Chapter 32 Peritoneal Cavity and Gastrointestinal Tract
Introduction
The network of connections formed by the peritoneal reflections serves to provide continuity between the abdominal walls and the organs therein. In addition, it also bridges the retroperitoneum with the peritoneum. These connections not only serve a physiologic and life-sustaining role but also act as a pathway for spread of disease.1 These processes include inflammation, infection, trauma, and importantly, tumor.
Primary tumors of the peritoneum are rare.2 Most commonly, primary tumor elsewhere metastasize to the peritoneum. Patients present with vague and nonspecific symptoms. Therefore, imaging plays a key role in the diagnosis of peritoneal disease. Because of the spaces and compartments formed by the peritoneal reflections, there are predictable patterns of disease spread that can be anticipated with certain tumors. Common tumors that spread and metastasize to the peritoneum include stomach, colon, ovarian, and pancreatic cancer and lymphoma.
Peritoneal disease could not be assessed in a direct manner radiographically before the advent of cross-sectional imaging.3 With improving technologies such as multidetector row computed tomography (CT), positron-emission tomography/computed tomography (PET/CT), magnetic resonance imaging (MRI), and ultrasound, peritoneal metastasis can now be readily evaluated and followed on scans for surveillance.
Anatomy
Embryology
To fully understand the peritoneum, a basic understanding of its embryologic development is necessary.4–7 However, to explain the complex and detailed embryologic development of the peritoneum is not the purpose of this chapter. Briefly, the primitive gut is suspended within the peritoneal cavity by a dorsal and ventral primitive mesentery, which divides the peritoneum into a right and a left cavity. Unlike the ventral mesentery, the dorsal mesentery does not stop its attachment at the stomach, but continues to connect the primitive gut to the posterior abdominal wall inferiorly. The absence of the ventral mesentery in the lower abdomen allows for communication between the left and the right abdominal cavity.
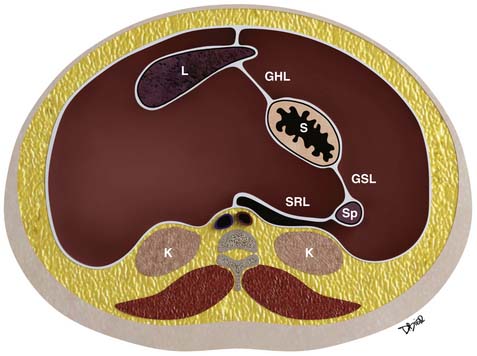
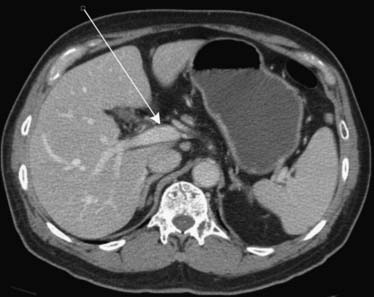
Further growth, organ development, elongation, cavitation, and rotation form the adult peritoneum (Figures 32-1 and 32-2). This includes the formation of the lesser sac, which is isolated from the remainder of the peritoneum or greater sac, except at a small opening called the foramen of Winslow.
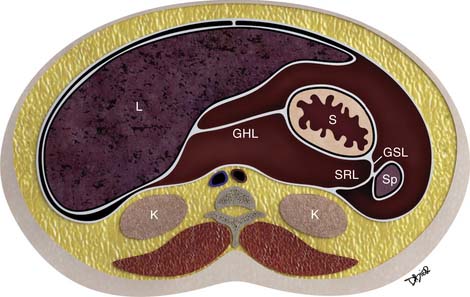
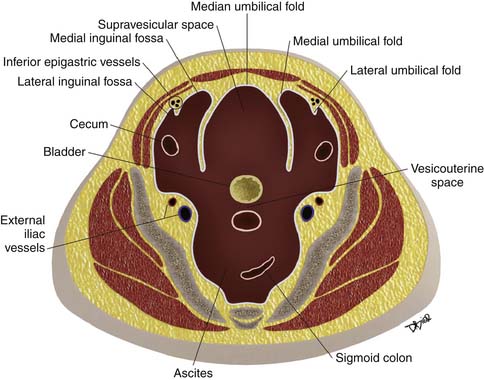
Figure 32-2 Peritoneal structures in the adult, position and relationships.
(Illustration courtesy of David Bier.)
A single layer of mesothelial cells forms the peritoneum. It is separated from the submesothelial layer of connective tissue by a basal lamina. The submesothelial layer of connective tissue consists of collagen, elastic fibers, fibroblast-like cells, arteries, veins, and lymphatics.6 The submesothelial layer or subperitoneal space is a virtual space that allows continuity between the mesenteries, the ligaments, the abdominal wall, and the retroperitoneum, as are described further.
Visceral and Parietal Peritoneum
The peritoneum is classified as either visceral or parietal.8 The abdominal and pelvic walls are lined by the parietal peritoneum. This includes the anterior surface of the retroperitoneum, the abdominal wall, and the undersurface of the hemidiaphragm. Conversely, the visceral peritoneum covers the intraperitoneal organs or viscera and forms the omenta and mesenteries.
In males, the greater peritoneal cavity is a closed continuous cavity. Conversely, in females, it is discontinuous at the ostia of the oviducts, providing a communication between the peritoneal cavity and the lower pelvis, which is extraperitoneal.6
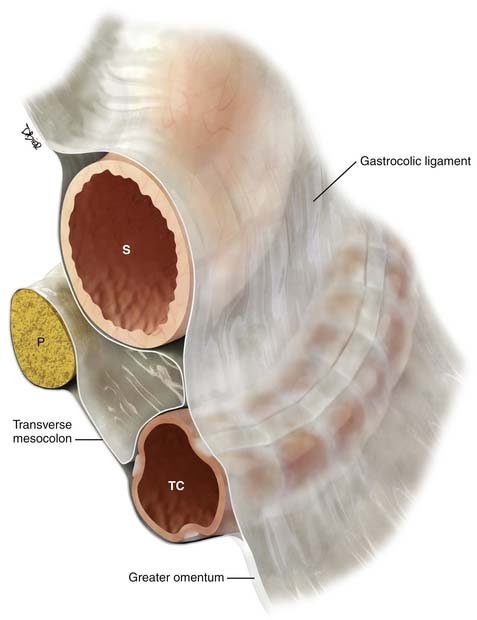
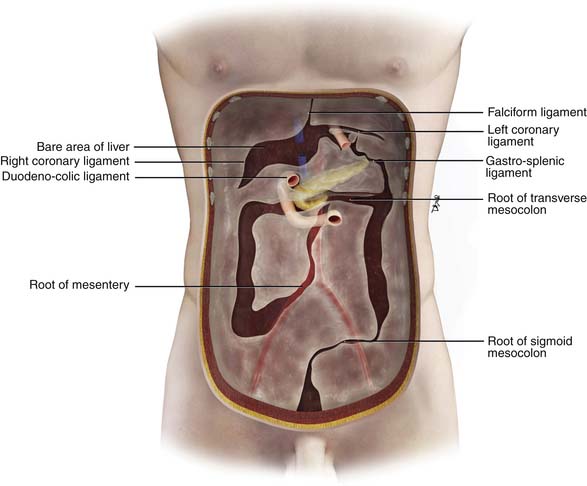
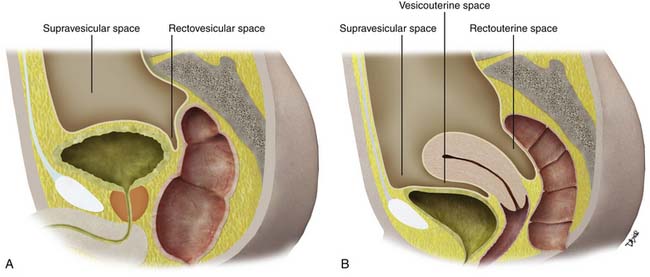
Double folds of the peritoneum result in formation of ligaments and mesenteries. They suspend and form the supporting structure for the peritoneal organs. For example, the mesentery suspends the small bowel within the peritoneal cavity. The mesentery serves also to carry the arteries, lymphatics, and nerves. The omenta are formed from a double fold of the visceral peritoneum that extends from the stomach (Figures 32-3 and 32-4). The peritoneal cavity is divided into various interconnecting compartments by the ligaments and mesenteries.
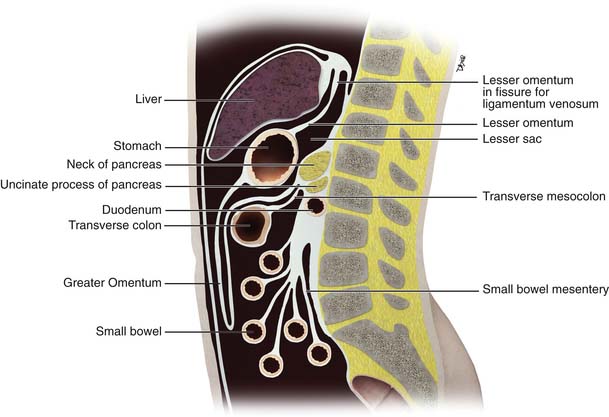
Figure 32-3 The peritoneal structures in midsagittal view, diagrammatic representation.
(Illustration courtesy of David Bier.)
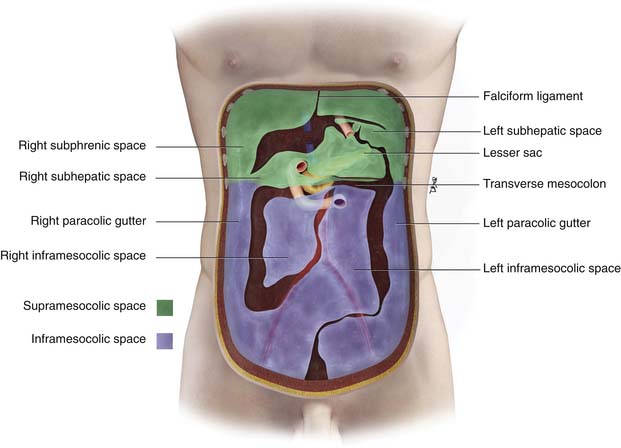
Supramesocolic and Inframesocolic Space
The peritoneal cavity is divided into a supramesocolic and an inframesocolic space by the transverse mesocolon9 (Figure 32-5). The supramesocolic space is further divided into the right and left supramesocolic space by the falciform ligament. The left supramesocolic space is then further subdivided into the anterior and posterior perihepatic spaces. The right supramesocolic space also is subdivided into the anterior perihepatic space and a posterior compartment known as the lesser sac. The right and left supramesocolic space communicates via the foramen of Winslow, allowing communication between the lesser sac and the remainder of the peritoneal cavity or greater sac. There is continuity between the right paracolic gutter and the right supramesocolic space. However, the phrenicocolic ligament acts as a barrier between the left paracolic gutter and the left supramesocolic space.
Important supporting ligaments in the supramesocolic space include the gastrohepatic ligament, hepatoduodenal ligament, gastrocolic ligament, gastrosplenic ligament, and splenorenal ligament (Figures 32-6 to 32-8). The ligaments are anatomically connected and continuous and their location and relationship can be identified by certain landmarks, mostly vasculature (Table 32-1).
Table 32-1 Supramesocolic Ligaments: Their Organ Relationship and Landmarks
| LIGAMENT | ORGAN RELATIONSHIP | LANDMARKS |
|---|---|---|
| Gastrohepatic ligament | Lesser curvature of the stomach to left hepatic lobe | Left gastric vessels and left gastric nodal station |
| Hepatoduodenal ligament | Lesser curvature of the stomach to the hepatic hilum | Portal vein, hepatic artery, extrahepatic bile duct, and nodal stations |
| Gastrocolic ligament/supracolic omentum | Greater curvature of the stomach to the body of the transverse colon | Perigastric branches of the left gastroepiploic vessels with anastomosis to the right gastroepiploic vessels |
| Greater omentum | Transverse colon extending as an apron anterior to the small bowel | Epliploic vessels and branches of the gastroepiploic vessels |
| Gastrosplenic ligament | Continuous and to the left of the gastrocolic ligament, from the greater curvature of the fundus and upper body of the stomach to the splenic hilum | Short gastric vessels and left gastroepiploic vessels |
| Splenorenal ligament | Continuity between the spleen and the tail of the pancreas | Distal splenic artery or proximal splenic vein |
The inframesocolic compartment is divided into a right and a left inframesocolic space by the obliquely oriented small bowel mesentery. The ascending colon provides the lateral border of the right inframesocolic space. The inframesocolic compartment consists of the root of the mesentery, jejunal mesentery, ileal mesentery, ascending mesocolon, descending mesocolon, sigmoid mesentery, and the pelvic floor and peritoneal folds (Table 32-2).
Table 32-2 Inframesocolic Compartment, Organ Relationship, and Landmarks
| LIGAMENT | ORGAN RELATIONSHIP | VASCULAR LANDMARKS |
|---|---|---|
| Root of mesentery | From the horizontal portion of the duodenum to the right iliac fossa | SMA, SMV, and ileocolic artery and vein |
| Ileal mesentery | From the root of the mesentery to the ileum | Ileal artery and veins |
| Ascending mesocolon | Root of the mesentery to the ascending colon | Right colic artery and vein, cecal artery and vein |
| Jejunal mesentery | From the base of the mesentery to the jejunum | Jejunal artery and vein |
| Descending mesocolon | Base of the transverse mesocolon along the tail of the pancreas to the descending colon | Left colic artery and vein |
| Sigmoid mesocolon | Root of the sigmoid mesocolon | Sigmoid arteries, superior hemorrhoidal artery and vein |
SMA, superior mesenteric artery; SMV, superior mesenteric vein.
Paravesicular Spaces
Peritoneal folds or reflections in the pelvis also result in potential spaces and compartments10–12 (Figures 32-9 and 32-10). The urinary bladder, obliterated umbilical arteries, and inferior epigastric vessels indent upon the parietal peritoneum to form the anterior and posterior paravesicular spaces.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree