Part 7 Genitourinary
Case 67
Clinical History
16-year-old female found to have bilateral hydronephrosis on renal ultrasound after evaluation for urinary tract infection (UTI) (▶Fig. 67.1).
Key Finding
Delayed washout on a Tc-99m MAG3 renography without diuretic augmentation
Top 3 Differential Diagnoses
Mechanical obstruction. When a patient is noted to have hydronephrosis on anatomic imaging, it is important to be able to delineate if the collecting system dilation is due to a mechanical obstruction, i.e., secondary to stricture, mass, or stone. This is the main reason behind performing diuretic renography in nuclear medicine. A collecting system that shows delayed washout on standard Tc-99m MAG3 renography, usually considered a half emptying time greater than 15 minutes, should be given a diuretic with continued dynamic assessment of the kidneys. If the collecting system washout remains delayed, it is suggestive of mechanical obstruction.
Vesicoureteral reflux (VUR). Not all cases of collecting system dilation are secondary to a mechanical obstruction. Urine is propagated from the renal pelvis, down the ureter, and into the bladder by smooth muscle cells. Any failure in this propagation can result in collecting system dilation even without the presence of a mechanical obstruction. This is known as a functional obstruction or functional retention. In these patients, the collecting system washout time will normalize after the administration of a loop diuretic as the resultant increased hydrostatic pressure (assuming functioning nephrons) overcomes the functional obstruction. A washout half time of less than 10 minutes after diuretic administration is definitely normal and less than 15 minutes is likely normal. VUR can cause a dilated but otherwise normal collecting system. Associated recurrent infection/inflammation can also lead to reduced ureteral peristalsis resulting in a functional obstruction.
Prior obstruction or infection. Previous but resolved mechanical obstruction or infection of the upper urinary tract can result in a dilated, but not obstructed, collecting system secondary to a patulous system with decreased peristalsis.
Additional Diagnostic Consideration
Primary megaureter: It is a term used to describe multiple entities involving a congenital abnormality of the distal ureter and ureterectasis. Primary megaureter can be refluxing, obstructing, or nonrefluxing and nonobstructing. Obstructed primary megaureter is thought to be secondary to an aperistaltic, possibly aganglionotic segment of the distal ureter similar to Hirschsprung’s disease in the colon. The adynamic segment results in proximal dilation from relative obstruction which may be overcome by increased hydrostatic pressure.
Diagnosis
Patulous extrarenal pelvis post UTI.
✓ Pearls
Diuretic renography is used to evaluate for a mechanical obstruction in a patient with hydronephrosis.
Increased hydrostatic pressure from the diuretic can normalize washout in a functional obstruction.
A dilated nonobstructed system can be from VUR, prior obstruction/infection, and primary megaureter.
Collecting system half washout in under 10 minutes after diuretic administration is not obstructed.
Suggested Readings
Berrocal T, López-Pereira P, Arjonilla A, Gutiérrez J. Anomalies of the distal ureter, bladder, and urethra in children: embryologic, radiologic, and pathologic features. Radiographics. 2002; 22(5):1139–1164 Taylor AT. Radionuclides in nephrourology, Part 2: pitfalls and diagnostic applications. J Nucl Med. 2014; 55(5):786–798Case 68

Clinical History
91-year-old male with recurrent metastatic prostate cancer admitted for urosepsis and acute renal failure with concern for ureteral obstruction (▶Fig. 68.1).
Key Finding
Decreased renal perfusion on dynamic renography
Top 3 Differential Diagnoses
Renal artery stenosis. Renal perfusion is evaluated by the dynamic acquisition of 1 to 5 second images for the initial 60 seconds of renal scintigraphy. Visually, activity should be in the renal arteries within seconds of activity in the aorta, usually around the same time activity reaches the aortic bifurcation. Semiquantitative evaluation is done using whole kidney and aorta regions of interest (ROI). The time–activity curve (TAC) for each kidney should show rapid climb, within seconds of a similar rapid climb in the aorta, and then peak and level off at a level similar to each other and above the level of the aorta. Decreased flow to either kidney may be secondary to renal artery stenosis (RAS), most frequently caused by atherosclerotic disease and fibromuscular dysplasia. External compression on the renal artery, such as from tumor or fibrosis, can appear similar. Angiotensin-converting enzyme inhibitor (ACEI)-augmented renography can be performed in the evaluation of renovascular hypertension (RVH).
Ureteral obstruction. It is important to identify ureteral obstruction and treat it as it can lead to obstructive nephropathy. Obstruction of urinary outflow results in increased intrarenal resistance due to both pressure and reactive vasoconstriction. Eventually, this results in decreased glomerular filtration rate (GFR) and, if left untreated, renal atrophy and fibrosis. Decreased renal flow on renal scintigraphy will not be the first sign of ureteral obstruction, but it is important to note along with other parameters indicating residual renal function.
Renal vein thrombosis. The inability for blood to drain out of the kidney can lead to pressure extending across the renal vascular bed that increases resistance to arterial flow. Renal vein extension from tumor, such as in renal cell carcinoma and Wilms tumor, is important to exclude with anatomic imaging.
Additional Diagnostic Considerations
Renal artery dissection: Dissection is not a frequent cause of decreased renal perfusion. Renal perfusion may be completely absent if there is resultant acute complete occlusion of the renal artery. If a perfused kidney is not seen in the renal fossa, ectopia and prior resection should be excluded first.
Poor injection technique: Poor injection bolus can result in a false positive for delayed flow. With a poor bolus, the TACs for the aorta and both kidneys will have a slow initial rise.
Subcapsular collection: A high-pressure subcapsular collection can result in increased renal resistance and manifestations similar to RAS, the so-called Page kidney.
Diagnosis
Likely prolonged right ureteral obstruction from pelvic adenopathy.
✓ Pearls
Decreased renal perfusion can result from slow blood in, slow blood out, or slow urine out.
It is important to ensure an adequate bolus of the radiopharmaceutical when evaluating renal perfusion.
Exclude renal ectopia or prior resection if a perfused kidney is not seen in the renal fossa.
Suggested Readings
Taylor AT. Radionuclides in nephrourology, Part 2: pitfalls and diagnostic applications. J Nucl Med. 2014; 55(5):786–798 Wolin EA, Hartman DS, Olson JR. Nephrographic and pyelographic analysis of CT urography: differential diagnosis. AJR Am J Roentgenol. 2013; 200(6): 1197–1203Case 69

Clinical History
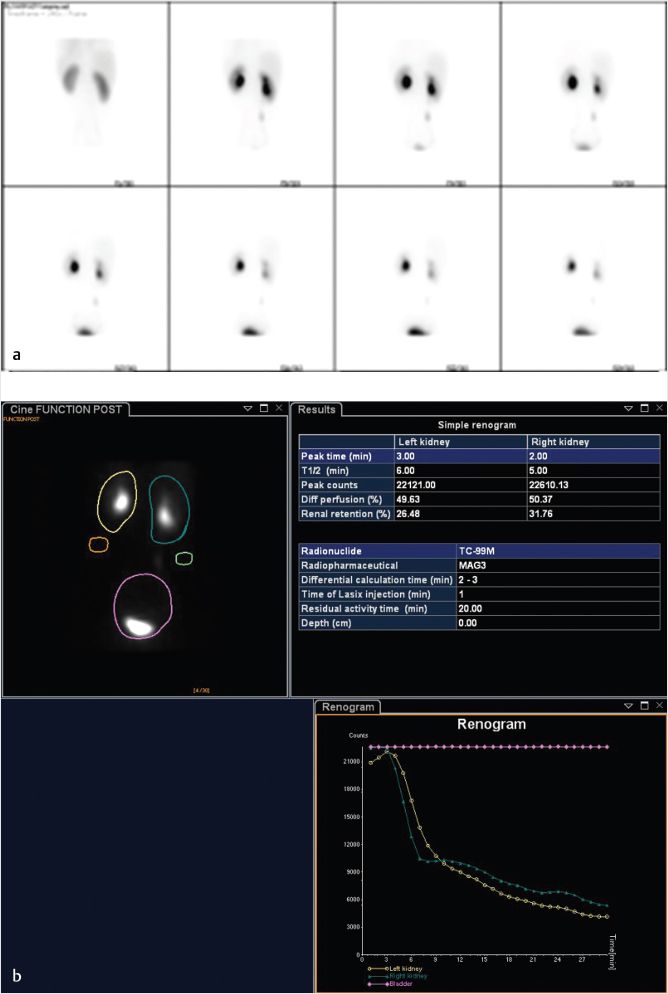
75-year-old female with chronic left hydronephrosis complaining of left lower back and flank pain (▶Fig. 69.1).
Key Finding
Delayed washout of the genitourinary collecting system on diuretic renography
Top 2 Differential Diagnoses
Mechanical obstruction. Evaluating a dilated genitourinary collecting system for mechanical obstruction is best done with diuretic renography. This involves performance of standard nuclear medicine renography with Tc-99m MAG3 with the addition of a diuretic, usually furosemide. The diuretic can be administered either 15 minutes prior to the radiopharmaceutical, at the same time as the radiopharmaceutical (time 0), or 20 minutes later after delayed clearance has already been shown without the diuretic. A TAC is created using either a whole kidney or collecting system ROI for generation of quantitative data. Washout will be delayed if a system is dilated secondary to mechanical obstruction, and the delay will persist despite the increased hydrostatic pressure from diuretic effect. A postdiuretic half emptying time (either from peak to half peak or from time of diuretic administration to half that level, depending on the protocol utilized) greater than 20 minutes is consistent with mechanical obstruction, whereas less than 10 minutes is normal. The 10- to 20-minute area is a nonspecific zone with many interpreting 10 to 15 minutes as “likely not obstructed” and 15 to 20 minutes as “likely obstructed.” Mechanical obstruction carries a broad differential, including stones, blood clots, sloughed papilla, crossing of iliac vessels, and benign or malignant strictures.
False positive for mechanical obstruction. A patulous collecting system will result in delayed washout of radiotracer but should normalize after diuretic administration. However, this requires an adequate response to the diuretic. Patients with dehydration or poor baseline renal function may fail to mount a full response. A larger dose of furosemide might also be needed to overcome the so-called reservoir effect in a markedly patulous system. A full or neurogenic urinary bladder increases back pressure into the collecting system and can also mimic obstruction. This can be relieved with catheterization, if the patient is unable to empty their bladder spontaneously.
Diagnosis
Obstructed left renal collecting system.
✓ Pearls
Diuretic renography can help delineate if genitourinary collecting system dilation is due to obstruction.
Washout half time over 20 minutes on diuretic renography is suggestive of mechanical obstruction.
Renal failure and dehydration can cause a false-positive exam due to poor diuretic response.
Furosemide dose is typically around 40 mg for adults, based on renal function, and 1 mg/kg for children.
Suggested Readings
Boubaker A, Prior JO, Meuwly JY, Bischof-Delaloye A. Radionuclide investigations of the urinary tract in the era of multimodality imaging. J Nucl Med. 2006; 47(11):1819–1836 McQuillan BF, Zelasko S, Wolin EA. Nuclear medicine genitourinary imaging in native kidneys. J Am Osteopath Coll Radiol. 2016; 5:14–20 Taylor A, Jr, Nally JV. Clinical applications of renal scintigraphy. AJR Am J Roentgenol. 1995; 164(1):31–41Case 70

Clinical History
46-year-old male with history of pyeloplasty 2 years prior for congenital ureteropelvic junction (UPJ) obstruction with improved but persistent right flank and testicular pain (▶Fig. 70.1).
Key Finding
Increased cortical retention on MAG3 renal scan
Top 2 Differential Diagnoses
Acute renal failure. TC-99m MAG3 is excreted almost entirely by tubular secretion. MAG3 is removed from the blood by a transporter located in the basolateral membrane of the proximal tubule. It then accumulates in the cells of the proximal renal tubule before being transported to the lumen of the tubule by organic ion transporters in the apical membrane. In renal failure, the apical membrane transporter is impaired more than the basolateral transporter and MAG3 can be extracted into the tubule cells with a greater efficiency than it is transported to the tubular lumen, resulting in retained cortical activity. Furthermore, any insult to the kidney will usually result in decreased GFR prior to decreased tubular function. This allows for radiotracer to continue to reach the tubules and be secreted into the tubular lumen, but decreased GFR results in decreased filtrate washing out the tubules, visible as cortical retention on scintigraphy. In acute renal failure, MAG3 renal scintigraphy will demonstrate preserved renal blood flow during the flow phase of the study. There will be cortical retention with retained cortical activity at 20 min possibly approaching 100%. Normally, at 20 min the retained activity should be less than 30% of the peak activity. The TAC will demonstrate a gradually rising slope well past the point where the cortical activity would be expected to decrease.
Chronic renal failure. While chronic renal failure will also demonstrate delayed cortical retention during renal scintigraphy, the TAC will usually demonstrate a plateau as opposed to gradually rising slope as is seen with acute renal failure due to loss of function of both the basolateral and apical membrane transporters in the renal tubule cells. There may also be decreased renal blood flow with reduced extraction of tubular agents such as MAG3. The kidneys may appear smaller than normal.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree