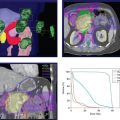
FIGURE 18-2. RTOG consensus guidelines for contours on pelvic lymph nodes in high-risk prostate cancer.
1. INTRODUCTION
• Definitive or adjuvant radiotherapy (RT) has contributed significantly to the successful management of urologic and gynecologic malignancies. Conventional RT is performed through either anteroposterior (AP) parallel-opposed fields or a four-field technique consisting of an anterior, a posterior, and two lateral portals. However, the use of conventional portals has been reported to result in incomplete coverage of the intended target volume and higher doses to normal tissues.1–3 Early studies by Bonin et al.4 and Pendlebury et al.5 reported inadequate coverage of the external iliac lymph nodes using standard irradiation fields in 45% and 62% of patients, respectively.
• The lack of conformality via conventional techniques is also associated with normal tissue complications. According to various criteria to classify the severity of the radiation side effects, severe complications may develop in 8% to 10% of patients treated with a conventional beam arrangement. The incidence of complications requiring surgical management is approximately 5%.6
• As chemoradiotherapy has become the integral therapeutic measure in either the definitive or postoperative setting, gastrointestinal (GI) complications have been the most significant concern other than hematologic side effects.
• Results from the early Radiation Therapy Oncology Group (RTOG) 79-20 study suggest that in a select group of patients, the use of extended fields covering the para-aortic lymph nodes is associated with better disease-free and overall survival compared with pelvic RT alone.7 However, when the lymph nodes are grossly enlarged, para-aortic lymph node RT combined with chemotherapy proved to be highly toxic in the RTOG 92-10 study. Although the acute hematologic toxicity was higher in patients receiving chemoradiotherapy than in those receiving RT alone, RTOG 92-10 clearly showed that 50% (15 of 30 patients) experienced grade 4 nonhematologic toxicity after therapy, and all 15 of those toxicities were bowel related. The cumulative incidence of late grade 3 and 4 toxicity was 34% at 36 months.8
• Techniques such as intensity-modulated radiation therapy (IMRT), which allows adequate target coverage in the pelvic and para-aortic lymph nodes while keeping the dose delivered to the critical organs such as the small bowel to a minimum, would be of tremendous interest and may permit combining high-dose RT and chemotherapy without prohibitive GI complications. Minimizing the volume of the GI tract inside the radiation field is pivotal to the potential improvement of the therapeutic ratio by IMRT.
• Portelance et al.9 demonstrated that IMRT for cervical cancer yields similar tumor coverage with superior normal tissue sparing compared with conventional beam arrangements. Similar findings were also reported in a study from the University of Chicago.10
• Guo et al.3 showed a significant reduction in volume of small bowel and rectum irradiated to 45 Gy with IMRT compared with conventional plans for endometrial cancer. In addition to the small bowel and rectum, Heron et al.2 showed a reduction to bladder volume dose using IMRT.
• Mundt et al.11 found reduced grade 2 acute GI toxicities in patients who received IMRT compared to conventional whole pelvic radiotherapy (WPRT), 60% versus 91%, respectively, when treating for cervical and endometrial carcinoma.
• Kidd et al.12 reported the results of 452 cervical cancer patients treated with IMRT or non-IMRT with 50 Gy delivered to the pelvic lymph nodes and found reduced grade ≥3 bowel or bladder toxicities in favor of IMRT. There was also improved overall survival and cause-specific survival.
• Kachnic et al.13 reported the early toxicity results of RTOG 0529, a phase II trial of dose-painted IMRT with chemotherapy for anal carcinoma, in which elective pelvic nodes were treated to 45 Gy, and found low rates of grade 3 or higher GI toxicity of 7%. This was compared favorably to the 35% grade 3 and 4 GI toxicity, primarily diarrhea, reported in RTOG 9811.14
• The dosimetric advantage of IMRT may potentially improve the therapeutic outcome in patients with locally advanced cervical cancer, especially when the pelvic/para-aortic lymph nodes are grossly enlarged and a higher radiation dose is required.
• Patient- and tumor-related issues have hindered the acceptance of IMRT for patients with gynecologic malignancies.
º The first is related to the organ motion of the pelvic structures; for example, the uterus and cervix may shift as much as 4 to 5 cm on an AP projection, depending on whether the bladder and rectum are empty or full.1 Other studies regarding inter- and intrafraction organ motion have shown less shift while undergoing RT.15,16
• The second concern that hinders the widespread use of IMRT for gynecologic cancer is the lack of an objective description of pertinent lymph node locations in a three-dimensional (3D) projection. However, because the lymph node status is extremely important in determining the prognosis of gynecologic and urologic malignancies, IMRT plans must provide adequate coverage of the pelvic, para-aortic, and inguinal draining nodes when these are at risk.
2. IMAGING FOR PARA-AORTIC, PELVIC, AND INGUINAL LYMPH NODES
• Without computed tomography (CT) or magnetic resonance imaging (MRI), lymphangiography (LAG) can be an alternative to pelvic and para-aortic imaging.
• CT and MRI may be equally effective as LAG in detecting enlarged lymph nodes; however, small lymph nodes containing microscopic disease (clinical target volume [CTV]) are often difficult to identify using CT and MRI on the basis of size.
• Most institutions use CT to gather imaging data for IMRT treatment planning. Inconsistencies in visualizing unenlarged lymph nodes on pelvic and abdominal CT imaging could impose significant variations in target delineation among different physicians.
• Although LAG would greatly aid in determining the target volumes accurately, few institutions perform these technically difficult, uncomfortable, and time-consuming studies.
• In earlier Gynecologic Oncology Group (GOG) studies, LAG was considered the best option for detecting para-aortic nodal metastasis. The GOG studied the clinical–pathologic correlation of para-aortic lymph node involvement by CT, LAG, and ultrasonography in patients with stage IIB, III, and IVA cervical carcinoma. Of 264 patients evaluated, the LAG sensitivity was 79%, with a specificity of 73%. The sensitivity of CT and ultrasonography was 34% and 19%, with a specificity of 96% and 99%, respectively.17 However, LAG was also associated with some shortcomings in detecting metastatic internal iliac and presacral nodes, which are only occasionally seen.
• Scheidler et al.18 concluded that LAG, CT, and MRI perform equivalently in the detection of grossly enlarged metastatic pelvic lymph nodes from cervical cancer.
• Chao and Lin19 demonstrated that the nodal CTV can be better delineated by LAG-aided CT imaging. The combination of LAG, to demonstrate nodal texture, and CT, for spatial orientation, provides a better tool to delineate the CTV for the para-aortic, pelvic, and inguinal lymph nodes than relying solely on CT or MRI.
•
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree