, accounting for <5% of thyroid malignancies and <2% of extranodal lymphomas, with an annual estimated incidence of 2 per 1 million. Women are more commonly affected than men (2–8:1). Patients typically present in the sixth or seventh decade of life, with men often presenting at a younger age than women [2].
Most thyroid lymphomas are non-Hodgkin’s lymphomas (NHLs) of B-cell origin. Patients with Hashimoto’s thyroiditis (HT) are at greater risk for developing PTL, with a relative risk of 67 compared to those without HT [2].
The transformation from HT to PTL occurs in about 0.5% of cases. Approximately 60–90% of PTL cases arise in a background of HT [2].
Clinical manifestation of PTL is known as a rapidly growing mass arising in the middle-age-to-elderly phase of life, in hitherto asymptomatic female patients with a history of longstanding HT [3].
Although PTL may grow suddenly and be life-threatening due to airway obstruction, early detection and diagnosis followed by appropriate treatment can lead to favorable prognosis [2, 3].
In a retrospective study by Graff-Baker et al. of 1408 patients with PLT identified over 32 years of follow-up, a total of 88% had stage I–II disease; median survival was 9.3 years, a 5-year survival of 90% [4].
18.1.2 US Features of Primary Thyroid Lymphoma [3, 5]
PTL can be divided into three types based on internal echoes, borders, and posterior echoes: nodular, diffuse, or mixed.
Enhanced posterior echoes are present in all three types and help to distinguish lymphoma from other types of thyroid lesions.
In the nodular type (Fig. 18.1aa), the goiter is usually unilateral with internal hypoechoic, homogeneous, and pseudocystic lesion. Well-defined borders separate lymphomatous lesions from nonlymphomatous tissues.
In the diffuse type, the goiter is bilateral and diffuse heterogeneous exceedingly hypoechoic parenchyma with intervening echogenic septa-like structures. In contrast to the nodular type, the border between the lymphoma and nonlymphomatous tissue could not be clearly identified.
The mixed type of lymphoma shows multiple patchy, hypoechoic lesions.
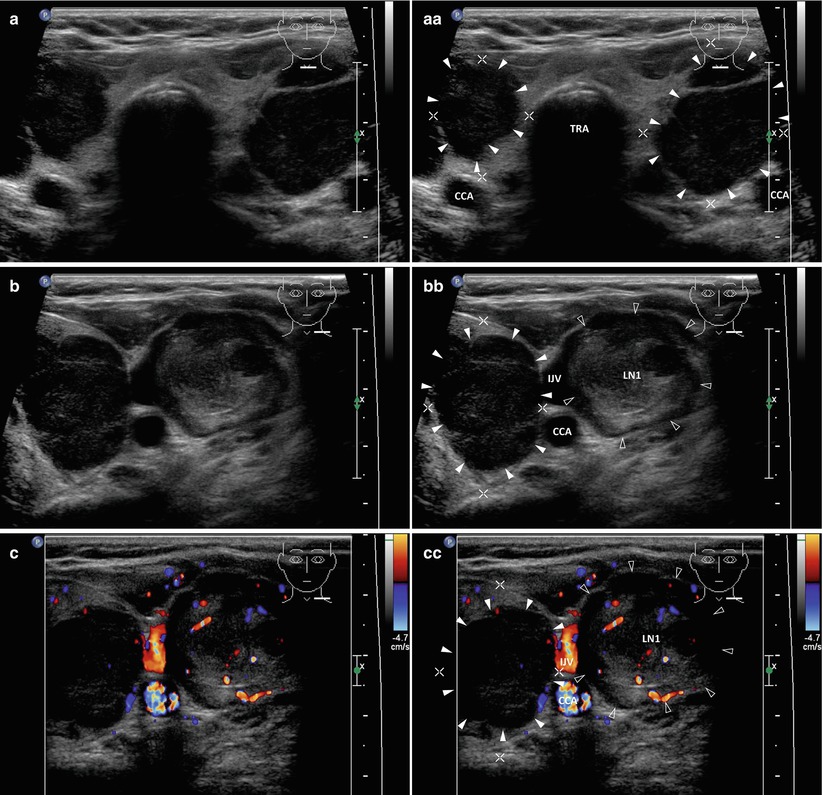


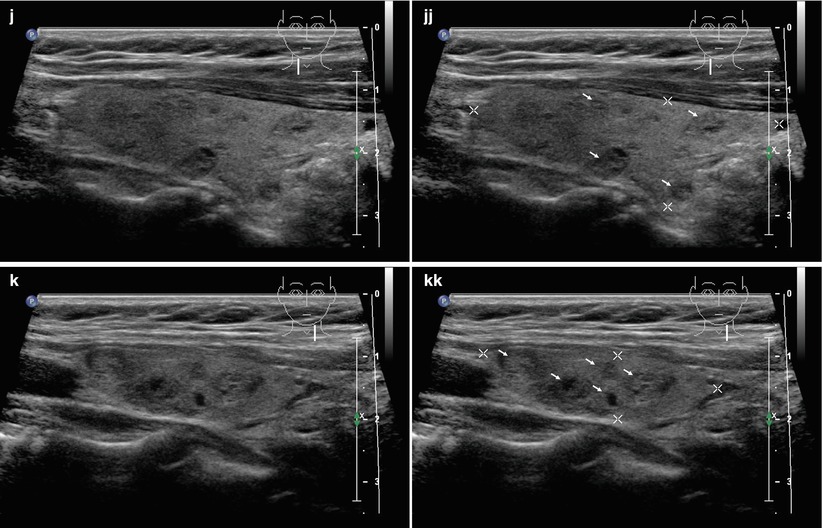
Fig. 18.1
(aa) A 70-year-old woman with secondary Non-Hodgkin lymphoma of thyroid gland and malignant cervical lymph nodes (LNs): suspicious solid nodule (arrowheads) in the RL, size 20 × 18 × 16 mm and volume 3 mL—round shape; inhomogeneous structure; markedly hypoechoic; microlobulated margin; suspicious solid nodule (arrowheads) in the LL, size 33 × 24 × 20 mm and volume 8 mL—ovoid shape; inhomogeneous structure; markedly hypoechoic; microlobulated margin; Tvol 48 mL, RL 21 mL, and LL 27 mL; transverse; depth of penetration 4.5 cm. (bb) Detail of a suspicious nodule in the LL and malignant LN next to the left IJV at level C-III: solid nodule (arrowheads)—inhomogeneous structure; markedly hypoechoic; microlobulated margin; malignant LN1 (blank arrowheads)—oval shape; size 23 × 20 mm; coarse structure; mixed echogenicity, mostly hyperechoic with hypoechoic areas; transverse. (cc) Detail of suspicious nodule in the LL and malignant LN1 next to the left IJV at level C-III, CFDS: solid nodule (arrowheads)—minimal vascularity, pattern 0; malignant LN (blank arrowheads)—mixed vascularity; transverse. (dd) Detail of large malignant LN2 (blank arrowheads), size 40 × 27 × 19 mm and volume 11 mL, next left IJV at level C-II: oval shape; homogeneous structure; markedly hypoechoic with transverse fibrous band; transverse. (ee) Detail of large malignant LN2 (blank arrowheads) next left IJV at level C-II, CFDS: increased hilar and central vascularity; transverse. (ff) Detail of large malignant LN2 next left IJV at level C-II: elliptical shape; size 40 × 19 mm, L/S ratio ≈2 (not pathological); homogeneous structure; markedly hypoechoic; next to another two small round hypoechoic ln3, ln4 size of 11 and 12 mm; longitudinal. (gg) Detail of suspicious nodule (arrowheads) in the RL: round shape; inhomogeneous structure; hypoechoic; microlobulated margin; transverse. (hh) Detail of suspicious nodule (arrowheads) in the RL, CFDS: increased hilar end peripheral vascularity, pattern II; transverse. (ii) One year after successful chemotherapy, large hypoechoic thyroid nodules and malignant cervical lymphadenopathy disappeared. US overall view of small multinodular goiter: small, solid, hyperechoic nodules (arrows) in both lobes; size from 5 to 8 mm; Tvol 18 mL, RL 9 mL, and LL 9 mL; transverse. (jj) Detail of the RL: small, solid, hyperechoic nodules (arrows); longitudinal. (kk) Detail of the LL: small, solid, hyperechoic nodules (arrows); longitudinal

Fig. 18.2
(aa) A 58-year-old woman with Hashimoto’s thyroiditis (HT) and a suspicious solitary medium-sized nodule (arrowheads) in the LL, size 23 × 28 × 17 mm and volume 8 mL. Cytology revealed extramedullary plasmacytoma. US overall view: “taller-than-wide” shape; solid; inhomogeneous structure; markedly hypoechoic with hyperechoic fibrous septa; microlobulated margin; thyroid gland with HT—inhomogeneous, sporadically hypoechoic micronodular structure; Tvol 23 mL, RL 9 mL, and LL 14 mL; transverse. (bb) Detail of suspicious medium-sized nodule (arrowheads): inhomogeneous structure; markedly hypoechoic with hyperechoic fibrous septa; microlobulated margin; transverse. (cc) Detail of suspicious medium-sized nodule (arrowheads): inhomogeneous structure; markedly hypoechoic with hyperechoic fibrous septa; microlobulated margin; longitudinal


Fig. 18.3
(aa) A 57-year-old woman with a gastric cancer and metastatic cervical and supraclavicular lymph nodes (LN). US appearance of small Hashimoto’s thyroiditis (HT) with non-suspicious solid nodules (FNAB not performed): inhomogeneous hypoechoic micronodular structure; sporadically small, solid, hyperechoic nodules (arrows); Tvol 7 mL, asymmetry—RL 5 mL and LL 2 mL; transverse. (bb) Detail of RL with HT and nodules: sporadically small, solid, hyperechoic nodules (arrows), size from 5 to 10 mm; longitudinal. (cc) Detail of two metastatic LNs at jugulum at level C-VII: ln1, ln2—elliptical shape; homogeneous structure; hypoechoic; no hilus sign; size 9 × 6 mm and 9 × 7 mm; transverse. (dd) Detail of the five metastatic LNs in left supraclavicular region: ln3–ln6—elliptical or oval shape; homogeneous structure; hypoechoic, no hilus sign; size 9 × 6 mm and 9 × 7 mm; transverse
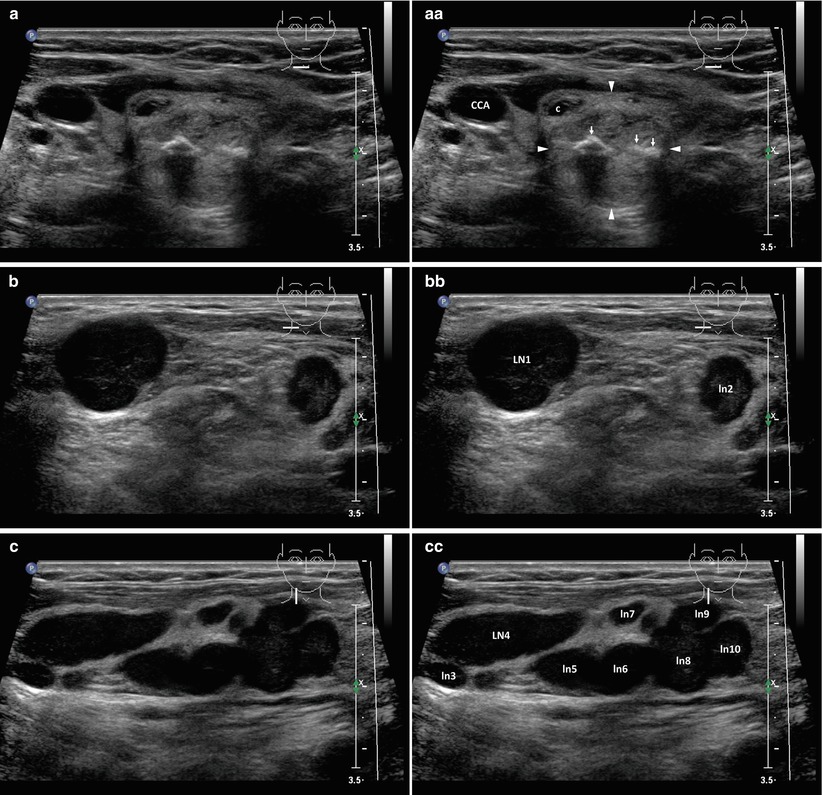
Fig. 18.4
(aa) A 57-year-old woman post right breast mastectomy for cancer and with metastatic lymph nodes (LN) in the right neck region. US finding of solitary non-suspicious complex nodule (arrowheads) with calcifications in the RL, size 17 × 17 × 16 mm and volume 2 mL (FNAB—benign cytology): round shape; coarse structure; hyperechoic; intranodular curvilinear calcifications (arrows) with acoustic shadow; transverse. (bb) Detail of the two metastatic LNs, large LN1 size 22 × 18 × 15 mm and volume 3 mL and small ln2 size 11 × 7 mm at level C-V: oval shape; homogeneous structure; hypoechoic; no hilus sign; transverse. (cc) Detail of cluster of approximately eight metastatic LNs size from 5 mm to 25 mm at level C-II, III, IV: ln3–ln10—elliptical or oval shape; homogeneous structure; hypoechoic, no hilus sign; longitudinal

Fig. 18.5
(aa) A 66-year-old woman after right nephrectomy for cancer and with metastatic lymph nodes (LN) in the left low neck at level C-IV and supraclavicular region. US appearance of small Hashimoto’s thyroiditis (HT) with solitary non-suspicious medium-sized solid nodule (arrowheads) in the LL, size 27 × 16 × 15 mm and volume 3.5 mL (FNAB—benign cytology): round shape; coarse structure; hyperechoic, irregular thin halo sing; RL—structure of atrophic HT; Tvol 11 mL, asymmetry—RL 3 mL and LL 8 mL; transverse. (bb) Detail of solitary medium-sized nodule in the LL and two metastatic LNs next to the left CCA and IJV at level C-IV: solid nodule (arrowheads)—coarse structure; hyperechoic, irregular thin halo sing; metastatic LN1 (blank arrowheads)—round shape, size 16 × 15 mm; metastatic LN2 (marks)—elliptical shape, size 16 × 7 mm; homogeneous structure; slightly hypoechoic; no hilus sign; both LNs compress the left IJV; transverse. (cc) Detail of three metastatic LNs—LN1, LN2 at level C-IV and LN3 at left supraclavicular region: LN1, LN2 next to the left IJV—oval and elliptical shape; LN1 (blank arrowheads) hyperechoic, LN2 (marks) slightly hypoechoic; no hilus sign; small LN3 (marks), size 10 × 7 mm—oval shape; homogeneous structure; hypoechoic; no hilus sign; transverse

Fig. 18.6
(aa) A 63-year-old woman with left bronchial cancer and with metastatic lymph nodes (LN) in the left low neck at level C-IV and supraclavicular region. US finding of solitary non-suspicious small solid nodule (arrow) in the LL, size 12 × 10 × 8 mm and volume 0.5 mL (FNAB—benign cytology): round shape; homogeneous structure; hyperechoic, thin halo sing; Tvol 10 mL, RL 5 mL and LL 5 mL; transverse. (bb) Detail of small metastatic LN, size 9 × 7 × 5 mm, volume 0.2 mL next to the left IJV at level C-IV: ln1 (marks)—oval shape; homogeneous structure; hypoechoic; no hilus sign; transverse. (cc) Detail of small metastatic LN, size 12 × 10 × 6 mm, volume 0.4 mL at left supraclavicular region: ln2 (marks)—elliptical shape; homogeneous structure; hypoechoic; no hilus sign; transverse


Fig. 18.7
(aa) A 35-year-old woman with Hodgkin lymphoma and with malignant lymph nodes (LN) in right and left low neck at level C-IV and supraclavicular regions. US appearance of solitary non-suspicious small solid nodule (arrow) in the RL, size 7 × 6 × 4 mm and volume 0.1 mL (FNAB not performed): ovoid shape; inhomogeneous structure; hyperechoic; sporadic tiny cystic cavities; thin halo sing; Tvol 14 mL, RL 7 mL, and LL 7 mL; transverse. (bb) Detail of two malignant LNs in the right supraclavicular region: elliptical shape, LN1 (marks) size of 18 × 10 mm, L/S ratio > 2 and LN2 (marks) size 21 × 12 mm, L/S ratio > 2 (not pathological); homogeneous structure; hypoechoic; no hilus sign; transverse. (cc) Detail of two malignant LNs in the left supraclavicular region: oval shape, LN3 (marks) size 11 × 10 and LN4 (marks) size 9 × 7 mm; homogeneous; hypoechoic; no hilus sign; transverse. (dd) Detail of another one malignant LN5 (blank arrowheads) deep in the jugulum next to the left CCA at level C-VII: ovoid shape, size 18 × 15 mm; inhomogeneous structure; hypoechoic; no hilus sign; lobulated margin; transverse

Fig. 18.8
(aa) A 64-year-old woman with Non-Hodgkin lymphoma and a large mass palpable for approximately 2 weeks in the right low neck region. Patient’s history: 26 years post total thyroidectomy for multinodular goiter. US appearance of giant malignant lymph node—LN (blank arrowheads), size 69 × 44 × 37 mm and volume 60 mL located in front of the right CCA at C-III, IV level and extends into the right thyroid bed as far as trachea: oval shape; solid; inhomogeneous structure; mostly hypoechoic; no hilus sign; empty left thyroid bed without thyroid remnants; transverse. (bb) Detail of giant malignant LN (blank arrowheads) in front of the right CCA and extending into the right thyroid bed: oval shape; solid; inhomogeneous structure; mostly hypoechoic; no hilus sign; transverse. (cc) Detail of giant malignant LN (blank arrowheads) in front of the right CCA and extending into the right thyroid bed: ovoid shape; solid; inhomogeneous structure; mostly hypoechoic; sporadic fibrous bands; no hilus sign; longitudinal
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree