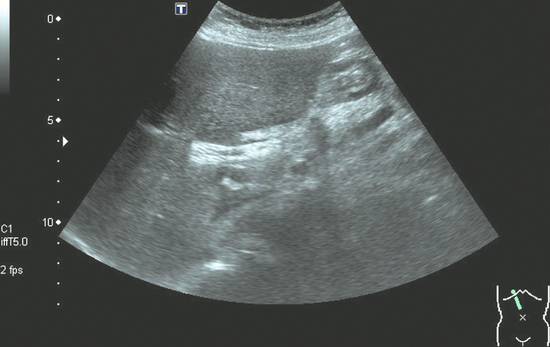
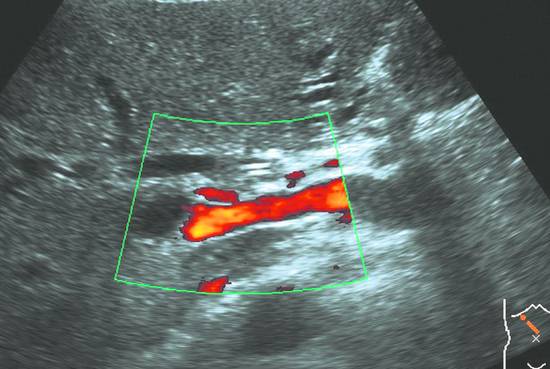
Palliative Interventions and the Role of Ultrasonography in Palliative Care Palliative care is playing an increasingly important role in contemporary medicine. Given the fact that many cancers and other diseases are incurable or only partially curable, great importance is attached to the amelioration of suffering. The goal of palliative care is not to cure a disease or combat its causes but to relieve its symptoms. In the truest sense of the word, then, palliative care should wrap a “protective cloak” (Latin pallium = cloak or cover) around patients to provide comfort, to shield them from inappropriate procedures, and especially to relieve pain. In this sense, palliation includes all actions (medical, nursing, social, psychological) involved in the management of incurable diseases that shorten life expectancy. It is particularly important to relieve distressing physical symptoms such as pain, dyspnea, and eating difficulties. In some cases the requirements for symptom abatement must remain modest.1–3 The main goals of palliative care are to: Prolong life Manage symptoms Address spiritual and psychosocial needs Provide palliative nursing care On the basis of the WHO definition of 2002,4 this concept has been expanded to include: Greater emphasis on the patient’s quality of life The earlier initiation of the palliative care, which is started concurrently with therapies aimed at prolonging life What is the specific role of ultrasonography in the palliative care setting (“palliative ultrasound”)?5 Ultrasound is a valuable diagnostic tool in the detection of palliative conditions (palliative staging). Ultrasound is a relatively low-cost means of monitoring palliative care patients and identifying situations that require palliative intervention. A number of palliative interventions can be performed under ultrasound guidance. These interventions can be performed not only as inpatient procedures but also in outpatient settings and at home. Finally, ultrasound examinations can provide care and comfort for palliative patients until the end of life. The natural history of cancer is marked by a progression of typical stages. Ultrasound plays a major role in diagnosis, staging, and treatment monitoring and is the only follow-up imaging study that conforms to consensus guidelines for all tumor entities.6 A large percentage of oncologic diseases are incurable, however. The patient eventually enters a stage in which the disease (e.g., pancreatic cancer) is no longer curable and palliative treatment options become a priority concern.7 Except in cases of colorectal cancer, the detection of hepatic metastases means that the disease has reached a palliative stage. Ultrasound has high sensitivity (>90%) in the detection of these lesions. It is considerably less sensitive in the detection of peritoneal carcinomatosis (approximately 50–60%). Ultrasound in a palliative treatment setting is useful for evaluating clinical progression and can accurately assess therapeutic response based on criteria such as the size of hepatic metastases or peritoneal fluid volume. Thus, ultrasound can contribute significantly to making the prognostic assessment that is so important for patients and their families. In cases where the primary intent of care is palliative, ultrasound should be used in subsequent follow-up examinations whenever possible, one goal being to economize on resources. One important goal of palliative staging is to spare the patient an unnecessary intervention, operation, or chemotherapy by demonstrating that the procedure will not benefit the patient and will only cause adverse side effects and raise false hopes. In cases where primary cancer treatment has been successful, the patient is placed on oncologic follow-up. The goal of this follow-up is to achieve long-term remission through: The early detection and curative treatment of metastasis The detection and curative treatment of recurrent disease Imaging follow-ups have these additional goals: The detection of a possible second tumor The evaluation of treatment response Today, of course, general follow-up care is considered to have a more comprehensive scope in line with the principles of “caring medicine.” But ultrasound follow-ups in the narrow sense are concerned mainly with the detection of hepatic metastases. What benefit does this hold for the affected patient? Strictly speaking, a benefit exists only if surgical resection of the metastases is still technically possible and would also provide a survival benefit for the patient (▶ Table 33.1). When a disease is diagnosed as incurable during primary staging or later in its course, ultrasound also has a special role in palliative treatment monitoring. For many interventions ultrasound is a noninvasive, universally available, and cost-effective procedure that is ideal for monitoring and documenting response to palliative therapy. Classic examples of palliative treatment monitoring are stent evaluation in patients with a malignant biliary obstruction, the assessment of ascites in peritoneal carcinomatosis, and evaluating pancreatic tumor response to chemotherapy. The guideline for palliative chemotherapy states that upper abdominal ultrasound is the modality of choice for evaluating tumor response during the course of palliative chemotherapy (▶ Fig. 33.1, ▶ Fig. 33.2 and ▶ Table 33.2).7 Fig. 33.1 Biliary stent monitoring. Ultrasound after metal stent placement in a patient with bile duct cancer excludes further obstruction of the proximal biliary tract. (Source: image courtesy of Dr. Albrecht Holle, University of Rostock, Germany.) Fig. 33.2 Follow-up image after stenting and during palliative chemotherapy in a patient with pancreatic cancer.
33.1 Content and Goals of Palliative Care
33.2 Ultrasound in Palliative Staging, Follow-Up, and Palliative Treatment Monitoring
Benefit has been documented for the detection or resection of hepatic metastases
Benefit has not been documented for the detection or resection of hepatic metastases
Colorectal cancer +
Stomach −
Lung − (+)
Breast −
NET (neuroendocrine tumor) (+)
Pancreas −
Lymphoma +
Bile ducts −
Kidney −
Diagnostic/therapeutic
Procedure
Indications, goals, comments
Chapter
Diagnostic
FNA pancreatic cancera
Confirm diagnosis before palliative chemotherapy
12
FNA HCC
HCC (>5 cm) before TACE or chemotherapy; HCC (<5 cm) before HiTT or PEIT
12, 18, 19
FNA hepatic metastasis
Before ablative treatment (HiTT), before palliative chemotherapy
12, 18, 19
FNA ascites
Before palliative chemotherapy or local treatment
13, 22
FNA pleural effusion
Before palliative chemotherapy or pleurodesis
12, 24
FNA lung cancera
Before chemoradiation
12, 24
Therapeutic
PTCDa
Palliative biliary tract decompression in patients with bile duct carcinoma, liver cancer, or pancreatic cancer
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree

 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access