Pancreas, Spleen, and Bowel
QUESTIONS
A. Reverberation artifact
B. Ring-down artifact
C. Comet-tail artifact
D. Twinkle artifact
View Answer
1 Answer B. Image of the right upper quadrant shows ring-down artifact arising from a gas-filled loop of bowel.
In ring-down artifact, the transmitted ultrasound energy causes resonant vibrations within fluid trapped between multiple gas bubbles. These vibrations create a continuous sound wave that is transmitted back to the transducer. This phenomenon is displayed as a line or series of parallel bands extending posterior to a gas collection. Ring-down artifact occurs most frequently because of gas and has also been shown with metal.
Reverberation artifacts (answer choice A) occur when the ultrasound signal reflects repeatedly between highly reflective interfaces that are usually in the near field. This is seen as multiple equidistantly spaced linear reflections. Comettail artifact (answer choice C) is a form of reverberation. In this artifact, the two reflective interfaces and their sequential echoes are closely spaced. The later echoes have decreased amplitude resulting in a reverberation artifact with a triangular, tapered shape. Twinkle artifact (answer choice D) is due to a form of intrinsic noise within the Doppler circuitry of the US machine and is commonly observed at color Doppler imaging when insonating certain rough reflective surfaces.
References: Dillman JR, Kappil M, Weadock WJ, et al. Sonographic twinkling artifact for renal calculus detection: correlation with CT. Radiology 2011;259:911-916.
Feldman MK, Katyal S, Blackwood MS. US artifacts. RadioGraphics 2009;29:1179-1189 Hertzberg BS, Middleton WD. Ultrasound: the requisites, 3rd ed. Philadelphia, PA: Elsevier, 2016:23.
2 Which of the following has the highest acoustic impedance?
A. Air
B. Fat
C. Muscle
D. Bone
View Answer
2 Answer D. Acoustic impedance of a material is defined as the product of the density of the medium and the speed of sound in that medium. It is a measure of the stiffness of a tissue. In the provided choices, acoustic impedance is lowest in air, followed by fat, muscle, and bone. Bone and metal have high acoustic impedance.
Reference: RSNA. RSNA/AAPM radiology physics educational modules.
3 Fresnel zone is:
A. The far field of the ultrasound beam
B. The near field of the ultrasound beam
C. Another name for side lobes
D. Another name for grating lobes
View Answer
3 Answer B. Fresnel zone is the near field of the ultrasound beam. It is near the transducer face and has a converging beam profile. The far field or diverging field of the ultrasound beam is called the Fraunhofer zone. Ultrasound imaging normally uses the Fresnel zone.
The length of the Fresnel zone is d2/44, where d is the diameter of the transducer and λ is the wavelength. Therefore, Fresnel zone increases with increasing transducer size and frequency (i.e., lower wavelength).
Reference: Bushberg JT, Seibert JA, Leidholdt EM. The essential physics of medical imaging, 3rd ed. Philadelphia, PA: Wolters Kluwer Health/Lippincott Williams & Wilkins, 2011:520-521.
4 Which maneuver should you attempt first to improve visualization of the pancreas in the image shown?
|
A. Set the focal zone deeper.
B. Reduce frequency.
C. Increase gain.
D. Decrease depth.
E. Reduce spatial compounding.
View Answer
4 Answer D. In this image, the structures we are interested in evaluating are displayed in the top half of the image, whereas the bottom half shows information that is not useful or diagnostic. Decreasing depth would eliminate the nondiagnostic information and allow us to evaluate the pancreas at an increased frame rate.
The focal zone (answer choice A) should be set at or just below the structure of interest. In this case, the focal zone (indicated by triangle on left side of image) is set appropriately, just below the pancreas. Lowering frequency (answer choice B) allows for increased penetration at the expense of decreased resolution. In this case, the pancreas is in the near field, and thus, we do not need to increase our penetration to evaluate it. Increasing gain (answer choice C) will amplify the ultrasound signal causing the image to have an overall brighter or more saturated look. Gain is set appropriately in this image. Spatial compounding (answer choice E) reduces speckle and noise. Reducing the number of lines of spatial compounding will cause the image to appear noisier. Increasing spatial compounding may reduce diagnostically helpful artifacts such as acoustic shadow.
Reference: Hangiandreou NJ. AAPM/RSNA physics tutorial for residents: topics in US. RadioGraphics 2003;23(4):1019-1033.
5 A 29-year-old female patient presents with Crohn disease and right-sided abdominal pain. Two US images obtained in the right abdomen are shown. What is the most likely diagnosis?
|
A. Acute appendicitis
B. Terminal ileitis
C. Intussusception
D. Incarcerated inguinal hernia
View Answer
5 Answer A. A blind-ending structure representing the appendix contains an echogenic shadowing appendicolith. The appendix is thickened at 9 mm. Other images on the study (not shown) demonstrated the appendix to be noncompressible with fluid adjacent to its tip. Findings are diagnostic of acute appendicitis. Sonographic evaluation of suspected acute appendicitis relies on the use of a high-resolution, usually linear probe and graded compression to optimize appendiceal visualization. The primary diagnostic criterion is a thickened appendix >6 mm in diameter. Other signs of acute appendicitis include lack of compressibility, echogenic inflamed periappendiceal fat, hyperemia, appendicolith, and periappendiceal fluid. Terminal ileitis can exhibit similar features, so careful assessment for a blind-ending morphology is important to avoid this pitfall.
References: Birnbaum BA, Wilson SR. Appendicitis at the millennium. Radiology 2000;215(2):337-348.
Hertzberg BS, Middleton WD. Ultrasound: the requisites, 3rd ed. Philadelphia, PA: Elsevier, 2016:208-209.
6 Which of the following will improve axial resolution in an ultrasound image?
A. Increasing transducer frequency
B. Decreasing transducer frequency
C. Increasing the diameter of ultrasound beam
D. Decreasing the diameter of ultrasound beam
View Answer
6 Answer A. Axial resolution is the ability to separate two closely spaced objects in the direction of the ultrasound beam. To avoid overlap of returning echoes, the distance between the two objects must be at least one-half of the spatial pulse length. Spatial pulse length (SPL) is the number of cycles emitted per pulse by the transducer multiplied by the wavelength. Decreasing the spatial pulse length will improve the axial resolution. This can be achieved by using a higher frequency, which will reduce the wavelength and hence the spatial pulse length. The tradeoff is decreased tissue penetration.
Decreasing the diameter of ultrasound beam improves the lateral resolution, which is the ability to separate two closely placed objects perpendicular to the ultrasound beam direction. The lateral resolution is best at the near field-far field interface where the effective beam diameter is approximately equal to half the transducer diameter.
Reference: Bushberg JT, Seibert JA, Leidholdt EM. The essential physics of medical imaging, 3rd ed. Philadelphia, PA: Wolters Kluwer Health/Lippincott Williams & Wilkins, 2011:561-562.
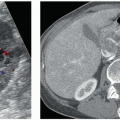
7a A 79-year-old male presents to the emergency department with painless jaundice. Which of the following structures are abnormal?
|
A. Pancreatic duct and common duct
B. Common duct and main portal vein
C. Main portal vein and splenic vein
D. Splenic vein and pancreatic duct
View Answer
7a Answer A. The images show both a dilated pancreatic duct and a dilated common bile duct, with a heterogeneous mass located in the pancreatic head. This imaging appearance is known as the “double-duct” sign, which is considered a hallmark for pancreatic head cancer. The dilated pancreatic duct should not be mistaken for the splenic vein, which is located posterior to the pancreas. Also, a dilated common duct (CD) could be confused for a vascular structure. However, the location of the CD to the left of the portal vein on the transverse image should indicate which anechoic structure is the portal vein and which is the CD. Colorflow imaging should help confirm the identity of the CD.
Reference: Hertzberg BS, Middleton WD. Ultrasound: the requisites, 3rd ed. Philadelphia, PA: Elsevier, 2016:185-186.
|
7b Which of the following is the most common sonographic appearance of the lesion shown?
A. Hyperechoic and hypervascular
B. Hyperechoic and hypovascular
C. Hypoechoic and hypervascular
D. Hypoechoic and hypovascular
View Answer
7b Answer D. Majority of pancreatic cancers appear hypoechoic on ultrasound compared to the surrounding pancreatic parenchyma. Pancreatic cancer is a hypovascular tumor. It can cause considerable desmoplastic reaction resulting in obstruction and dilatation of the pancreatic duct and common bile duct. Therefore, tumors in the pancreatic head are usually detected when they are small because of early biliary tract obstruction and jaundice compared to those in the body and tail, which tend to present as larger masses and with vague symptoms. Approximately 60% to 70% pancreatic cancers arise in the head, 10% to 20% in the body, and 5% to 10% in the tail.
Reference: Hertzberg BS, Middleton WD. Ultrasound: the requisites, 3rd ed. Philadelphia, PA: Elsevier, 2016:185-186.
8 What is the purpose of using gel between the transducer and skin surface?
A. To displace air
B. To decrease friction
C. To improve glide
D. To improve patient compliance
View Answer
8 Answer A. Reflection of ultrasound energy at a boundary between two tissues occurs because of the differences in acoustic impedances of the two tissues. Air-tissue interfaces reflect almost all of the incident ultrasound beam because of large differences in acoustic impedance between those two media. Therefore, gel is applied between the transducer and skin surface to displace air and therefore minimize differences in acoustic impedance.
Reference: RSNA. RSNA/AAPM radiology physics educational modules.
9 Plan-Do-Study-Act is a commonly used methodology for which of the following goals?
A. Quality control
B. High-reliability organization
C. Quality improvement
D. Patient confidentiality
View Answer
9 Answer C. The Plan-Do-Study-Act (PDSA) is an iterative four-step process used for quality improvement. In this process, a specific perceived practice deficiency is identified and an appropriate measurement is devised to assess the selected issue during the planning phase. A predicted result and desired performance target are also determined. Next, during the Do phase, baseline measurements are collected. Once an appropriate number of samples is collected, the data are studied and compared with the anticipated result and target. If the measured performance does not meet the target, potential root causes and other factors are examined. If the measured performance does meet the target, a plan to sustain the performance goal is instituted. During the Act phase, a plan for improvement is devised and implemented based on the root causes and factors identified during the Study phase. The PDSA cycle is then repeated continuously until the goal is achieved, or may be intermittently used to confirm that a performance goal is being maintained.
Reference: The American Board of Radiology. Quality and safety domain specification and resource guide. Tucson, AZ: The American Board of Radiology, 2016.
10 Compared to holding the transducer at an oblique angle to a tissue interface, perpendicular orientation to the interface will:
A. Return more of the echo to the probe
B. Result in mislocalization of lesions because of refractive artifact
C. Diminish penetration of deeper tissues
D. Increase the likelihood of duplication artifacts
View Answer
10 Answer A. Because the angle of incidence and angle of reflection of sound are the same but in opposite directions, a greater proportion of the reflected sound will be directed toward the probe when the transducer is held perpendicular to a tissue boundary. Increasing the angle of the probe will eventually result in all of the reflected energy to be directed completely away from the probe so that the echo will not be detected at all.
Refraction occurs when the beam propagates obliquely through tissue boundaries through which the speed of sound changes. This will result in mislocalization and sometimes artifactual duplication of anatomic structures. Refraction also results in defocusing and weakening of the ultrasound beam, compromising penetration and visualization of deeper tissues.
Reference: Hertzberg BS, Middleton WD. Ultrasound: the requisites, 3rd ed. Philadelphia, PA: Elsevier, 2016:22.
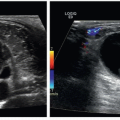
11 These are the ultrasound images from the left mid abdomen of a 70-year-old male with a history of non-Hodgkin lymphoma being evaluated for melena. What is the name of the sign that describes the ultrasound findings?
|
A. WES (wall-echo shadow) sign
B. Pseudokidney sign
C. Yin-yang sign
D. Onion skin sign
View Answer
11 Answer B. Lymphomatous involvement of the colon in this patient results in a typical sonographic appearance due to tumor infiltration—hypoechoic, concentric, long-segment bowel wall thickening with destruction of the wall layers and a central echogenic area with dirty shadowing corresponding to air-filled residual lumen. The peripheral hypoechoic thickened wall simulates renal cortex, and central echogenic area simulates renal sinus fat; hence the name.
Wall-echo shadow (WES) sign is described for cholelithiasis. Yin-yang sign is a color Doppler sign of pseudoaneurysm. Onion skin sign has been described for testicular epidermoid and mucocele of appendix.
References: Hertzberg BS, Middleton WD. Ultrasound: the requisites, 3rd ed. Philadelphia, PA: Elsevier, 2016:204, 206.
Ledermann HP, Börner N, Strunk H, et al. Bowel wall thickening on transabdominal sonography. AJR Am J Roentgenol 2000;174(1):107-115.
Rumack CM, Wilson SR, Charboneau WJ. Diagnostic ultrasound, 4th ed. Philadelphia, PA: Elsevier Health Sciences, 2011:270-280.
12 A 70-year-old male with anemia and splenomegaly on physical examination undergoes a left upper quadrant ultrasound. Based on the imaging findings, what is the most likely diagnosis?
|
A. Splenic infarcts
B. Leukemia
C. Lymphangiomas
D. Hemangiomas
View Answer
12 Answer B. The normal spleen has a homogeneous echotexture and is hyperechoic compared to the liver and kidney. It measures up to 13 cm in length and normally has a crescentic configuration. This patient has an enlarged spleen that contains multiple solid hypoechoic lesions. Lymphangiomas are composed of multiple variably sized cystic spaces and are either anechoic or hyperechoic depending on the cyst size. Hemangiomas are typically hyperechoic. Splenic infarcts may be hypoechoic but are expected to be wedge shaped and peripherally located. In an older patient with splenomegaly and multiple hypoechoic solid splenic lesions, a lymphoproliferative process must be considered. This patient was diagnosed with chronic lymphocytic leukemia with leukemic splenic infiltration. The differential diagnosis for solid hypoechoic splenic lesions is fairly extensive and includes lymphoma, metastases, infarcts, abscesses, and sarcoidosis.
Reference: Hertzberg BS, Middleton WD. Ultrasound: the requisites, 3rd ed. Philadelphia, PA: Elsevier, 2016:192-203.
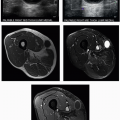
13a A 55-year-old male presents with intractable chronic abdominal pain. What is the most likely etiology for the condition shown in the ultrasound image?
|
A. Alcohol
B. Gallstones
C. Idiopathic
D. Heredity
View Answer
13a Answer A. The ultrasound image shows heterogeneous pancreatic parenchyma with multiple echogenic foci consistent with calcifications. The calcifications may or may not shadow depending on their size. The imaging appearance is typical of chronic pancreatitis.
Chronic pancreatitis is an inflammatory disease process that leads to progressive and irreversible structural damage of the pancreas resulting in permanent dysfunction of both endocrine and exocrine pancreatic function. Histologic changes include acinar cell loss, islet cell loss, inflammatory cell infiltrates, and eventually irregular fibrosis. Patients present with abdominal pain, malabsorption, and diabetes.
Alcohol abuse is the most common cause of chronic pancreatitis in Western countries, accounting for 70% to 90% of cases (choice A is correct). Other etiologies include genetic (mutations in the cystic fibrosis gene, hereditary pancreatitis), ductal obstruction (e.g., trauma, pseudocysts, stones, tumors, pancreas divisum), tropical pancreatitis, systemic disease such as systemic lupus erythematosus, hypertriglyceridemia, autoimmune pancreatitis, and idiopathic pancreatitis.
The classic sonographic sign of chronic pancreatitis is pancreatic calcifications. The intraductal location of the calcifications may not be obvious on ultrasound, where they may seem scattered throughout the pancreatic parenchyma as in this case. Other sonographic findings include duct dilatation, pancreatic atrophy, irregular contours, and hyperechoic parenchyma due to fatty deposition and fibrosis.
References: Perez-Johnston R, Sainani NI, Sahani DV. Imaging of chronic pancreatitis (including groove and autoimmune pancreatitis). Radiol Clin North Am 2012;50(3):447-466.
Zamboni GA, Ambrosetti MC, D’Onofrio M, et al. Ultrasonography of the pancreas. Radiol Clin North Am 2012;50(3):395-406.
13b Aspiration of the lesion shown here in the same patient is likely to reveal elevated levels of which of the following?
|
A. Carcinoembryonic antigen (CEA)
B. Amylase
C. Lipase
D. Mucin
View Answer
13b Answer B. The ultrasound image shows a large anechoic cystic lesion adjacent to the head of the pancreas. Multiple echogenic calcifications are again shown in the pancreas. In this setting, the lesion most likely represents a pancreatic pseudocyst.
In a pseudocyst, intracystic fluid will be expected to have a high amylase level and a low CEA and CA 19-9 level. High amylase levels can also be seen in IPMNs. CEA and CA 19-9 are also low in pancreatic serous tumors. High CEA levels are seen in mucinous cystic neoplasms.
Reference: Al-Hawary MM, Francis IR, Anderson MA. Pancreatic solid and cystic neoplasms. Radiol Clin North Am 2015;53(5):1037-1048.
14 What is the best definition of “value” in health care?
A. Reduce cost of providing health care.
B. Increase quality of health care.
C. Provide a desired level of quality at low cost.
D. Provide care for more individuals.
View Answer
14 Answer C. Two important components of value in health care are quality and cost. Value is the efficient (low cost) use of resources, which yields a desired level of quality.
Reference: The American Board of Radiology. Quality and safety domain specification and resource guide. Tucson, AZ: The American Board of Radiology, 2016.
15 A 25-year-old male presents with left upper quadrant pain. What is the most appropriate step for further management?
|
A. Surgery or percutaneous drainage
B. Anticoagulation
C. Supportive management
D. CT or MRI
View Answer
15 Answer C. A wedge-shaped peripheral hypoechoic splenic lesion with a coarsened echotexture with its apex pointing to the hilum represents an acute splenic infarct. The diagnosis of splenic infarction can be made with a high degree of confidence because of its characteristic shape, location, and coarse echotexture. Splenic infarcts are a common cause of focal splenic lesions seen on imaging. The most common etiologies include emboli or thrombosis of the splenic artery, splenic vein, or their branches. Other etiologies include lymphoproliferative disorders and sickle cell anemia. Infarcts usually become smaller and hyperechoic with time as the devitalized tissue is replaced by scar and will be accompanied by overlying capsular retraction. However, the sonographic appearance of splenic infarcts can vary and appear as mass-like or nodular foci, requiring additional imaging with CT or MRI. Although a workup to determine the etiology of splenic infarction is important, acute uncomplicated splenic infarcts usually require only supportive therapy. Potential complications include abscess, pseudocyst formation, rupture, and hemorrhage.
References: Goerg C, Schwerk WB. Splenic infarction: sonographic patterns, diagnosis, follow-up, and complications. Radiology 1990;174(3):803-807.
Hertzberg BS, Middleton WD. Ultrasound: the requisites, 3rd ed. Philadelphia, PA: Elsevier, 2016:198-201.
Rumack CM, Wilson SR, Charboneau WJ. Diagnostic ultrasound, 4th ed., 2 volume set. Philadelphia, PA: Elsevier Health Sciences, 2011:163.
16a A 20-year-old female presents with left upper quadrant pain following blunt abdominal injury. What is the most likely diagnosis?
|
A. Splenic laceration
B. Subcapsular hematoma
C. Splenic infarct
D. Splenic pseudoaneurysm
View Answer
16a Answer A. An elongated hypoechoic focus within the splenic parenchyma contains no color flow and represents a splenic laceration. No subcapsular or perisplenic collection is shown. The most commonly injured intra-abdominal organ following blunt trauma is the spleen. Splenic injuries range from contusion to shattered spleen. Treatment decisions are based on clinical and hemodynamic parameters and may include conservative management, embolization, and surgery. Although subcapsular hematomas are also contained within the splenic capsule, they should be located along the periphery of the spleen, follow the splenic contour, and typically have a crescentic shape. Splenic infarcts and lacerations may be sometimes difficult to distinguish by imaging, but the clinical history should permit differentiation. The sensitivity of ultrasound for the detection of pseudoaneurysms is inferior to CT, but a sonographic diagnosis requires demonstration of internal flow.
16b What is the next step in management for this patient?
A. Coil embolization
B. Splenectomy
C. Contrast-enhanced CT
D. Follow-up imaging surveillance
View Answer




16b Answer C. Although splenic injuries can be demonstrated by ultrasound, CT provides a more comprehensive evaluation for splenic injuries and perisplenic hematomas as well as assessment for other intra-abdominal organs and vessels.
Reference: Rumack CM, Wilson SR, Charboneau WJ. Diagnostic ultrasound, 4th ed. Philadelphia, PA: Elsevier Health Sciences, 2011:165-167.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree