Part 6 Gastrointestinal
Case 60

Clinical History
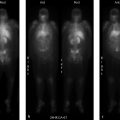
88-year-old female with nausea after meals referred for gastric emptying study (▶Fig. 60.1).
Key Finding
Esophageal activity seen on gastric emptying study
Top 2 Differential Diagnoses
Gastroesophageal reflux disease. Scintigraphic gastric emptying studies are frequently performed for the evaluation of gastroparesis, and remain the gold standard. While much of the overall impression of a gastric emptying study is derived from the quantitative data, with well-defined normal limits of emptying at predetermined time points, it is very important to analyze the source images when interpreting the exam to ensure that the quantitative data is reliable, and also to evaluate for any other possibly clinically relevant findings. One such finding somewhat commonly seen is esophageal activity. Seeing activity in the esophagus, particularly if only seen on the more delayed images, is pathognomonic for gastroesophageal reflux disease (GERD). This is important to note as GERD may actually be responsible for the symptoms leading to the clinical concern for gastroparesis. Furthermore, there appears to be somewhat of a relationship between gastroparesis and GERD. It is thought that a delay in gastric emptying can either cause or exacerbate GERD. Delayed emptying can lead to distension and increased pressure in the gastric cardia which may shorten the lower esophageal sphincter, making it less effective. Prolonged gastric retention also gives gastric contents more time to reflux, increases gastric acid production, and can lead to higher volume reflux. Delayed gastric emptying has been found in up to one-third of adult patients with GERD. Although scintigraphy is not primarily performed for evaluation of GERD in the adult population, it is useful in the evaluation of suspected GERD in an infant. This does not include a standard gastric emptying evaluation, but instead is performed with a dedicated protocol usually involving 60-minute dynamic imaging of a supine infant after administration of Tc-99m radiolabeled milk or formula. It is a highly sensitive study that uses a normal, physiologic meal and does not require abdominal compression. If GERD is seen, either in an adult or pediatric patient, 24-hour images can be obtained to evaluate for pulmonary activity due to aspiration.
Esophageal retention. Esophageal activity seen on a gastric emptying study may represent radiotracer that never made it into the stomach. If this is the case, activity should be seen in the esophagus on the initial image obtained immediately after oral intake of the radiolabeled meal and should decrease, not increase, on subsequent images.
Diagnosis
Early esophageal retention with subsequent gastroesophageal reflux.
✓ Pearls
Images from gastric emptying studies should be evaluated for evidence of gastroesophageal reflux.
Up to one-third of adults with GERD have been found to have delayed gastric emptying.
Delayed gastric emptying can both cause and exacerbate GERD.
Scintigraphy is useful for the evaluation of an infant with suspected GERD.
Suggested Readings
Abell TL, Camilleri M, Donohoe K, et al. American Neurogastroenterology and Motility Society and the Society of Nuclear Medicine. Consensus recommendations for gastric emptying scintigraphy: a joint report of the American Neurogastroenterology and Motility Society and the Society of Nuclear Medicine. J Nucl Med Technol. 2008; 36(1):44–54 Elbl B, Birkenfeld B, Walecka A, et al. Upper gastrointestinal tract scintigraphy and ultrasonography in diagnosis of gastroesophageal reflux in children. Pol J Radiol. 2011; 76(1):63–67 Fass R, McCallum RW, Parkman HP. Treatment challenges in the management of gastroparesis-related GERD. Gastroenterol Hepatol (N Y). 2009; 5(10, Suppl 18): 4–16 Mariani G, Boni G, Barreca M, et al. Radionuclide gastroesophageal motor studies. J Nucl Med. 2004; 45(6):1004–1028Case 61

Key Finding
Delayed solid meal gastric emptying
Top 3 Differential Diagnoses
Diabetic gastroenteropathy. Gastroparesis, or delayed gastric emptying in the absence of mechanical obstruction, is most commonly caused by diabetes mellitus (DM). It affects approximately 5% of those with type 1 DM and 1% of those with type 2 DM. Diabetic gastroenteropathy is presumed secondary to autonomic neuropathy involving the stomach and is typically seen in the setting of other diabetic complications including retinopathy, nephropathy, and peripheral neuropathy. The hyperglycemia seen in DM also suppresses gastric motility and delays gastric emptying. In fact, rapid gastric emptying (RGE) leading to spikes in serum glucose may precede the onset of DM and gastroparesis. Clinical predictors of diabetic gastroenteropathy include abdominal bloating, female gender, high glucose levels, and high body mass index (BMI).
Postsurgical gastroparesis. Surgical vagotomy, performed for the treatment of refractory peptic ulcer disease, intentionally compromises the vagal innervation to the stomach in an effort to decrease gastric acid secretion. However, decreased vagal (parasympathetic) innervation also significantly prolongs gastric emptying, unless pyloroplasty is performed concurrently. Inadvertent vagal nerve injury may occur as a complication of procedures such as fundoplication and gastric bypass.
Viral/postviral gastroparesis. Gastroparesis can present as an acute symptom related to viral gastroenteritis, most commonly due to norovirus or enterovirus. It may also present in a delayed manner following a prodromal gastrointestinal (GI) or respiratory infection, known as postviral gastroparesis (PVGP), a subtype of idiopathic gastroparesis. While both conditions are typically self-limited, symptoms related to PVGP may be prolonged and persist for months to years. PVGP secondary to cytomegalovirus, Epstein–Barr virus, and varicella zoster virus infection typically result in the longest duration of symptoms.
Additional Diagnostic Consideration
Medications: Several classes of medication can alter gastric motor function and result in either accelerated or delayed gastric emptying. Prokinetic agents that accelerate gastric emptying, include metoclopramide, tegaserod, erythromycin, and domperidone. Medications that can delay gastric emptying include opiates, benzodiazepines, anticholinergics (i.e., atropine, dicyclomine, tricyclic antidepressants), calcium channel blockers, and aluminum-containing antacids, as well as phenobarbital, progesterone, and octreotide. Discontinuation of these medications for 48 to 72 hours prior to imaging is important to avoid false-positive or false-negative gastric emptying results due to medication effects.
Diagnosis
Severely delayed gastric emptying; possible vagal nerve injury.
✓ Pearls
Diabetic gastroenteropathy is the most common cause of gastroparesis.
Gastroparesis can be due to acute viral gastroenteritis or present following a viral prodrome (PVGP).
Surgical vagal nerve injury results in delayed gastric emptying unless pyloroplasty is also performed.
Numerous medications can result in false-positive or false-negative findings on gastric emptying studies.
Suggested Readings
Camilleri M, Parkman HP, Shafi MA, Abell TL, Gerson L. American College of Gastroenterology. Clinical guideline: management of gastroparesis. Am J Gastroenterol. 2013; 108(1):18–37, quiz 38 Mariani G, Boni G, Barreca M, et al. Radionuclide gastroesophageal motor studies. J Nucl Med. 2004; 45(6):1004–1028 Maurer AH. Gastrointestinal motility, part 1: esophageal transit and gastric emptying. J Nucl Med. 2015; 56(8):1229–1238Case 62

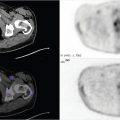
Clinical History
34-year-old female presenting with abdominal discomfort with meals (▶Fig. 62.1).
(Case courtesy of Joseph S. Fotos, MD, Penn State Hershey Medical Center.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree