12 Percutaneous Transhepatic Biliary Drainage
Wael E.A. Saad
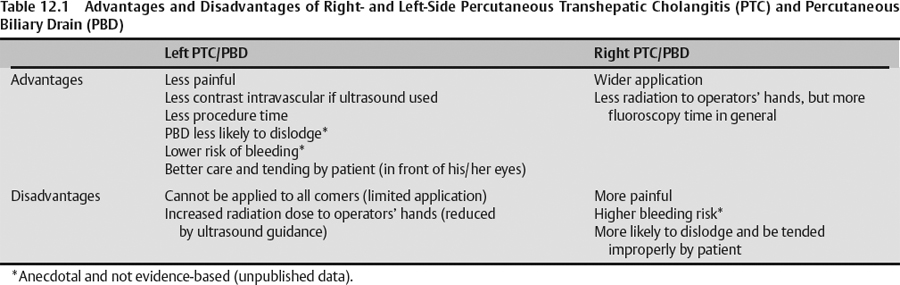
The indications of ultrasound-guided percutaneous transhepatic cholangiography (PTC) with or without subsequent percutaneous biliary drainage (PBD) are usually directed at the left hepatic lobe where the left biliary ducts lie. Right-side PTC with or without PBD is almost always performed under fluoroscopy. The focus of this chapter is on ultrasound-guided left bile duct access with or without drainage. Table 12.1 lists the advantages and disadvantages of right versus left PTC and PBD.
The following are indications of PTC and PBD placement whether right sided or left sided:
- Drainage of an obstructed biliary tract
- Cholangitis
- Pruritus
- High bilirubin with a patient who is a chemotherapy candidate
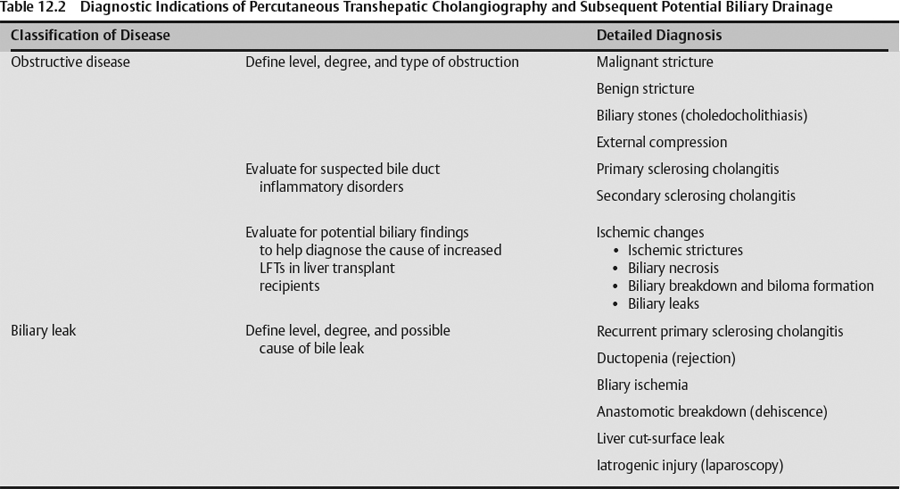
- Diagnostic evaluation of obstructive jaundice (Table 12.2)
- Providing a portal (percutaneous access) for minimally invasive biliary interventions
- For percutaneous removal of biliary stones
- Transhepatic fluoroscopic-guided stone removal
- Combined endoscopic retrograde cholangiopan-creatogram (ERCP) and transhepatic fluoroscopic stone removal (rendezvous procedure)
- Transhepatic endoscopic and fluoroscopic stone removal
- For biliary interventions
- Balloon dilation of biliary strictures
- Traversal of transected bile ducts (bile leaks/injury)
- Brush biopsy/sampling for diagnosis of cause of obstruction
- For placement of brachytherapy
- Bile diversion
- Uncorrected coagulopathy. Relative versus absolute contraindication depends on the degree of coagulopathy, the clinical setting, and the degree of urgency of the PBD procedure.
Preprocedural imaging evaluation is focused on the left hepatic lobe and bile ducts.
- Evaluate
- Look for adjacent organs that can be inadvertently traversed
- This may make the operator consider approaching the bile ducts from the right and not the left, if there is close proximity of viscera or if the left lobe is very high up in the chest and covered by the rib cage, particularly costal cartilage.
- This helps plan the needle trajectory for the PTC/PBD.
- This can help reduce transgression of adjacent organs with subsequent potential major complication.
- Particular organs that may be traversed include the colon, heart, stomach, and diaphragm/lung.
- Laboratory value evaluation mostly revolves around ruling out coagulopathy.
- Suggested coagulopathy thresholds are
- International normalized ratio (INR): ≤1.4
- Platelets (PLT): ≥50,000 – 70,000
- Activated partial thromboplastin time (aPTT): ≤50 seconds
- Serum creatinine
- This is more important in decompressed biliary systems when approaching from the intercostal approach (right side) utilizing fluoroscopy only. In this situation, large volumes of contrast may be inadvertently injected intravenously (in the hepatic and/or portal veins) in an attempt to opacify the decompressed bile ducts. Intravascular contrast injection may have a toll on the kidney, especially with a poor baseline renal function.
- Utilizing ultrasound for access guidance for the left biliary system requires minimal contrast, and if ultrasound-guided left biliary access is successful, there will be no inadvertent contrast injection into the circulation.
- Indications
- Alternatives
- To refuse the procedure
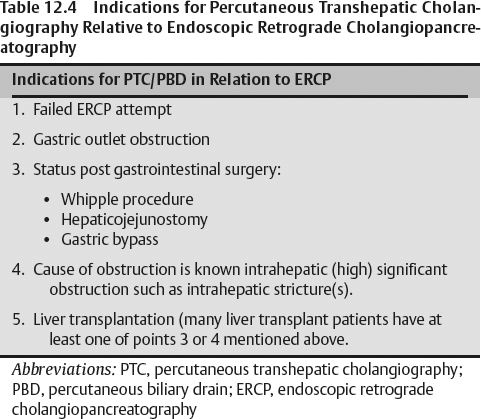
- ERCP is the first line of therapy. PTC/PBD is reserved as the second line of therapy. Table 12.4 lists the indications for PTC/PBD following ERCP or where ERCP is a forgone failure.
- Procedural risks
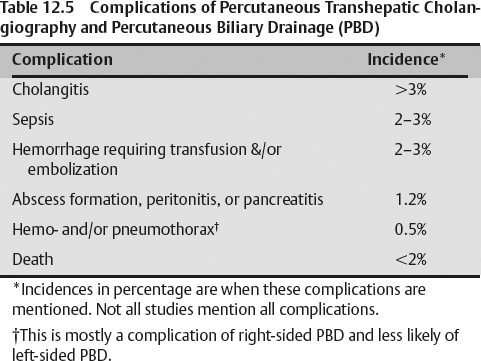
- Infection (Table 12.5)
- This complication in its broader definition occurs in more than 3% of cases.
- Infection can be divided into cholangitis (most common), biliary sepsis (most serious), or perihepatic abscess (least common).
- Patients should receive prophylactic antibiotics prior to any transhepatic biliary procedure. Intravenous antibiotics used include Zosyn (Wyeth Pharmaceuticals, Madison, NJ): 3.375 g intravenously (IV; primary antibiotic used by the authors) and ciprofloxacin: 400 mg IV.
- Bleeding (Table 12.5)
- Most common presentation of bleeding is bleeding from the biliary drain (hemobilia/upper gastro-intestinal bleeding).
- It may present as pain and/or hypotension and a computed tomography (CT) scan may show
- Subcapsular hematoma
- Active extravasation in the few cases where CT IV contrast is used
- Bleeding may be transient with or without blood transfusion.
- In rare cases, bleeding may require intervention such as transcatheter hepatic arterial embolization or exploratory surgery.
- Injury to surrounding organs and/or structures (Table 12.5)
- Pleura (pneumo- and hemothorax)
- Multiarray 4–5 MHz ultrasound transducer
- Doppler capabilities to differentiate bile ducts from blood vessels
- Transducer guide bracket
- Sterile transducer cover
- Chlorhexidine skin preparation/cleansing fluid
- Fenestrated drape
- 21-gauge infiltration needle
- 10 to 20 mL 1% lidocaine syringe
- 11-blade incision scalpel
- 21- to 22-gauge needle allows a 0.018-inch wire. If the needle is placed in the intended target calyx, upsizing the wire to a 0.035-inch wire (additional step) is usually required prior to nephrostomy tube placement.
- The needle can be a diamond tip 21-gauge needle.
- The needle can be a 15-cm 22-gauge Chiba needle.
- Telescoped graduate dilation system with metal stiffener (Neph-set [Cook Corp., Bloomington, IN] or AccuStick [Boston Scientific, Natick, MA]) to upsize 0.018-inch wire to 0.035-inch wire.
- An 8-French fascial dilator that can be passed over a 0.035-inch guidewire may be used (see below).
- An 8-French self-retaining (string-locking) pigtail drainage catheter, which is the definitive biliary tube/drain to be placed last (final product of the procedure).
- Required for moderate sedation and fluid replenishment/resuscitation
- Required for IV prophylactic antibiotics such as
- Zosyn 3.375 g
- Ciprofloxacin 500 mg
- Determine easiest visibility of left lobe intrahepatic bile ducts
- Place Doppler ultrasound near the target bile ducts to differentiate them from blood vessels. False-positives would be thrombosed blood vessels that are not common.
- Assess left hepatic lobe mobility with breathing and the patient’s ability to fixate the visualized bile ducts by breath holding
- Correlate and triangulate the access site (at skin) and the target bile ducts to choose and mark the skin access site
- Avoid the rib cage. Make sure the needle trajectory does not cross costal cartilage or ribs.
- It is preferable that the needle skin entry site be 1.5 to 2.0 cm from the subcostal margin to reduce post-procedural chest wall pain complications.
- Make sure the base of the heart is clear from the needle trajectory
- Make sure that the hepatic parenchymal tract to the target bile duct is clear of hepatic cysts or tumors (preferable, but not a must)
- The transducer (along with the bracketed needle guide) is used to choose and triangulate the skin entry site, the target bile duct, and the needle trajectory to achieve the above points. The traditional/common transducer orientation is transverse to the patient’s abdomen/spine and longitudinal along the long axis of the left hepatic lobe. However, a slight panning toward the xyphoid/chest can also be adopted.
- The operator must not only think of successfully “hitting” the target duct, but also of using an ideal angle as well, so that a wire can be passed from lateral to medial to cannulate the left biliary system and be able to internalize the biliary drain if need be.
- Skin preparation/cleansing in the region that was chosen as an ultrasound imaging portal and a needle access needle portal
- Place a fenestrated drape at the chosen and prepared skin region
- Utilizing a 21-gauge (by at least a 3.7-cm-long) infiltration needle, 1% lidocaine infiltration is performed, infiltrating down to the sensitive hepatic capsule.