Key Points
- •
Ultrasound guidance for insertion of a peripheral intravenous (IV) catheter is a useful technique in patients with nonpalpable or nonvisualizable veins.
- •
Patient and operator positioning are critical to success when using ultrasound to obtain peripheral IV access.
- •
A scan of the upper extremity venous anatomy should be performed to identify the best site for peripheral IV insertion before attempting the procedure.
Background
Difficult peripheral venous access is a frequent challenge confronting clinicians. Using ultrasound guidance to establish peripheral venous access provides more precise localization of veins and prevents multiple puncture attempts.
Many studies have demonstrated benefits of placing peripheral intravenous catheters (IVs) using ultrasound guidance. In the emergency department, ultrasound-guided placement of peripheral IVs reduced the need for central venous access in 85% of patients. In addition, placement of peripheral IVs with ultrasound guidance is more likely to be successful than blind placement of external jugular IVs. One study of intensive care unit patients found a 36% increase in success of peripheral IV placement using ultrasound guidance compared with usual methods.
Ultrasound-guided placement of peripheral IVs can be used in any patient, but the technique is particularly useful in patients with nonpalpable or nonvisualizable peripheral veins. Nurses, physicians, and other healthcare providers have successfully learned ultrasound-guided peripheral IV placement through focused training courses.
Differentiating Arteries and Veins
Arteries can be differentiated from veins based on pulsatility, compressibility, wall thickness, and Doppler appearance. Arterial walls are thicker, more echogenic, and less compressible and venous walls are thinner, less echogenic, and easily compressible (anterior wall touches the posterior wall under light pressure). Arterial pulsations can be visualized with two-dimensional imaging, but color or spectral Doppler may be used when uncertain. Color flow in veins can be augmented by compressing distally, whereas color flow in arteries remains unchanged with distal compression ( Table 29.1 ).
| Arteries | Veins |
|---|---|
| Noncompressible under light pressure | Compress easily under light pressure |
| Thick, echogenic walls | Thin, nearly imperceptible walls |
| Round shape | Variable shape |
| Pulsatile | Nonpulsatile (may appear pulsatile by transmission of pulses from an adjacent artery) |
| Color flow unchanged with distal compression | Color flow augmented by distal compression |
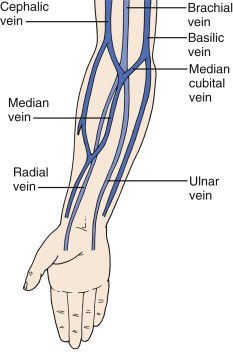
Normal Anatomy
The anterior forearm, antecubital fossa, and medial upper arm are the most common sites for performing ultrasound-guided peripheral IV placement ( Figure 29.1 ). The brachial, cephalic, and basilic veins are the largest upper extremity veins and can be easily accessed for placement of peripheral IVs with ultrasound guidance.
Technique
Patient Position
The procedure can be performed with patients in a sitting or supine position. Operator comfort is critical to procedural success, especially in patients with difficult anatomy, and positioning should maximize both operator and patient comfort. The ultrasound machine should be positioned behind the area of insertion within the operator’s direct line of sight, avoiding the need for head turning or awkward body positioning. The patient’s arm should be fully extended and externally rotated with the palm facing upward. A tourniquet should be placed proximal to the area of insertion.
Identification of Insertion Site
The arm should be scanned to identify potential insertion sites prior to skin preparation. Using a linear transducer (5–12 MHz), scan the most common insertion sites in a transverse plane. The imaging depth should be set to 2–2.5 cm to avoid vessels deeper than 2.5 cm, which have a lower likelihood of successful cannulation. One study showed a higher failure rate with deep (>1.2 cm) as well as proximal vessels. Evaluate veins for size, depth from skin surface, proximity to arteries, and signs of thrombosis (noncompressibility or intraluminal echogenic material). The ideal vein is large, superficial, and distant from arteries. Image the vein’s course along the arm or forearm and select the most accessible distal site.
Ultrasound Preparation
After an insertion site is chosen, the skin should be sterilized with chlorhexidine or a similar solution per local protocol. The operator should clean the face and sides of the transducer thoroughly with antiseptic wipes. A sterile transducer cover may be used, and sterile ultrasound gel is recommended for the procedure.
Catheter Selection
Most standard peripheral IV catheters are too short to be inserted into deeper peripheral veins. Longer IV catheters have less risk of premature failure due to dislodgement compared to shorter IV catheters, especially in obese and edematous patients. Catheters that are at least 48 mm in length (1.88 in) are preferred. If longer IV catheters are not available, arterial line catheters may be used as an alternative.
Transverse versus Longitudinal Approach
One small study found no difference in success rate using a transverse versus longitudinal approach, yet a transverse approach was found to be faster. We recommend that novice operators initially learn a transverse approach. More experienced operators that are skilled at performing real-time, ultrasound-guided procedures may prefer to use a longitudinal approach.
Transverse Approach
With the target vessel in the middle of the screen, the IV catheter should be inserted distal to the ultrasound probe at a distance approximately equal to the depth of the vessel. With a transverse approach, the operator slowly advances the IV catheter and subtly tilts the transducer to maintain the needle tip in sight. The operator must maintain the needle tip in sight, and the needle tip should be visualized in the same plane as it enters the vessel. Once a flash of blood is observed, the angle of the needle should be reduced and the catheter advanced over the needle into the vein ( Figures 29.2 and 29.3 ).











