Fig. 1
Chronic otomastoiditis. On this axial CT scan a small, underdeveloped, poorly pneumatized mastoid is visible (arrows)
Opacification of mastoid air cells and sclerosis of mastoid are typical imaging findings (Fig. 2). Evidence of bone erosion (mastoid septae and rarely, cortex) is characteristic for chronic suppurative otitis media (Veillon 2000; Pandey et al. 2009).


Fig. 2
This axial CT scan shows sclerotic mastoid process with opacified air cells (arrows)
4.2 Tympanic Membrane Changes
Visualization and evaluation of the tympanic membrane is best performed with otoscopy. However, some findings which are typical for chronic inflammation, are well visible with CT and they usually inform the radiologist of some more profound changes within the middle ear and mastoid.
Tympanic membrane thickening and/or perforation is pathognomonic for chronic inflammation. It is evaluated with otoscopic imaging; on CT thickened membrane is visible as grey line of soft tissue density (Fig. 3).
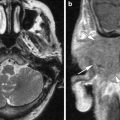
Fig. 3
Axial CT scan of the right middle ear. Thick tympanic membrane (arrow)
Tympanic membrane retraction is the condition, when a part of the tympanic membrane is pulled inwards within the middle ear, usually due to negative pressure in the middle ear. It is also best evaluated with otoscopy. If the retraction is profound, it may become adherent to the stapes head (Fig. 4) (Mafee et al. 1986).
Fig. 4
In this patients axial CT scan of the right ear reveals deep retraction of the thickened and calcified tympanic membrane, which almost touches stapes head
The term Myringosclerosis stands for the formation of the hyalinized collagen in the tympanic membrane. In most cases changes are clinically significant and cause little or no hearing loss. On CT myringosclerosis is visible as thickened and calcified (Fig. 5) tympanic membrane (Lemmerling et al. 2009).
Fig. 5
In this patient a thick calcified plaque is visible in the tympanic membrane (arrow). This finding is typical for myringosclerosis
4.3 Ossicular Chain Fixation
Post-inflammatory ossicular chain fixation (PIOF) is a common problem in patients with COM and in many cases it results with conductive hearing loss. It usually takes three pathologic forms (Swartz et al. 1985, Lemmerling et al. 2008, 2009):
presence of fibrous tissue (chronic adhesive otitis media)
hyalinization of collagen (tympanosclerosis)
new bone formation (fibro-osseous sclerosis).
Fibrous tissue fixation appears on CT as noncalcified, soft-tissue debris encasing some or all of the ossicular chain. It is usually present in the niche of oval window, forming so called “peristapedial tent” (Fig. 6), but may also be present anywhere in meso- and epitympanum. On CT it is usually presented as a subtle mass of soft tissue density. Therefore, diagnosis of fibrous tissue fixation based on sole CT appearance should not be made, since fixation cannot be determined by imaging and the density of the mass is similar to other middle ear substances, like fluid and cholesteatoma. Diagnosis of fibrous tissue fixation can be suggested, if a soft tissue mass is seen in the setting of COM, in patient with dry ear and conductive hearing loss (Swartz et al. 1985).


Fig. 6
Chronic otomastoiditis with ossicular chain fixation. On this axial CT scan a soft tissue-density mass is found around stapes, forming peri-stapedial tent
Tympanosclerosis reflects deposits of hyalinized collagen in the tympanic cavity. It appears as unifocal or multifocal punctate or weblike calcifications in the middle ear cavity (Fig. 7) or on the tympanic membrane (myringosclerosis). In the tympanic cavity, it may be present in any location, visible as focal calcified densities in the middle ear cavity, along tendons, also in direct apposition to the ossicular chain. If the debris is not in a position to compromise the ossicular chain function, conductive hearing loss will not take place. On CT changes may be subtle—increased thickening of stapedial crura—or more profound (Swartz et al. 1985; Lemmerling et al. 2009). Since calcification of tendons and ligaments is a characteristic for tympanosclerosis, knowledge of normal anatomy and anatomical variants is mandatory in order to evaluate the exact location and extent of the disease. Normal eminences, prominent bone ridges, and tendons should not be mistaken for pathological changes (Lemmerling et al. 1997; Petrus 1997).


Fig. 7
This CT scan shows tympanosclerosis as post-inflammatory calcifications within epitympanum (arrows) in patient with chronic otitis media and hearing loss
New bone formation has been identified mostly in the epitympanum and is the least common manifestation of PIOF. It is visible as lamellar structures of high density (Fig. 8), thick bony webs, or generalized bony encasement (Lemmerling et al. 2008).
Fig. 8
This coronal temporal bone CT scan reveals large dense bone deposit (arrow) within epitympanum. This type of tympanosclerosis is referred to as new bone formation
In general, CT of the temporal bone plays an important role in the evaluation of the extent of PIOF. It also enables differential diagnosis which includes other causes of conductive hearing loss, like otosclerosis, ossicular chain erosion, post-traumatic changes, developmental abnormalities. In case of suspected cholesteatoma MRI is the modality of choice (De Foer et al. 2007; Lemmerling et al. 2009).
4.4 Ossicular Chain and Tympanic Cavity Erosion
Post-inflammatory ossicular chain erosion is not very frequent in case of a non-cholesteatomatous disease, but does occur, and will affect first the incus long process and lenticular process, followed by stapes head.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree