14 Percutaneous Suprapubic Cystostomy
Wael E.A. Saad
The following are indications of suprapubic catheter placement:
- Adults: Bladder outlet obstruction/catheter placement
- Acute urine retention (AUR)
- Defined as sudden and painful inability to pass urine
- By far the most common indication
- This occurs in 10% of men in their 70s or 80s over any given 5-year period (10% risk of occurrence in a 5-year period in men over 70 years of age)
- Suprapubic catheterization is considered second in line to transurethral catheterization in cases of AUR in the majority (>85%) of urologists.
- Posttraumatic avulsion on the urinary bladder from its neck or in cases of posttraumatic bladder leakage with multiple other traumas (a temporizing measure for a less significant and less life-threatening injury: bladder injury) (Fig. 14.1).
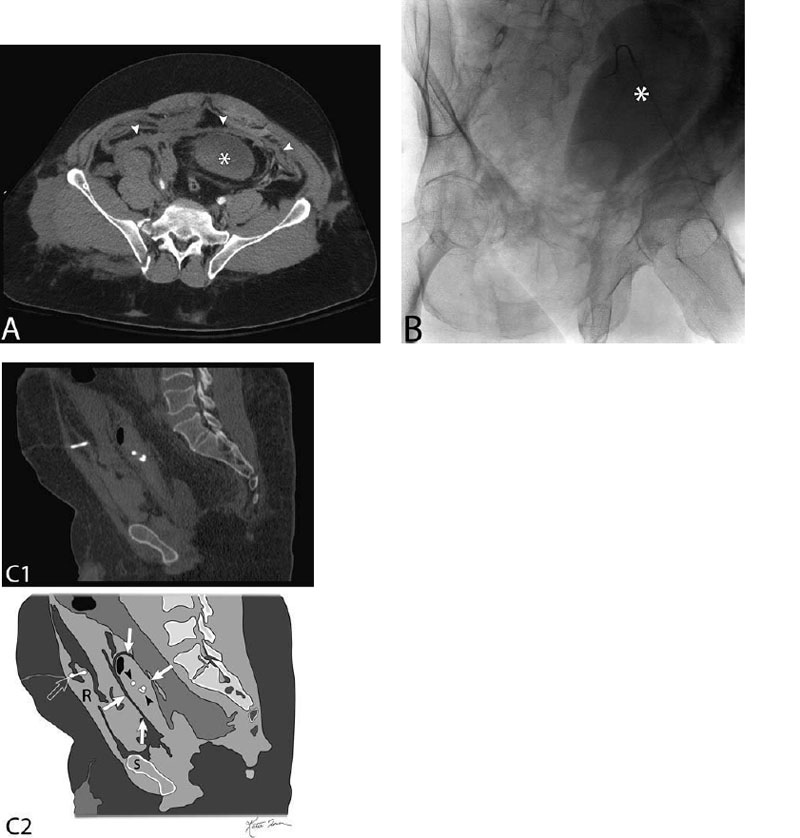
Fig. 14.1 Suprapubic catheter (cystostomy) in a detached urinary bladder. (A) Contrast-enhanced axial computed tomography (CT) image of the upper pelvis in a patient status postblunt trauma (car accident). The image demonstrates fluid/blood in the peritoneum from the trauma (arrowheads). This blood (arrowheads) is most likely blood from pubic rami fractures (not shown). The urinary bladder (*) is seen high riding because it has been detached/avulsed from its neck. (B) An oblique fluoroscopic image during angiography demonstrating the pear-shaped avulsed urinary bladder (*). The underlying angiographic catheter is in the arteries for pelvic angiography and a subsequent embolization. (C) Sagittal reconstruction of an unenhanced CT of the pelvis after a suprapubic catheter has been placed (top) and schematic sketch of it (bottom). The suprapubic catheter is seen traversing the anterior abdominal wall (hollow arrow) and coiled in the urinary bladder (arrowheads). The urinary bladder sits between the four solid arrows (R, rectus abdominis; S, symphysis pubis).
- Urinary bladder access as a first step for a subsequent intervention in cases where retrograde urethral annulation has failed (not common)
- Removing urinary bladder stones
- Fulgurating superficial premalignant lesions in the urinary bladder
- Antegrade cannulation of the urethra to help guide retrograde cannulation
- Pediatric: Bladder aspiration for fever workup
- To obtain a sterile urine sample in fever workup (septic infants)
- Uncorrected coagulopathy. Relative versus absolute contraindication depends on the degree of coagulopathy, the clinical setting, and the degree of urgency of the percutaneous fluid drainage procedure.
- Status posttotal cystectomy
- Confirm the location of the bladder (central in the pelvis and sits above prostate)
- Confirm that the bladder is central and not pushed off to the side (Fig. 14.1).
- Rule out other objects/structures (pathology versus normal structures) that may mimic the bladder in the pelvis by ultrasound
- Dilated fluid-filled bowel loops
- Duplication cysts (gastrointestinal duplication cysts)
- Giant urinary bladder Hutch diverticulum
- Urachal cysts
- Lymphoceles
- Ovarian cysts
- Cystic tumors (the most confusing tumors are most likely ovarian cystic tumors)
- Evaluate the percutaneous window to the urinary bladder and check that nothing stands between the anterior abdominal wall and the anterior bladder wall
- Look for adjacent organs that can be inadvertently traversed
- Small bowel and decompressed redundant large bowel
- This can help reduce transgression of adjacent organs with subsequent potential major complication.
- Laboratory value evaluation mostly revolves around ruling out coagulopathy
- Suggested coagulopathy thresholds for a suprapubic urinary bladder catheter
- International normalized ratio: ≤1.7–1.8
- Platelets: ≥50,000
- Activated partial thromboplastin time: ≤50 seconds
- Multiarray 4–5 MHz ultrasound transducer
- Transducer guide bracket (if needed)
- Sterile transducer cover