Ascites: Fluid in dependent recesses of peritoneal cavity
 Varices: Well-defined, tubular or serpentine collateral vessels with same enhancement as adjacent veins
Varices: Well-defined, tubular or serpentine collateral vessels with same enhancement as adjacent veins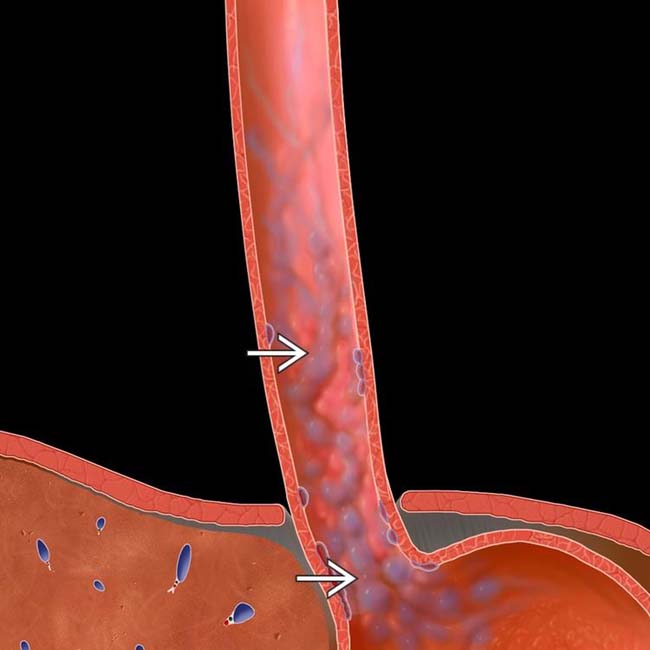
 as serpiginous, longitudinally oriented submucosal venous collaterals extending into the gastric fundus.
as serpiginous, longitudinally oriented submucosal venous collaterals extending into the gastric fundus.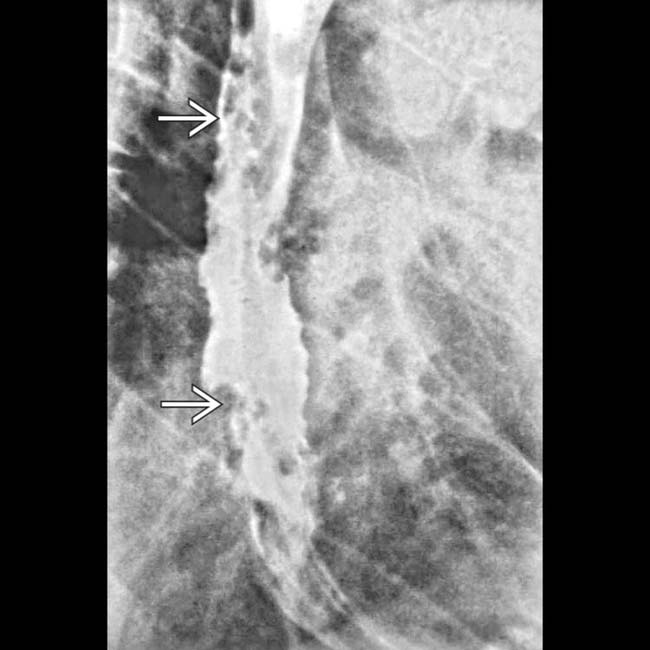
 in the esophageal wall. Varices are usually pliable and easily compressed. Varicoid carcinoma could have a similar appearance.
in the esophageal wall. Varices are usually pliable and easily compressed. Varicoid carcinoma could have a similar appearance.
 in the left upper quadrant in communication with the splenic vein and the left renal vein
in the left upper quadrant in communication with the splenic vein and the left renal vein  , which appears dilated, forming a splenorenal shunt.
, which appears dilated, forming a splenorenal shunt.
 in the portal and superior mesenteric veins, with calcification suggesting chronicity. Portal hypertension increases the risk of portal vein thrombus due to stasis and slow flow.
in the portal and superior mesenteric veins, with calcification suggesting chronicity. Portal hypertension increases the risk of portal vein thrombus due to stasis and slow flow.TERMINOLOGY
Definitions
• Portal hypertension: Elevated portal pressures due to resistance to portal flow, defined as absolute portal venous pressure of > 10 mm Hg or gradient between portal and systemic veins of > 5 mm Hg
• Varices: Abnormally dilated and tortuous veins due to rerouting of blood flow away from liver into lower pressure systemic veins through collateral pathways
IMAGING
General Features
• Common features of portal hypertension
 Varices: Well-defined, tubular or serpentine portosystemic collateral vessels with same enhancement as adjacent veins
Varices: Well-defined, tubular or serpentine portosystemic collateral vessels with same enhancement as adjacent veins
 Slow or reversed flow in portal veins on Doppler ultrasound
Slow or reversed flow in portal veins on Doppler ultrasound
 Varices: Well-defined, tubular or serpentine portosystemic collateral vessels with same enhancement as adjacent veins
Varices: Well-defined, tubular or serpentine portosystemic collateral vessels with same enhancement as adjacent veins Slow or reversed flow in portal veins on Doppler ultrasound
Slow or reversed flow in portal veins on Doppler ultrasound– Eventually, portal flow may be biphasic (alternating hepatopetal/hepatofugal flow) or completely reversed
• Varices: Types or locations
 Left gastric venous collateral vessels
Left gastric venous collateral vessels
 Esophageal varices
Esophageal varices
 Paraesophageal varices
Paraesophageal varices
 Recanalized paraumbilical vein
Recanalized paraumbilical vein
 Abdominal wall varices
Abdominal wall varices




 Left gastric venous collateral vessels
Left gastric venous collateral vessels– Vascular channels in triangular fatty tissue between medial wall of upper gastric body and posterior margin of left hepatic lobe in lesser omentum
 Esophageal varices
Esophageal varices– Dilated tortuous submucosal venous plexus of esophagus can be divided into “uphill” and “downhill” varices
 Uphill varices (collateral blood flow into superior vena cava (SVC) from portal vein via azygous vein): Result from portal hypertension and found in distal 1/2 of esophagus
Uphill varices (collateral blood flow into superior vena cava (SVC) from portal vein via azygous vein): Result from portal hypertension and found in distal 1/2 of esophagus
 Uphill varices (collateral blood flow into superior vena cava (SVC) from portal vein via azygous vein): Result from portal hypertension and found in distal 1/2 of esophagus
Uphill varices (collateral blood flow into superior vena cava (SVC) from portal vein via azygous vein): Result from portal hypertension and found in distal 1/2 of esophagus– CECT has limited sensitivity for small esophageal varices, which may not be evident when collapsed
 Paraesophageal varices
Paraesophageal varices– Collateral vessels in posterior mediastinum behind esophageal wall connect coronary vein with azygos and hemiazygos veins and vertebral plexus
 Recanalized paraumbilical vein
Recanalized paraumbilical vein– Dilated collateral vein (≥ 3 mm) arising from left portal vein and coursing between medial and lateral segments of left hepatic lobe in anterior edge of falciform ligament
 Abdominal wall varices
Abdominal wall varices– Prominent collateral veins radiating from umbilicus referred to as “caput medusae” (head of Medusa, a mythological figure who had snakes for hair)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree