Pediatric brain tumors are the most common solid tumor of childhood. This article focuses on the metabolic signature of common pediatric brain tumors using MR spectroscopic analyses.
Key points
- •
Pediatric brain tumors are the most common solid tumor in children and the leading cause of death in this patient population.
- •
Magnetic resonance spectroscopy (MRS) enables the radiologist to identify tumor tissue, to grade tumors, to differentiate tumor types, to distinguish active tumor from radiation necrosis or scar tissue, to guide stereotactic biopsy sites, and to determine early response to treatment.
- •
MRS may provide prognostic information used to guide therapy early on in the patient’s treatment, effectively improving outcomes and minimizing side effects.
- •
Taurine has been established as an important biomarker in distinguishing medulloblastomas (the most common posterior fossa neoplasm in children) from other common pediatric brain tumors, such as cerebellar astrocytomas.
- •
In spite of being grade I tumors, pilocytic astrocytomas typically show significantly elevated choline (Cho) peaks, Cho/NAA and Cho/creatine ratios, along with reduced NAA and creatine peaks and presence of lactate on MR spectroscopy.
- •
The presence of high myo-inositol (mI) levels strongly suggests a diagnosis of ependymoma.
- •
In the brainstem glioma, a citrate peak can be demonstrated at approximately 2.6 ppm and can be used to follow tumor progression.
- •
Studies have suggested that mI level could be used as a marker for tumor grading in astrocytoma, whereas higher levels could be found in low-grade (grade II) astrocytoma compared with higher-grade astrocytoma or glioblastoma.
- •
Choroid plexus papillomas (CPP) typically demonstrate significantly elevated myo-inositol peak, low creatine, and decreased choline when compared with choroid plexus carcinomas (CPC).
- •
MRS may provide additional information in cases in which the differential diagnosis by neuroimaging is difficult, such as tumor versus infection, tumor versus tumefactive demyelinating lesions, and tumor versus radiation necrosis.
Introduction
Second only to leukemia as the most prevalent malignancy of childhood, the brain tumor is the most common solid tumor among children, significantly surpassing other types of solid tumors (eg, sarcomas, carcinomas, and lymphoma) as the leading cause of death in the pediatric patient population.
Proton nuclear magnetic resonance spectroscopy (1H-MRS), a noninvasive, in vivo technique that provides additional metabolic diagnostic indices beyond anatomic information, has been extensively used to evaluate brain tumors. Magnetic resonance spectroscopy (MRS) enables the radiologist to identify tumor tissue, to grade tumors, to differentiate tumor types, to distinguish active tumor from radiation necrosis or scar tissue, to guide stereotactic biopsy sites, and to determine early response to treatment.
Several studies have demonstrated that most tumors have decreased N-acetyl-aspartate (NAA) (neuronal/oligodendrocytic marker), stable creatine (Cr), except in instances of energy failure (tumor necrosis), and increased choline (Cho) (increased membrane turnover, cellularity).
Compared with long echo-time (TE) spectroscopy, short TE spectroscopy enables the detection of additional metabolites that are characterized by a shorter T2 relaxation time at an improved signal-to-noise ratio (SNR), including, among others, taurine (Tau), glutamine plus glutamate (Glx), myo-inositol plus glycine (mI + gly), and alanine (Ala). These metabolites have demonstrated some utility in the diagnosis of specific tumor histology.
In this article, we discuss posterior fossa tumors, supratentorial parenchymal and extraparenchymal tumors, and pineal region tumors. We also describe the differential diagnosis of focal brain lesions that may resemble brain tumors.
Introduction
Second only to leukemia as the most prevalent malignancy of childhood, the brain tumor is the most common solid tumor among children, significantly surpassing other types of solid tumors (eg, sarcomas, carcinomas, and lymphoma) as the leading cause of death in the pediatric patient population.
Proton nuclear magnetic resonance spectroscopy (1H-MRS), a noninvasive, in vivo technique that provides additional metabolic diagnostic indices beyond anatomic information, has been extensively used to evaluate brain tumors. Magnetic resonance spectroscopy (MRS) enables the radiologist to identify tumor tissue, to grade tumors, to differentiate tumor types, to distinguish active tumor from radiation necrosis or scar tissue, to guide stereotactic biopsy sites, and to determine early response to treatment.
Several studies have demonstrated that most tumors have decreased N-acetyl-aspartate (NAA) (neuronal/oligodendrocytic marker), stable creatine (Cr), except in instances of energy failure (tumor necrosis), and increased choline (Cho) (increased membrane turnover, cellularity).
Compared with long echo-time (TE) spectroscopy, short TE spectroscopy enables the detection of additional metabolites that are characterized by a shorter T2 relaxation time at an improved signal-to-noise ratio (SNR), including, among others, taurine (Tau), glutamine plus glutamate (Glx), myo-inositol plus glycine (mI + gly), and alanine (Ala). These metabolites have demonstrated some utility in the diagnosis of specific tumor histology.
In this article, we discuss posterior fossa tumors, supratentorial parenchymal and extraparenchymal tumors, and pineal region tumors. We also describe the differential diagnosis of focal brain lesions that may resemble brain tumors.
Posterior fossa tumors
Medulloblastoma
Medulloblastoma (MB), a highly malignant neoplasm, is the most common posterior fossa neoplasm in children, representing 15% to 20% of all pediatric brain tumors and 30% to 40% of posterior fossa neoplasms. The tumor usually arises at the midline within the vermis and exhibits growth into the fourth ventricle.
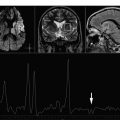
On computed tomography (CT), the tumor is usually characterized as hyperdense, and on T2 images, as isointense to hypointense compared with gray matter ( Fig. 1 A ). These imaging findings are likely secondary to high cell density and high nuclear-to-cytoplasmic ratio.
Apparent diffusion coefficient (ADC) values are significantly lower in MBs than in all other posterior fossa tumors ( P <.001) related to high cell density (see Fig. 1 B).
Typical spectral findings
Cho
On MRS, MBs usually demonstrate a significant elevation of the Cho peak related to the high cell density and elevated Cho/Cr and Cho/ NAA ratios, reflecting its malignant nature (see Fig. 1 C). High Cho has been previously reported as a characteristic finding of primitive neuroectodermal tumors (PNETs).
In a study by Carles Majós and colleagues, significantly elevated levels in Cho peak were used to distinguish PNET from non-PNET tumors with a high degree of accuracy (94%). Elevation of the Cho peak is useful in distinguishing between MB and L’Hermitte-Duclos disease (LDD), as MBs occasionally present with a laminated appearance, and with no contrast enhancement, may mimic LDD. The Cho peak is typically elevated in patients with MB when compared with patients with LDD.
Tau
Spectra with a short TE show a significantly elevated Tau concentration at 3.3 ppm in patients with MB when compared with other tumors (see Fig. 1 C). Further, at a TE of 30 ms, the Tau peak projects above the baseline; whereas, at a TE of 144 ms, the Tau peak occurs below the baseline.
Tau has been established as an important biomarker in distinguishing MBs from other common pediatric brain tumors, such as cerebellar astrocytomas. Although higher Tau levels are associated with increased cellular proliferation and tumoral aggressiveness, decreased ADC combined with elevated levels of Cho and Tau, often suggest more significant malignancy in MBs.
Glutamine and glutamate
In a study of 60 children with untreated brain tumors, Panigrahy and colleagues measured the highest glutamate (Glu) concentrations in pineal germinoma and in MB (see Fig. 1 C). Specifically, the MB, pineal germinoma, and astrocytoma showed mean Glx concentrations above the mean in all tumors; whereas, Glx concentration was low in both the choroid plexus papilloma and carcinoma. The quantitation of these metabolites proved useful in separating either MB or astrocytoma from the choroid plexus papilloma.
Ala
Ala levels, when elevated, are readily detectable in specific diseases, including meningioma, glioblastoma, and MBs. Consistent with this, Panigrahy and colleagues report the highest mean Ala concentration among posterior fossa tumors in MBs.
Lipids
Prominent lipid (Lip) resonances were observed in some, but not all, spectra of malignant MB (see Fig. 1 C). In an in vitro, high-resolution analysis of the lipid content in the tissue serum and cerebrospinal fluid (CSF) of patients with primary brain tumors, Srivastava and colleagues demonstrated that proton MRS of the lipid extract of serum (blood specimen collected before the surgical procedure) and surgically discarded tissue had a significantly larger number of total cholesterol–containing and Cho-containing phospholipids in patients with MB and glioblastoma multiforme as compared with healthy subjects. This study supports the role of Lip estimation in CSF and tissue serum as a complementary diagnostic tool for evaluating pediatric brain tumors preoperatively.
Lactate
High lactate (Lac) values are usually found in the spectra (see Fig. 1 C).
Final considerations
Prognosis
Although significant differences exist between the metabolite profiles of metastatic and localized MB at presentation, localized tumors with metabolite profiles similar to those that have metastasized are at increased risk of relapse ( Table 1 ). Metastatic tumors, for example, are characterized by higher total Cho (tCho), which is consistent with increased cell turnover and tumor growth, a finding substantiated by a significant positive correlation between tCho and the Ki67 index.
| Metastatic Medulloblastoma | Localized Medulloblastoma |
|---|---|
| Higher total choline Higher taurine | Higher mobile lipids Higher lactate Lower creatine |
Tau is present in both metastatic and localized tumors, although higher levels are typically found in metastatic tumors, which is consistent with previous findings in neuroblastoma (ie, Tau is a reliable biomarker for more aggressive subtypes of neural tumors). The fact that higher mobile Lip levels are observed in localized tumors may also reflect a higher proportion of nonviable tumor in these cases.
Therapeutic response
MRS may be used to assess therapeutic response in patients with MB. If an elevation of the Cho peak is seen within the margins of the surgical bed, residual or recurrent tumor should be considered ( Fig. 2 ). In cases in which the patient has received radiation therapy (RT), the extent of disease must be carefully interpreted. Specifically, a transient elevation of the Cho peak may be seen and a follow-up should be performed to distinguish RT effects from tumor recurrence.
Late chemotherapy/radiotherapy effects
In a study evaluating the neuro-metabolic alterations in pediatric survivors of posterior fossa tumors, Rueckriegel and colleagues demonstrated that concentrations of NAA were significantly decreased in the respective white ( P <.0001) and gray matters ( P <.0001) of patients with MB compared with NAA levels in healthy controls. Further incremental decreases of metabolite concentrations in patients with MB compared with concentrations found in patients with pilocytic astrocytoma (PA) may point to additional harm caused by irradiation and chemotherapy.
Metastases
Metastases from MB will present with the same spectral abnormalities as those described for the primary tumor. After chemotherapy, MRS and diffusion may help assess therapeutic response.
Atypical Teratoid/Rhabdoid Tumor
Children with atypical teratoid/rhabdoid tumors (ATRTs) of infancy and childhood present at a younger age than those with MB, with the median age at diagnosis 2 to 4 years. (The median age for diagnosis of MB is about 6 years). Girls are more affected than boys, and most ATRTs (94%) are intra-axial, occurring in the infratentorial compartment in 47% of cases.
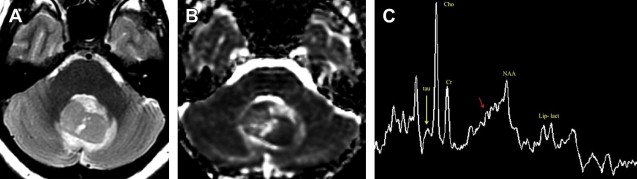
Neuroimaging characteristics of ATRT ( Fig. 3 A–C ) can be similar to those of MB in the posterior fossa; to germ-cell tumors; and to PNETs when arising in the supratentorial compartment. however, the prognosis is worse than that typically associated with MB.
Typical spectral findings
MRS shows elevated Cho and reduced NAA as well as a prominent Lip peak (see Fig. 3 D–E). However, there are no reports in the literature that quantify these changes or address the presence or size of Tau peaks.
Final considerations
To differentiate these tumors from MBs, we should consider the following.
Location
ATRTs tend to be more lateral in location and may compromise the cerebello pontine angle.
Heterogeneity
ATRTs tend to be more heterogeneous in signal intensity when compared with MBs. Hemorrhage and blood products may be seen.
Cerebellar Astrocytoma
Cerebellar pilocytic astrocytoma (CPA), one of the most common posterior fossa tumors (second only to MB), is often diagnosed as a juvenile PA, with excellent survival after gross total surgical resection. The differential diagnosis between CPA and MBs is crucial, however, because treatment and prognosis differ completely. The diagnosis is made by the following neuroimaging characteristics.
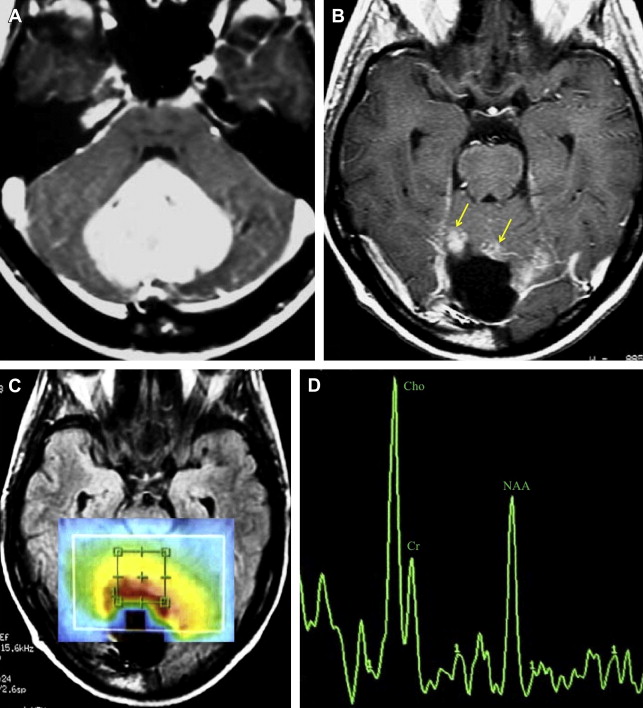
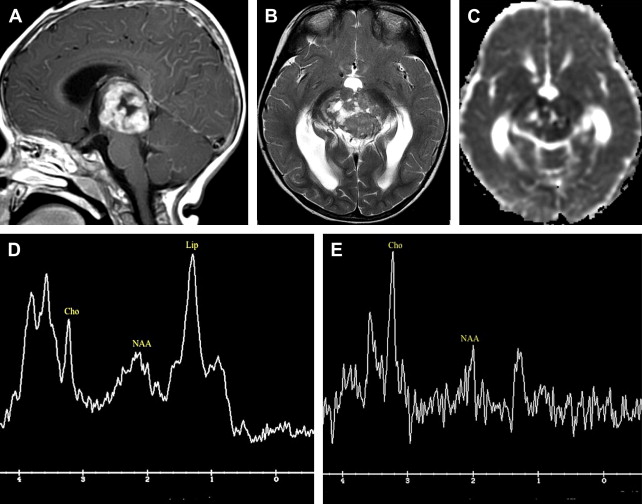
T2 characteristics
The enhancing solid component of CPA ( Figs. 4 B and 5 B ) is typically hyperintense on T2 images (see Figs. 4 A and 5 A) compared with the normal cerebellar parenchyma. By contrast, the solid component of MBs is usually isointense or hypointense (see Fig. 1 A) to normal cerebellar parenchyma on T2 images. However, higher-grade astrocytomas may manifest lower signal intensity on T2-weighted images, effectively mimicking MBs.
Diffusion characteristics
The solid component of the CPA has greater ADC values (see Figs. 4 C and 5 C) than do other cerebellar tumors, such as ependymoma, ATRT, and MB (see Fig. 1 B).
MRS
The Tau peak, considered very characteristic of MBs, is not typically demonstrated in PAs.
Typical spectral findings
Cho
Increases in tCho may be reliably correlated with the grade of a glioma; however, tCho is not an effective or accurate biomarker for grade I PAs that show a wide range of tCho values, including those demonstrating a marked increase. In fact, high Cho content and Cho/Cr and Cho/NAA ratios are consistently demonstrated in CPA despite the benign clinical course for tumors of this type (see Figs. 4 D and 5 D, E).
Lac
Apart from tumor necrosis, there are several possible reasons for elevated Lac levels in this histologically benign tumor (see Figs. 4 D and 5 D, E), including an abnormal number (or dysfunction of) mitochondria, which could interfere with oxidative phosphorylation and electron transport, alterations in proportional oxygen delivery, oxygen extraction or usage by the tumor, or anaerobic glycolysis by tumor cells.
Cr
In a study of untreated pediatric brain tumors, Panigrahy and colleagues demonstrated that Cr was significantly reduced in PA (see Figs. 4 D and 5 D, E), thereby distinguishing tumors of this type from all other posterior fossa tumors ( P >.000001). Schneider and colleagues also found that total creatine (tCr) was significantly reduced in circumscribed PA, clearly distinguishing them from other tumors.
Final consideration
Posterior fossa compared with suprasellar PAs
Interestingly, some investigators have reported significant differences in the spectral composition between the cerebellar and suprasellar PAs, with significantly higher mI and glutamate/glutamine peaks in suprasellar tumors, and a trend toward lower Cr in cerebellar tumors. However, Panigrahy and colleagues have shown no differences between the spectroscopic patterns of supratentorial and infratentorial PA.
Further, there have been no significant differences identified in MRS profiles between pediatric and adult PAs.
Ependymoma
Ependymomas are the fourth most common posterior fossa tumors in children following MB, cerebellar astrocytoma, and brainstem glioma. The most important imaging finding in identifying an ependymoma is extension of the tumor through the fourth ventricular outflow foramina ( Fig. 6 A, B ) ; however, this feature is not entirely pathognomonic, as some MBs may extend through the fourth ventricular exit foramina. In addition, they usually show more bulbous extension and restricted diffusion rather than small amounts of tissue through the foramina that is characteristic of an ependymoma.
Punctate calcification is demonstrated in 50% of ependymoma cases on CT. These tumors are heterogeneous on magnetic resonance (MR) imaging (see Fig. 6 ), reflecting a combination of solid tumor, cyst, calcification, necrosis, edema, or hemorrhage.
When performed, perfusion MR of ependymoma generally demonstrates markedly elevated cerebral blood volume (CBV) (see Fig. 6 D) and, unlike many other glial neoplasms, poor return to baseline that may be attributable to fenestrated blood vessels and an incomplete blood brain barrier (BBB). In the authors’ experience, some ependymomas demonstrate significantly high permeability while no significant elevation of the permeability is demonstrated in other cases (see Fig. 6 E).
Typical spectral findings
MRS shows considerable heterogeneity.
mI
Short echo spectra (TE = 30 ms) show low to very high mI (see Fig. 6 F, G), although never as high as in choroid plexus papillomas (CPPs) ( Fig. 7 ).
In a study by Harris and colleagues, the presence of high mI levels strongly suggests a diagnosis of ependymoma when short TE is used at 1.5 T. Ependymomas and infiltrative low-grade gliomas show higher levels of mI compared with MBs and PAs.
Cr
Harris and colleagues suggest that ependymomas have higher Cr levels than do astrocytomas and MBs.
Glx
Schneider and colleagues also demonstrated that ependymomas are characterized by an elevation in mI and Glx.
Brainstem Glioma
Brainstem tumors represent 10% to 20% of all central nervous system (CNS) tumors in childhood. Most brainstem gliomas are diffuse and involve the pons. Diagnosis is based on the characteristic changes on MR imaging of diffuse T2 hyperintense expansion of the brainstem without biopsy ( Fig. 8 ).
Single voxel MRS (SV-MRS) is usually selected over chemical shift imaging (CSI) to evaluate brainstem gliomas. This ensures that the quality of individual tumor spectra is not adversely affected by unavoidable compromises accompanying CSI acquisitions from larger volumes. In addition, the processing and quality control of CSI are more time consuming, and require the expertise of a skilled MR spectroscopist.
Typical spectral findings
Cho
Although Cho/NAA and Cho/Cr ratios are elevated in diffuse brainstem gliomas (DIBGs) (see Fig. 8 C, D), mean tCho concentration in DIBGs is lower than is mean tCho in normal-appearing brainstems in controls. This may be an indicator of low membrane turnover and may explain, in part, the low sensitivity of DIBGs to RT. Total Cho could also serve as a surrogate marker to identify tumors that are less proliferative but also less likely to respond to RT.
Citrate
A citrate peak can be demonstrated at approximately 2.6 ppm (adjacent to the Glx peak) and can be used to follow tumor progression (see Fig. 8 D). Reduced citrate levels may indicate malignant transformation of these tumors, or may be related to chronic administration of steroids, RT, and/or chemotherapy. Although the citrate signal is most prominent and most often observed in DIBGs, it is also noted in other common pediatric brain tumors and in the developing brain of infants younger than 6 months.
Final considerations
Low-grade versus high-grade pontine gliomas
The spectral pattern in pontine gliomas is related to aggressiveness. Proton MRS and perfusion imaging may be useful in differentiating low-grade (usually focal) pontine tumors, which have lower Cho peaks and lower blood volumes, from high-grade tumors in which the Cho/Cr ratio is usually higher.
Malignant transformation
Available literature suggests that at least a subset of diffuse pontine gliomas is histologically low grade (World Health Organization [WHO] grade II) at initial clinical presentation, but rapidly evolve into high-grade neoplasms, with most found to be glioblastoma multiforme at postmortem examination. This finding is consistent with a very high rate of mortality: 90% of patients succumb within 2 years after initial diagnosis.
Some studies suggest that MRS might be a useful early predictor of disease progression, preceding clinical and radiological deterioration. Metabolic changes indicative of malignant transformation include increased levels of tCho, decreased metabolite ratios of NAA/tCho and Cr/tCho, and increased levels of Lips. In addition, a significant reduction in the “apparent” citrate levels may also be associated with malignant transformation.
Therapeutic response
MRS may be used in estimating therapeutic response or tumor progression. Using multivoxel MRS (MV-MRS), Laprie and colleagues followed 8 patients with diffuse pontine glioma in a series of studies from diagnosis to the time of response to RT and found that Cho:NAA values decreased, followed by an increase at the time of relapse.
In a study by Thakur and colleagues, 2 pediatric patients with diffuse pontine tumors showed clinical improvements following RT; however, MRS showed an overall increase in Cho/Cr and Cho/NAA ratios, indicating tumor progression. Although these findings seem contradictory, the disease did, in fact, progress in both patients. There is now evidence from 3 independent studies that MRS identifies subjects with progressing disease and impending relapse several months before clinical manifestations of the illness. This finding could be important for assessing the efficacy of novel treatment strategies in individual patients early on in the plan of care.
Supratentorial tumors
Astrocytoma
Pilocytic astrocytomas (PAs) are the most common glial tumors in children. They are typically well demarcated with T2 signal abnormality roughly equivalent to the amount of gadolinium enhancement. Occasionally, these tumors present with an associated cyst. Supratentorial astrocytomas are most commonly located in the optic/hypothalamic region ( Fig. 9 ), but can also be found in the brain parenchyma ( Fig. 10 ).

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree