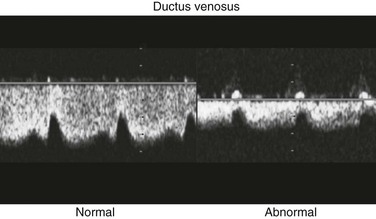
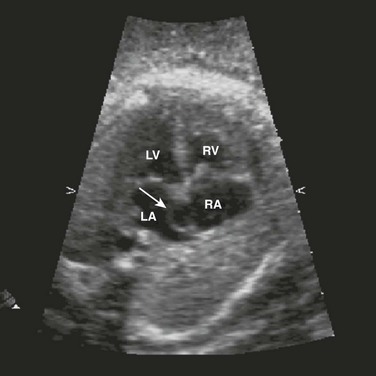
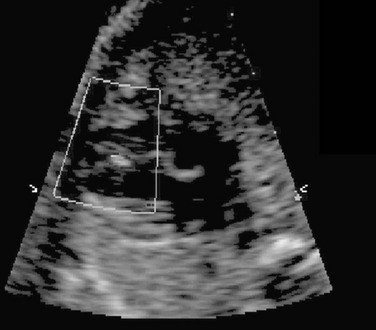
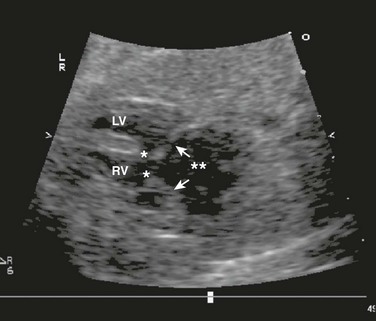
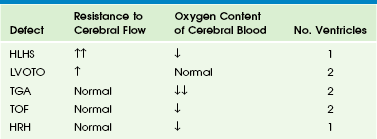
Chapter 71 Congenital heart disease, the most common birth defect, occurs in 3 to 8 per 1000 newborns.1–3 The incidence is higher prenatally, affecting 5.8% to 16.9% of fetuses undergoing screening echocardiograms.4–6 Despite advances in imaging techniques, routine obstetric ultrasound is only 30% to 50% sensitive for detection of congenital heart defects.7–12 With the addition of careful delineation of outflow tracts, sensitivity improves significantly.13 The most difficult lesions to diagnose prenatally are transposition of the great arteries and outflow tract abnormalities. A complete fetal echocardiogram includes two-dimensional, M-mode, and color Doppler imaging to assess fetal cardiac structure, rhythm, and function. Novel techniques include tissue Doppler and strain analysis. The fetal cardiac circulation has been studied in human and animal models (Fig. 71-1). Fetal and postnatal cardiovascular physiology differs markedly. Key differences include the following: Figure 71-1 Diagram of the normal fetal cardiac circulation. 1. Right ventricular output is greater than left ventricular output. 2. Oxygen saturation of blood to the brain is higher than of blood to the body because maternal blood is directed from the umbilical vein to the ductus venosus and across the foramen ovale by the eustachian valve. 3. A ductus arteriosus is present. Deoxygenated blood from the superior vena cava travels to the right ventricle to the ductus arteriosus and then to the placenta. 4. Pulmonary vascular resistance is increased, resulting in decreased flow to the lungs. This changes after birth to allow an increase in pulmonary blood flow. 5. In utero, afterload for the left ventricle decreases but increases dramatically with umbilical cord clamping. Fetal cerebral vessels can vasodilate during stress, which decreases resistance and increases diastolic flow in the middle cerebral artery. Peripheral vessels vasoconstrict to direct blood to the brain; this causes increased resistance and decreased diastolic flow in the descending aorta. This represents an autoregulatory mechanism (Fig. 71-2). This phenomenon of increasing cerebral blood flow has been described in growth-restricted fetuses as a predictor of poor perinatal outcome (Fig. 71-3). This phenomenon also occurs in fetuses with congenital heart disease (Table 71-1), although the clinical significance of this finding as a predictor of outcome is still in question.14 Table 71-1 Figure 71-2 Normal and abnormal arterial spectral Doppler signals from the umbilical and middle cerebral arteries. Flow patterns in the umbilical vein and ductus venosus can be used to assess right ventricular filling. Impaired relaxation, associated with placental insufficiency or cardiac dysfunction, can cause decreased or reversed diastolic venous flow, particularly in atrial systole (Fig. 71-4). Absent or reversed flow in the ductus venosus and pulsatility of the umbilical vein flow associated with elevated atrial pressure have been recognized as markers of poor outcome in hydropic fetuses. The relationship of the aorta and pulmonary outflow to the ventricles should be determined, and peak velocities in aortic and ductal arches should be obtained. Arch sidedness can be determined from the three-vessel view. The aorta, main pulmonary artery, and the SVC are seen relative to the trachea (Fig. 71-5) An aorta positioned right of the trachea suggests a right aortic arch and calls for careful evaluation for vascular rings and congenital heart disease. Fetal echocardiography has been in use since the late 1980s. The optimal time for transabdominal imaging of the fetal heart is between 20 and 28 weeks of gestation. Transvaginal imaging can be performed as early as 8 weeks, with successful diagnosis of heart defects possible as early as 11 weeks.15–16 Third-trimester imaging, although possible, is limited by paucity of the amniotic fluid and limited variability in fetal position. Indications for fetal echocardiography include maternal and fetal risk factors (Box 71-1). The most common reasons are family history of congenital heart disease, fetal dysrhythmia, maternal diabetes, and extracardiac defects. Indications that are most predictive of cardiac disease are an abnormal four-chamber view on routine ultrasound (30% to 50%), fetal dysrhythmia (30%), hydrops (30%), and polyhydramnios (25%). The most common atrial septal defects (ASDs) are ostium secundum defects. Sinus venosus defects (superior or inferior type) are often associated with anomalous drainage of the right pulmonary veins. Ostium primum defects are an endocardial cushion defect, and often associated with Down syndrome. A patent foramen ovale is a normal structure of the fetus and newborn (Figs. 71-6 and 71-7); it may be difficult to distinguish a normal foramen ovale from a secundum ASD prenatally. Secundum defects are amenable to catheter closure; other defects require surgical correction. Ventricular septal defects (VSDs) are the most common type of congenital heart defect. They can occur in the membranous, AV canal, muscular, or conal (outlet) septum. Perimembranous (around the membranous septum) defects are the most common. Moderate to large defects require surgical intervention in infants with congestive heart failure; small defects often close on their own. Muscular defects are the second most common; small defects usually close on their own, but multiple defects can cause congestive heart failure (Fig. 71-8). AV canal (endocardial cushion) defects are easily diagnosed prenatally (Fig. 71-9) and can be associated with Down syndrome. They include a primum ASD, inlet VSD, and common AV valve. VSDs can be isolated. The cross-sectional anatomy of the common valve is best determined from short-axis imaging. Partial AV septal defects have a primum ASD with a cleft mitral valve. Transitional AV septal defects have an atrial defect, common AV valve, and restrictive VSD.
Prenatal Imaging and Therapy of Congenital Heart Disease
Fetal Physiology and Flow
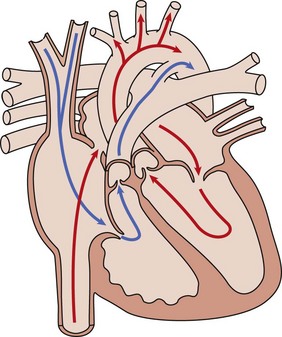
Oxygenated umbilical venous blood enters the right atrium from the inferior vena cava and is directed across a patent foramen ovale. into the left atrium, from which it enters the fetal systemic circulation. Unoxygenated fetal systemic venous blood enters the right atrium via the superior vena cava. This blood is directed into the right ventricle and then out into the main pulmonary artery. High pulmonary vascular resistance and a patent ductus arteriosus causes preferential flow into the descending aorta.
Cerebral Resistance
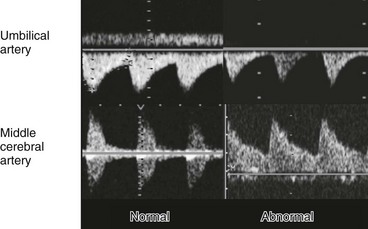
Fetal compromise results in increased peripheral and placental resistance (decreased diastolic flow in umbilical artery) and decreased cerebral resistance (increased diastolic flow in middle cerebral artery); this is known as the brain-sparing effect.
Venous Flow Patterns
Fetal Anatomy
Aortic and Ductal Arches
Prenatal Imaging: Timing and Indications
Cardiac Defects
Atrial Septal Defects
Ventricular Septal Defects
Atrioventricular Canal defects
Prenatal Imaging and Therapy of Congenital Heart Disease