Clinical Background on Prostate Cancer Recurrence
Radical prostatectomy (RP) remains the most common primary treatment for primary localized prostate cancer (PCa) and offers definitive cure in most patients. Primary whole gland radiation and ablative therapies also can achieve high success rates in appropriate patient populations. However, the incidence of biochemical recurrence (BCR) ranges from 19 to 35% at 10 years following radical prostatectomy and around 30% following primary radiation therapy, 1 posing a challenge in terms of further diagnosis and treatment. Biochemical recurrence, also variously called prostate specific antigen (PSA) failure or biochemical failure, is defined most commonly as two consecutive elevated serum PSA values above 0.2 ng/mL following RP. This definition is not universal, as Cookson et al identified 53 different definitions of BCR in a sampling of 145 papers. 2 The initial rise in serum PSA marks a crucial point in disease management as it can be the initial indicator of subsequent disease progression or eventual PCa related mortality. 3 Importantly, BCR can precede clinically evident disease recurrence by 7 to 10 years (mean, 8 years). 4 Detection of BCR serves as a trigger for further imaging-based evaluation to localize the site of any clinically evident recurrence (whether local or distant) so that targeted salvage therapy may be initiated to interrupt progression to PCa-related mortality.
Following RP, serum PSA is expected to rapidly fall to undetectable levels and is then routinely followed post-treatment at periodic intervals, typically every 6 to 12 months for 5 years and yearly thereafter. 5 Presence of any detectable serum PSA provides as an exquisitely sensitive marker for recurrence and thus serves as a simple and robust follow-up test. Although, as stated above, the traditional definition of BCR is two consecutive serum PSA values > 0.2 ng/mL, some have argued that an alternate criterion PSA value of 0.4 ng/mL with a subsequent rising level should be used. This alternative criterion may increase the specificity for clinically relevant recurrence as it has been shown to be more predictive of metastatic progression. 3, 6 Infrequently, the PSA level can remain persistently detectable postoperatively without ever reaching a zero nadir, which is typically due to residual noncancerous prostate tissue, subtotal carcinoma resection, or undetected distant metastasis at the time of surgery. In this situation, imaging may be obtained, and if negative, PSA may then be followed more closely (every 3 to 6 months) 5 than in patients achieving an undetectable PSA.
Although BCR is used as an early marker of primary treatment success, the natural history in patients with BCR is highly variable, ranging from an indolent nonprogressing pattern to rapid progression to end-stage disease. As such, it may be useful to additionally define the PSA doubling time (PSAdt) or PSA velocity (PSAvel), which have additional implications for predicted rates of progression. A short PSAdt of < 6 months and high PSAvel > 0.5 ng/mL/month are associated with an increased risk of progression, distant metastasis, and PCa-related mortality. 1, 7 A relatively indolent disease course is often seen with a long PSAdt > 6 months and low PSAvel. Other predictors of an increased risk of progression, metastasis, and PCa-related mortality include a Gleason score > 8 and early BCR occurring less than 24 months following primary treatment. 1
In general, patterns of PCa recurrence include (1) localized recurrent disease only; (2) distant metastatic disease only (typically nodal, less commonly osseous); and (3) a combination of these. Nomograms have been developed to predict the site of recurrence, which can be useful to guide decisions regarding imaging examinations performed and treatment selection. Overall, after RP, recurrent disease is most common in the prostate fossa (local recurrence), followed by pelvic and retroperitoneal lymph nodes, with skeletal metastases being much less common. 8, 9 Other distant sites of recurrence are even less common and include mediastinal and cervical lymph nodes as well as distant solid-organ metastases. A subset of patients with “oligometastatic” disease has recently been recognized, in part due to the use of specific PET imaging radiotracers such as C-11 choline, probably representing a state of lower progressive potential. 10 Such patients were previously undiagnosed until developing more widespread end-stage disease. Both locally recurrent and distant metastases can be seen concurrently, most often in patients that are not imaged until their PSA is relatively high. Risk of progression to metastatic disease is higher when there is a short disease-free interval (< 24 months), whereas local recurrence is more common with a late BCR. 11 Mild PSA elevations often represent local recurrence, while higher PSA values, short doubling times (< 6 months), and high PSA velocities often represent distant metastasis. 11 Positive surgical margins increase the risk of both local recurrence and distant disease. Finally, patients with a Gleason score 8 to 10 or tumor stage pT3b (extraprostatic extension) or pTx pN1 at RP have an increased risk of systemic failure with distant metastasis and PCa-related mortality. In comparison, those with a Gleason score < 7 or tumor stage pT3a (seminal vesical invasion) pN0 or pTx R1 (R1 = positive margin) more likely have a local recurrence. 12
Traditionally, high-risk patients with recurrent disease (rapidly rising PSA, Gleason score 8 to 10, and early BCR—see above) are treated with nontargeted salvage radiation therapy (sRT), hormonal androgen deprivation therapy (ADT), systemic chemotherapy, or a combination of these. These therapies may be considered blind treatment in that a specific site of recurrence has usually not been identified or, when it has, is not targeted specifically. This approach poses the potential for substantial treatment-related morbidity and may lack efficacy in halting the progression to advanced metastatic disease and PCa-related mortality. In particular, systemic ADT has demonstrated no proven mortality benefit in men with asymptomatic metastatic PCa 10 despite a number of potential side effects, and the European Association of Urology guidelines suggest postponing palliative ADT due to the lack of a clear survival benefit. 13 Additionally, salvage radiotherapy in patients with PSA > 2 ng/mL or with long PSA doubling times (> 6 months) had no proven benefit for PCa-specific survival when compared to active surveillance. 14 Ureteral and urethral strictures, cystitis, urinary and rectal incontinence, and perineal pain are all common complication of nontargeted radiation therapy. 15, 16 In addition, systemic androgen deprivation therapy has lifestyle-limiting side effects and recently has been associated with severe cardiovascular risks. 17 Given these considerations, surveillance may be deemed an appropriate alternative approach in select clinical settings.
As advanced imaging options improve and become more widely available, there is a movement towards targeted salvage treatment to specific sites of disease recurrence. Precise localization with imaging enables additional targeted treatment options that may achieve decreased patient morbidity in comparison with reliance on nontargeted systemic therapies. The current standard approach for salvage therapy following RP is nontargeted radiation to the pelvis. However this has reported failure rates as high as 42% in terms of providing adequate tumor control of local recurrences and is associated with many side effects as mentioned above. 18 On the other hand, although technically challenging, salvage prostatectomy may be an option for treating local recurrence following primary radiation therapy. 19 In addition, in patients with oligometastatic disease, which is a nonlocal recurrence identified at a single site, salvage surgical resection or image-guided ablation may be a viable option for curative intent, if not at least for delaying further progression. 20
Using the aforementioned nomograms, the most advantageous imaging modality can be chosen appropriately. Clinical symptoms such as bone pain also should be taken into consideration when imaging tests are ordered, (recognizing that bone metastases are very uncommon in patients that have a PSA under 10 ng/mL 21). It is important to recognize that salvage treatment options are most efficacious when the tumor burden is the lowest, as is the case when the serum PSA first becomes detectable. 14 Kitajima et al observed that 79 of 115 patients undergoing imaging at the time of BCR had only one site of recurrence, 70% of which were local, emphasizing the potential value of early imaging. 9 When advanced imaging fails to identify the site of recurrence at low PSA values, other conventional nontargeted treatment options may be considered (versus serial PSA follow-up and later repeat imaging). Several of these salvage treatment options, including image-guided therapies, are discussed in 8.10 Image-Guided Focal Treatments.
There are multiple imaging modality choices for the evaluation of BCR. The chosen imaging modality should reflect the expected location of recurrence (local versus distant metastasis) based on the consideration of patient-specific factors described above (timing and rate of PSA recurrence as well as symptoms). Nuclear medicine bone scintigraphy, computed tomography (CT), and fluorodeoxyglucose positron emission tomography–computed tomography (FDG PET/CT) have limited use for evaluation of new BCR. However, 11C-choline PET/CT has shown great potential for evaluation of suspected distant metastatic disease, and pelvic MRI, potentially with targeted biopsy of any lesions in the prostate bed, may be useful for suspected local recurrence.
Magnetic resonance imaging is the primary imaging examination for evaluating the prostate bed in the setting of BCR, both for identifying local recurrence, and for enabling focal treatment options. Therefore MRI will be addressed in detail in the subsequent section. The remainder of this section describes alternative imaging modalities that may be complimentary to MRI, acknowledging key limitations of these options.
Transrectal ultrasound (TRUS) is of limited value in assessing the prostate bed for local recurrence, having a reported low sensitivity ranging from 25 to 54%. 22, 23 One study showed a higher sensitivity (80%) in patients with a higher PSA of over 2 ng/mL, although only moderate specificity (67%), 24 likely owing to overlap of imaging characteristics for normal postoperative changes, fibrotic tissue, and recurrent disease. Typically, local recurrence is characterized by a hypoechoic nodule, most likely near the vesicourethral anastomosis. However, in up to 30% of recurrences, the recurrent nodule may be isoechoic to the surrounding tissue, making lesion localization difficult ( ▶ Fig. 8.1). Transrectal ultrasound-guided biopsy is considered the gold standard for confirming local recurrence, although it has a low diagnostic yield especially at low PSA levels (<1 ng/mL) and in the setting of small lesion size. Transrectal ultrasound-guided targeted biopsy of a suspected recurrent lesion in the prostatectomy bed that is initially detected using MRI achieves a greater diagnostic yield. 25
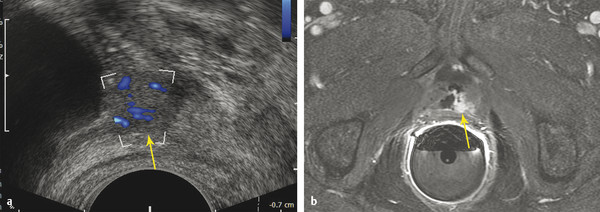
Fig. 8.1 Imaging of recurrent prostate carcinoma in a 70-year-old man with a history of robot-assisted prostatectomy and biochemical recurrence prostate-specific antigen = 1.2 ng/mL). (a) Transrectal ultrasound with Doppler demonstrates a 1.2-cm rounded hypoechoic nodule with hypervascularity near the bladder neck (arrow). Transrectal ultrasound has low tissue and spatial resolution, making recurrence difficult to differentiate from normal postoperative changes. (b) At subsequent MRI, dynamic contrast-enhanced images confirm an abnormal focal hyperenhancing nodule (arrow), consistent with local recurrence along the left side of the vesicourethral anastomosis. The patient subsequently underwent salvage radiation resulting in an undetectable PSA.
Computed tomography is widely available although it lacks sensitivity for evaluation of early BCR ( ▶ Fig. 8.2). 21, 22 In particular, CT has a minimal role in detecting local recurrence, only reliably identifying very large lesions measuring > 2 cm. 26 Computed tomography also has limited accuracy for diagnosing metastatic lymph nodes given its general reliance on nodal size, achieving a sensitivity of 27 to 75%, depending on the diagnostic criteria applied. For instance, if evaluating for metastatic lymph nodes based on a nodal diameter of over 1 cm, both poor sensitivity and specificity are achieved. Computed tomography is also suboptimal for skeletal metastases given low sensitivity for nonsclerotic lesions. In addition, CT is unreliable at assessing the response of sclerotic metastases to treatment given that such metastases often remain sclerotic despite adequate treatment response. Currently, the National Comprehensive Cancer Network guidelines suggest CT “may be considered” after RP when either the PSA fails to fall to an undetectable level (potentially representing undiagnosed presurgical metastatic disease) or, despite the above limitations, in the setting of BCR. Computed tomography may be most appropriate in the setting of advanced recurrent PCa, for instance, to monitor response of known metastatic lymphadenopathy or solid-organ metastases to androgen-deprivation therapy and/or chemotherapy ( ▶ Fig. 8.3).
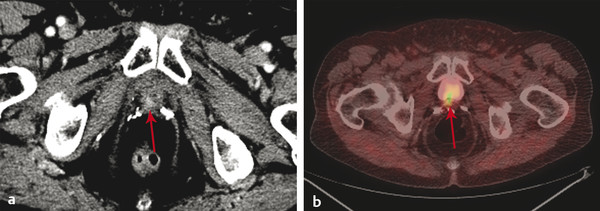
Fig. 8.2 An 86-year-old man with a history of Gleason score 3+4 stage pT3b, N0, M0 prostate cancer with a remote history of radical prostatectomy and salvage radiation therapy for a previous recurrence. His prostate-specific antigen has recently risen from an undetectable level to 2.0 ng/mL. (a) Contrast-enhanced CT images at narrow window settings shows a focus of enhancement at the right posterolateral vesicourethral anastomosis (arrow), considered highly suspicious for recurrence. No metastatic disease was identified. (b) Fused 11C-choline PET/CT image confirms a choline-avid focus corresponding to the CT finding (arrow).

Fig. 8.3 A 78-year-old man who underwent radical prostectomy 10 years previously, with subsequent salvage radiation for biochemical recurrence and more recent repeat relapse (prostate-specific antigen increasing rapidly to 42 ng/mL while on androgen-deprivation therapy). (a) Coronal CT image obtained at baseline prior to chemotherapy shows extensive metastatic retroperitoneal lymphadenopathy. (b) Coronal CT image obtained at follow-up shows partial response of the lymphadenopathy, although overall it shows progressive disease with extensive new hepatic metastases (arrows). Patient expired 1 week following the CT.
Bone scintigraphy also has low positive predictive value and sensitivity, especially in patients with PSA < 10 ng/mL. While Kane et al suggested a threshold PSA value of 10 ng/mL before bone metastases may be detected on a bone scan, 21 others have found that up to 34% of patients can have a positive bone scan with PSA values less than 10 ng/mL. 11 It should be noted, however, that average PSA values at the time of positive bone scans in these studies were 63 ng/mL and 123 ng/mL, respectively. 11, 21 For that reason American Urological Association (AUA) and NCCN guidelines suggest that the routine use of bone scintigraphy in the evaluation of BCR is not justified, but rather it should be reserved for follow-up of known skeletal metastases or in a patient with new bone pain and greatly elevated PSA (at least > 10 ng/mL). 27 While limited data suggests that 18F-NaF PET/CT may be able to detect otherwise occult osseous metastases including at lower PSA levels than typically diagnosed, the role of this examination in standardized diagnostic algorithms for BCR remains to be defined. 28
18F-FDG PET/CT is the mainstay of PET imaging for many other cancers, although it has limited value in evaluation of BCR likely owing to the low cellular proliferation and glucose metabolism of PCa cells. 18F-FDG PET/CT has particularly low sensitivity for evaluation of local recurrence in the prostate bed given urinary excretion and physiologic concentration of the radiotracer in the urinary bladder. Therefore, PET/CT is not recommended and has no significant clinical application in this setting (ACR appropriateness rating of 3). 29 18F-NaF PET/CT has been shown to be more sensitive than a conventional bone scan in depicting osseous metastases in PCa.
11C-choline is the only FDA approved PET/CT radio tracer for evaluation of BCR in the United States and has shown overall excellent performance in this application when considering detection of both local and distant metastases using a single imaging examination. 11C-choline has minimal background localization in the pelvis, thereby achieving very high specificity for PCa recurrence nearing 100%. 9 Nonetheless, 11C-choline PET/CT has limited spatial resolution, and urinary excretion may occasionally confound interpretation along the bladder neck. These factors diminish sensitivity for local recurrence. Thus, although potentially considered adequate for local recurrence, 11C-choline PET/CT is inferior to MRI for this purpose. On the other hand, 11C-choline shows the best performance among FDA-approved tests for detecting metastatic lymph nodes, including nodes as small as 5 mm, with an overall sensitivity of 83 to 100% 9( ▶ Fig. 8.4). As expected, lesion detection improves with increasing PSA and with increasing primary tumor Gleason score. 9 Also, given its whole body assessment, 11C-choline PET/CT can detect metastatic lesions above the pelvis, which are not routinely imaged using MRI. Some studies have shown an optimal threshold PSA level of 2 ng/mL for lesion detection. For example, Krause et al observed a diagnostic accuracy of 36% at PSA levels < 1 ng/mL, compared with 73% at PSA > 3 ng/mL. 22 Also as previously mentioned, 11C-choline PET/CT is helping to define a previously unrecognized population of patients with only a distant solitary focus of metastatic disease, termed oligometastatic. Logistically, use of 11C-choline is limited by its short half-life (20.4 min), thus necessitating a local cyclotron for production of the radiotracer.
Radiographic bone surveys and Indium-111 capromab pendetide (ProstaScint) scans have very poor performance in the setting of BCR, and their use is generally not warranted, receiving ACR appropriateness ratings of 1 and 3, respectively. 29
8.3 MRI for Evaluation of Biochemical Recurrence
The primary focus of this chapter is the imaging characteristics of recurrent PCa using MRI after failed primary treatment, including RP and radiation therapy. Multiparametric MRI(mpMRI) at 3 T using an endorectal coil may arguably be considered the gold standard for detection and delineation of local recurrence in the prostate fossa. MRI’s role in detecting local recurrence is important given that most recurrences occur locally in the prostate bed, especially with lower PSA levels and a relatively late time to recurrence. For detecting local recurrences, MRI is superior to TRUS as well as to all other imaging modalities including 11C-choline PET/CT, achieving a sensitivity of 83 to 95% (versus 45 to 75% for 11C-choline PET/CT) at PSA levels greater than 0.6 ng/mL. 25 In addition to detecting recurrent lesions, MRI is able to define the postsurgical pelvic anatomy and the overall extent of a recurrent lesion, which are important factors for focal treatment planning.
MRI has shown overall similar performance for detecting pelvic osseous metastases as 11C-choline PET/CT (sensitivity 87% vs. 81%, respectively). 9 Nonetheless, MRI and 11C-choline PET/CT could potentially play complimentary roles for this purpose, with each potentially detecting osseous metastases missed by the other test. The relative performance of the two examinations for osseous metastases may be influenced by treatment history, such as concurrent ADT or recent radiation therapy (RT).
The accuracy of MRI for nodal metastases (sensitivity 64%, accuracy 70%) 9 is mildly improved compared with CT, although still largely limited by reliance on conventional size criteria. This limited accuracy in diagnosing nodal metastases remains a primary weakness of MRI in the setting of PCa recurrence. 9 As previously noted, choline > PET/CT has shown significantly improved performance for evaluation of small lymph nodes (see ▶ Fig. 8.4). MR lymphography is a highly promising investigational technique with the potential for markedly improved performance in lymph node staging accuracy, including for very small nodes. Indeed, MR lymphography may outperform specific PET radiotracers due to improved spatial resolution. 30 While further investigation is required, the agent providing the best performance for MR lymphography in initial studies is not currently FDA approved for use in the United States.
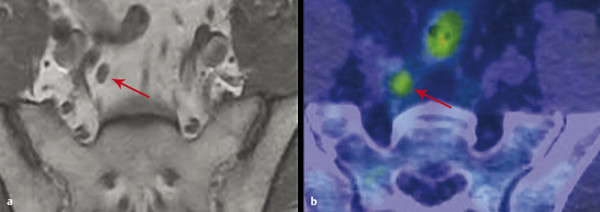
Fig. 8.4 Comparison of imaging modalities for pelvic lymph node recurrence. A 54-year-old man presented with a prostate-specific antigen level of 2.7 ng/mL 2.5 years after radical prostatectomy for prostate carcinoma with salvage external-beam radiation therapy to the surgical bed. (a) Axial T1-weighted MR image demonstrates a 0.5 cm x 0.7 cm lymph node in the right internal iliac chain (arrow), which was considered normal by size criteria. (b) 11C-choline PET/CT image demonstrates corresponding significant choline avidity of this small node (arrow) with the maximum standardized uptake value of 3.8. This node was confirmed to be a metastasis by extended bilateral pelvic node dissection.
In summary, MRI is the primary examination for evaluation of local tumor recurrence, and has reasonable performance for detecting osseous metastases (although these are relatively uncommon as an initial site of BCR). The main weakness of MRI is poor accuracy for lymph node metastases. 11C-choline PET shows the best performance for lymph node staging among currently available FDA-approved imaging approaches, although its weakness is local recurrence evaluation. In combination, these two examinations offer excellent synergy in the work-up of BCR ( ▶ Table 8.1; ▶ Fig. 8.5). However, the most cost-effective sequence for performing these two examinations is yet to be determined.
Sensitivity | Specificity | Accuracy | AUC | ||
(95% CI) | (95% CI) | (95% CI) | (95% CI) | ||
Local recurrence | |||||
MRI | 88.5%a | 84.6% | 87.4%a | 0.91a | |
(78.2%, 94.3%) | (66.5%, 93.8%) | (78.8%, 92.8%) | (0.85, 0.97) | ||
11C-choline PET/CT | 54.1% | 92.3% | 65.5% | 0.76 | |
(41.7%, 66.0%) | (75.9%, 97.9%) | (55.1%, 74.7%) | (0.67, 0.85) | ||
Pelvic lymph node metastasis (n = 70) | |||||
MRI | 64.0% | 85.0% | 70.0% | 0.81 | |
(50.1%, 75.9%) | (64.0%, 94.8%) | (58.5%, 79.5%) | (0.71, 0.91) | ||
11C-choline PET/CT | 90.0%a | 100.0% | 92.9%a | 0.95a | |
(78.6%, 95.7%) | (83.9%, 100%) | (84.3%, 96.9%) | (0.91, 1.00) | ||
Pelvic bone metastasis (n = 95) | |||||
MRI | 87.5% | 96.2% | 94.7% | 0.93 | |
(64.0%, 96.5%) | (89.4%, 98.7%) | (88.3%, 97.7%) | (0.84, 1.00) | ||
11C-choline PET/CT | 81.3% | 98.7% | 95.8% | 0.90 | |
(57.0%, 93.4%) | (93.2%, 99.8%) | (89.7%, 98.4%) | (0.80, 1.00) | ||
Abbreviations: AUC, area under receiver operating characteristic curve; CI, confidence interval; n, number. | |||||
aA statistically significant difference between MRI and 11C-choline PET/CT (p < 0.05). Source: Data from Kitajama et al 2015 9. | |||||
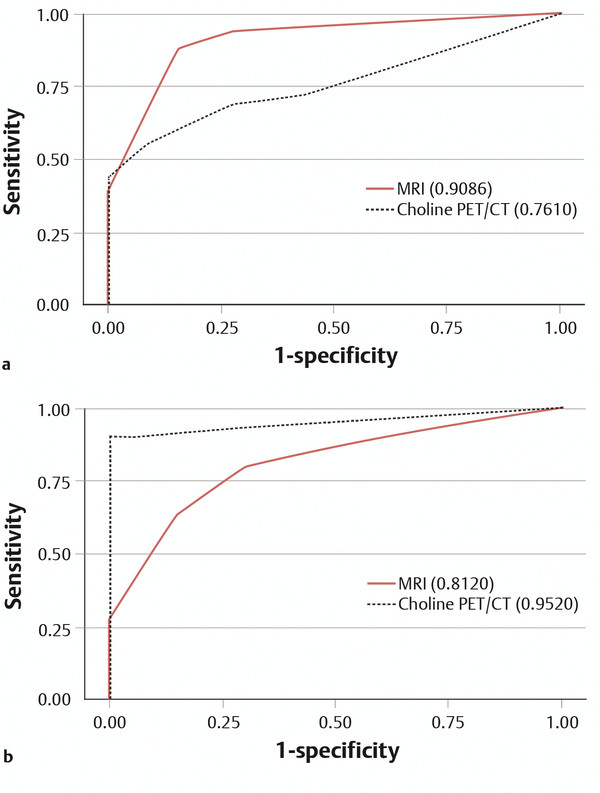
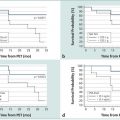
Fig. 8.5 Receiver operating characteristic (ROC) curves for MRI (solid red line) and 11C-choline PET/CT (dashed black line) in (a) evaluation for local recurrence (area under curve [AUC] of 0.91 for MRI and 0.76 for PET/CT [p < 0.05]) and in (b) evaluation for pelvic lymph node metastases (AUC of 0.81 for MRI and 0.95 for PET/CT [p < 0. 05]).
8.4 Post–Radical Prostectomy Anatomy
Understanding the postoperative appearance of the pelvis is critical for the evaluation of BCR. Following RP, the bladder base descends inferiorly and the levator ani muscle complex shifts anteriorly and inferiorly, partially occupying the prostatectomy bed, while the bladder takes on an inverted pear shape. These findings are best visualized in the coronal and sagittal imaging planes ( ▶ Fig. 8.6). The location of the urogenital diaphragm is typically unaffected. In the absence of recurrent disease, the prostatectomy bed typically contains only fat, minimal scar tissue, and vasculature. There may be linear low T1 and T2 signal in the anterior rectal wall related to postoperative fibrosis as well as linear fibrosis of Denonvilliers’ (rectoprostatic) fascia. A small-to-moderate amount of non-masslike low signal may occur at the site of the anastomosis of the urethra and bladder (vesicourethral anastomosis) due to normal postsurgical fibrosis. This finding is typically most prominent along the anterior aspect of the anastomosis and may result in indentation of the bladder wall. 31 Partial dehiscence of the vesicourethral anastomosis may be clinically inapparent and appears as a focal irregularly widened space or a focal outpouching (or pseudodiverticulum) between the bladder neck and membranous urethra, which in the chronic setting is very rarely of any clinical consequence.
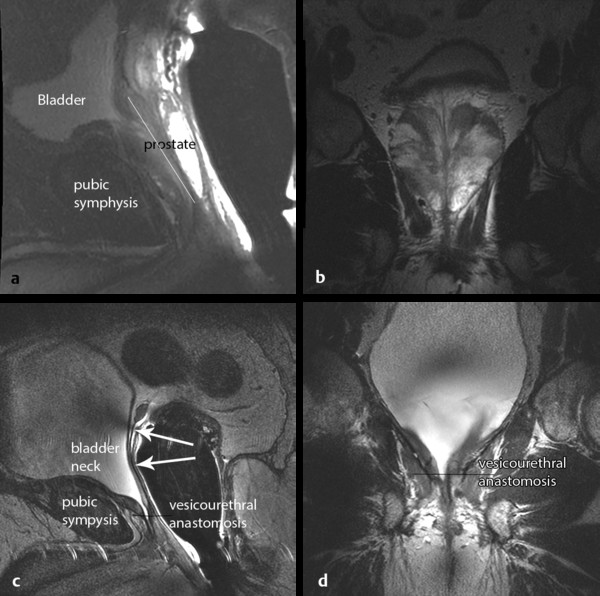
Fig. 8.6 (a) Sagittal and (b) coronal T2-weighted MRI of the prostate in a patient with biopsy-proven prostate carcinoma. (c) Sagittal and (d) coronal T2-weighted images of the pelvis in the same patient following radical prostatectomy, showing alterations in the anatomy. The bladder neck becomes elongated and tapered with the vesicourethral anastomosis near the level of the low pubic symphysis (noted on d). There is a fine linear scar typically visualized along the resection plane (c, arrows), with a small amount of scarring in the seminal vesicle beds at the superior aspect. The anus and rectum are shifted more anteriorly. (An endorectal coil is in place at both time points.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree