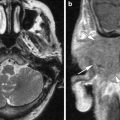
Fig. 1
CT in a patient with coalescent mastoiditis on the right side obviously shows coalescence of the mastoid cells and resorption of the lateral mastoid wall (arrows) (a, c). The contralateral normal ear is shown (b, d)
The sensitivity and accuracy of temporal bone CT findings was evaluated for the diagnosis of acute coalescent mastoiditis, by scoring for mastoid bone integrity on three points, the air cell septae, the sigmoid cortical plate, and the lateral cortical wall. CT turned out to be a valuable technique, and the erosion of the cortical plate that overlies the sigmoid sinus was the most sensitive and specific CT finding for distinguishing coalescent from noncoalescent mastoiditis (Antonelli et al. 1999).
Mastoid subperiosteal abscess develops when the process of coalescence of the mastoid cells leads to a breakthrough of the mastoid cortex and pus collection appears in the postauricular soft tissues. At this moment, clinical examinations and imaging studies, CT as well as MR, become very important, since the difference between the periostitis stage and the abscess stage cannot be deducted from the initial body temperature of the patient, the number of polymorphonuclears, or the CRP values (Francois et al. 2001). Subperiosteal abscess is seen in nearby 50 % of patients diagnosed with coalescent mastoiditis (Spiegel et al. 1998). The destructed lateral cortical otomastoid wall is easily visualized on CT examinations, and the images in soft tissue setting will show the present abscess (Figs. 2 and 3). MRI is able to show the same findings.
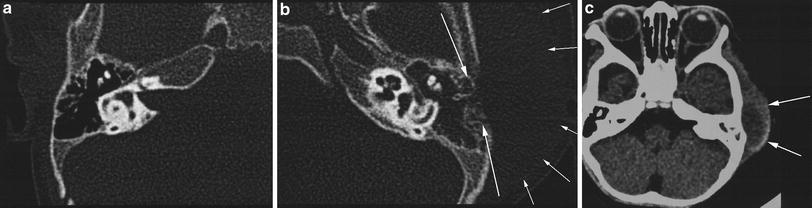

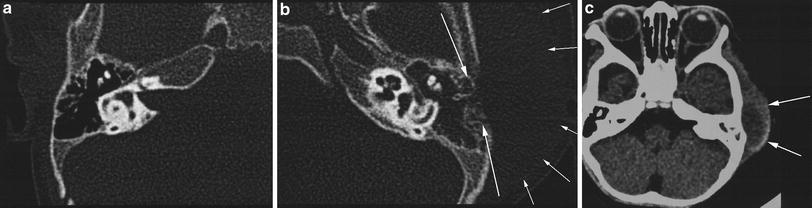
Fig. 2
CT of the normal right temporal bone shows a normal lateral otomastoid cortex (a), while on the contralateral side (b) the lateral cortex of the opacified otomastoid is fragmented (large arrows) and soft tissue swelling is seen (small arrows). This subperiosteal abscess (arrows) is best evaluated on images in soft tissue setting (c)

Fig. 3
In this child with severe fever, this axial CT image in soft tissue setting well-demonstrates the interruption in the lateral cortical wall of the mastoid with subsequent abscess formation
Occasionally, the infection can spread to the temporomandibular joint. When this spread pattern happens to be undertreated severe complications can occur, such as postarthritis ankylosis (Fig. 4).


Fig. 4
In another child with left side soft tissue swelling and subperiosteal abscess formation (a) in combination with coalescent mastoiditis with erosion of the mastoid cortex (b) imaging of the left temporomandibular joint performed 6 months later shows ankylosis as a delayed complication of arthritis (c)
In a retrospective study of 48 children with postauricular swelling and otoscopic signs of acute otitis media, the mastoid pus and the otorrhea were sterile whereas Streptococcus pneumoniae was the most frequent pathogen (Francois et al. 2001). While traditionally in children mastoid subperiosteal abscess required mastoidectomy, the improvement of antibiotic therapy has now changed this approach. It is accepted that uncomplicated acute mastoiditis is treated with myringotomy and intravenous antibiotics (Cohen-Kerem et al. 1999), and that in case of mastoid subperiosteal abscess formation treatment consists of tympanostomy tube insertion, intravenous antibiotics, and postauricular incision with abscess drainage. Such procedure avoids morbidity and complications of mastoid surgery in children (Bauer et al. 2002).
In rare cases, the pus escapades the mastoid near the incisura digastrica and tracks along the digastric and sternocleidomastoid muscles into the neck. Such abscesses are classically referred to as Bezold’s abscess (Spiegel et al. 1998). Reports of Bezold’s abscess in children are rare, since their mastoid pneumatization is not yet completed (Marioni et al. 2001). Most Bezold’s abscesses are seen in adults and are associated with a history of cholesteatoma and mastoidectomy (Castillo et al. 1998).
3 Complications
The clinical course of acute otitis media is often short and the process terminates because of the host’s immune system, the infection-resistant properties of the mucosal linings, and the susceptibility of the major organisms to penicillin. About 1–5 % of untreated or inadequately treated patients may experience complications. Prior to these complications, warning symptoms or signs may be evident: severe earache and/or headache, vertigo, chills and fever, and meningeal symptoms or signs (Dobben et al. 2000).
If complications of inflammatory otomastoid disease are suspected, CT permits accurate diagnosis (Dobben et al. 2000), but MR is the imaging modality of choice (Dobben et al. 2000; Maroldi et al. 2001).
3.1 Otogenic Intracranial Abscess
Increasing temporoparietal headache, near the affected ear, is often the only indication of otogenic brain abscess formation (Dobben et al. 2000). Although rarely seen, among all intracranial complications of middle ear disease, epidural abscess formation is the commonest one (Bizakis et al. 1998). It is most frequently seen as a severe complication of the untreated cholesteatoma, but is also noted in patients suffering from acute mastoiditis. Its therapy depends on the importance of the abscess formation and ranges from high-dosed antibiotics to drainage (Kempf et al. 1998).
MR is the modality of choice to image these abscesses. In view of imaging characteristics, an otogenic intracranial abscess is not different from nonotogenic intracranial abscesses, but its location is typically in the temporal lobe or cerebellum, and the ipsilateral middle ear and mastoid are opacified. The mass generally has a mixed high signal on the T2-weighted images, a mixed low signal on the T1-weighted images and is surrounded by edema. After intravenous injection of gadolinium ring enhancement is seen. Hemorrhage may be present in some parts of the abscess (Fig. 5).
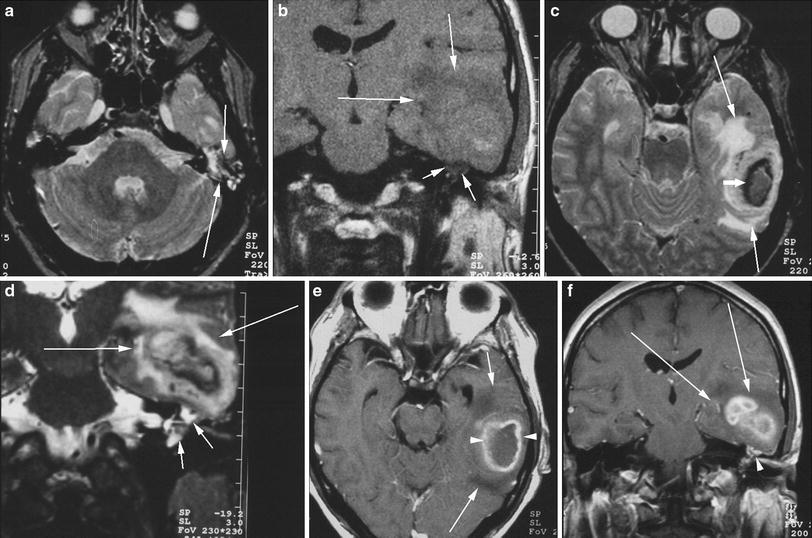
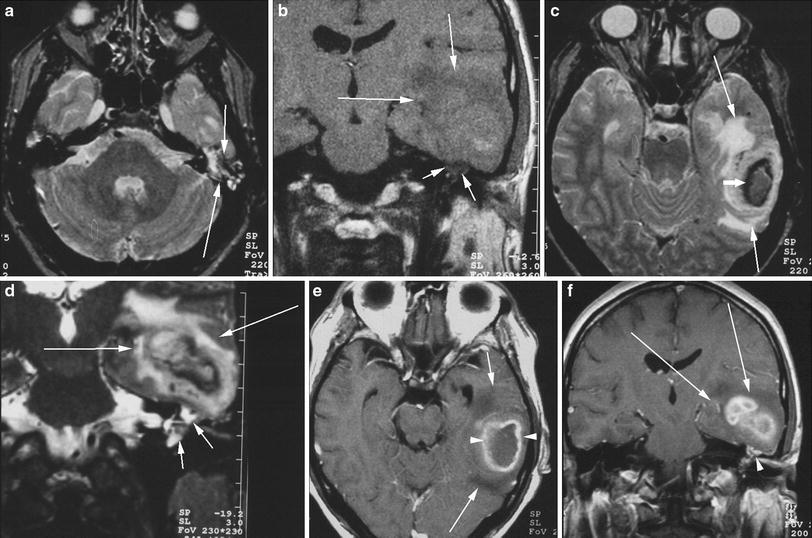
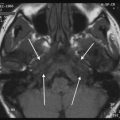
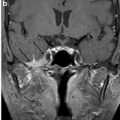
Fig. 5
In this patient with acute otomastoiditis on the left side, the axial T2-weighted image (a) at temporal bone level shows the opacified left otomastoid (arrows). The coronal T1-weighted image before injection of gadolinium (b) shows a large hypointense region (large arrows) in the temporal lobe of the brain, with some hyperintense (hemorrhagic) components, and the opacified otomastoid is also shown (small arrows). On the axial T2-weighted image at temporal lobe level (c) an abscess is visualized (small arrow), surrounded by vasogenic edema (large arrows). The coronal T2-weighted image (d) shows the continuity between the abscess and its surrounding edema on one hand (large arrows) and the inflammatory/infectious otomastoid disease (small arrows) on the other hand. The continuity is realized through an interrupted tegmen tympani. Ring enhancement (small arrow) is demonstrated on the T1-weighted image after intravenous injection of gadolinium (e). The perilesional edema is not enhancing (large arrows). The coronal T1-weighted image after gadolinium injection (f) confirms the findings noted on the coronal T2-weighted image, with the enhancing abscess and the nonenhancing edema (large arrows) in the temporal lobe region, and the enhancing otomastoid disease (small arrows). Note that no linear signal void is present between both enhancing regions, indicating that the normal tegmen tympani is absent
3.2 Sinus Thrombosis
Among all complications of mastoiditis, sigmoid and transverse sinus thrombosis are the least frequent ones (Rocha et al. 2000). It is described to be occasionally complicated by cerebellar venous infarction (Nayak et al. 1994; Ram et al. 2001). Sinus thrombosis is a difficult entity to diagnose. To my personal experience, the disease is easiest to recognize on T1-weighted images before intravenous injection of gadolinium, where the thrombus has an increased signal (Fig. 6). MR angiographic techniques with phase contrast are another valuable alternative.


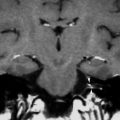
Fig. 6




On the T1-weighted image before gadolinium injection in a patient with right-sided otomastoid opacification (small arrows) a high signal is present in the sigmoid sinus (large arrows) (a) and is also seen in the transverse sinus (arrows) (b). Sigmoid and transverse sinus thrombosis
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree