Fig. 10.1
A 3-year-old girl who underwent liver transplantation for mixed hepatoblastoma. PET evaluation following increased serum alpha-fetoprotein. Maximal intensity projection (a), axial CT (b, d), and PET/CT (c, e) fusion images show the FDG-avid peritoneal lesions
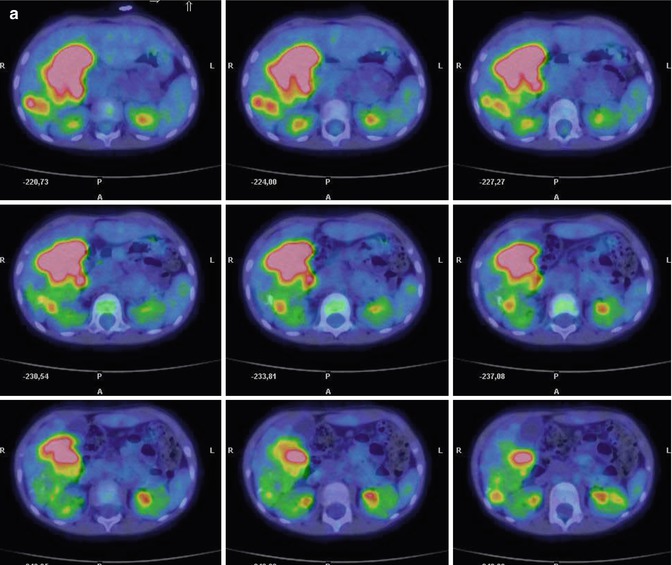
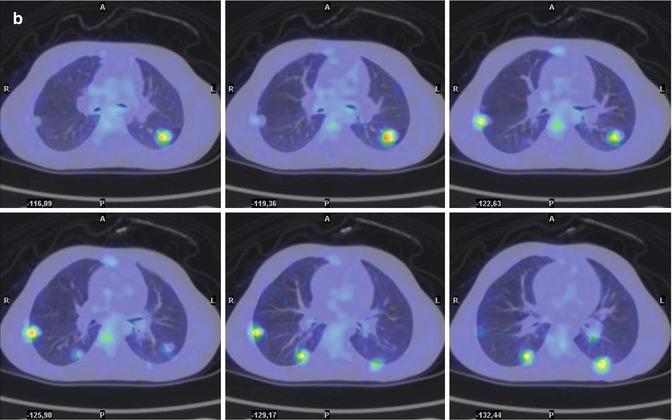
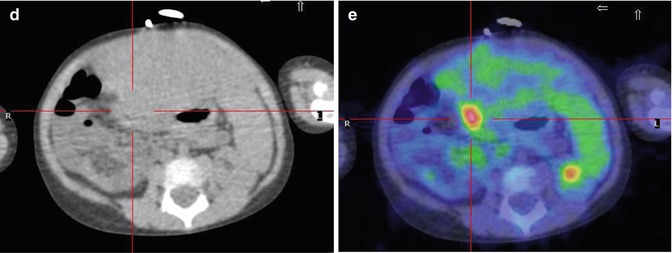
Fig. 10.2
A 4-year-old boy with hepatoblastoma. PET evaluation to determine liver transplantation eligibility. Axial PET/CT fusion images show FDG-avid lesions in the liver (a) and lungs (b). The patient was referred for chemotherapy
10.2 Hepatocarcinoma
As the second most common malignant liver tumor in childhood, HCC comprises 35 % of all hepatic malignancies in children [22]. HCC is histologically divided into classical and fibrolamellar types. Fibrolamellar HCC is the most frequent histological variation and is commonly observed in children and adolescents [23]. Conditions associated with a high risk for HCC development are α-1-antitrypsin deficiency, Wilson’s disease, hemochromatosis, hereditary tyrosinemia, Fanconi’s anemia, familial adenomatous polyposis and Gardener’s syndrome [1]. As in HB, α-FP is increased in HCC in the majority of patients [24]. Since the tumor is chemoresistant, surgical resection and liver transplantation (in case of unresectable HCC confined to the liver) are the only therapeutic options [25]. At diagnosis, 50 % of patients present with metastases [26], mostly in the lungs (31 %). Extrahepatic tumor extension and vascular invasion are also frequently seen (39 %) [27]. The US echogenicity of HCC is similar to that of the liver, and the CT characteristics are highly variable, either homogeneous or heterogeneous, solitary or multifocal, and well- or ill defined. While in adults the presence of underlying cirrhosis may help in the differential diagnosis, it is rare in the pediatric population [28]. CT is generally used to evaluate the response to treatment, but it cannot be used to estimate tumor viability (Fig. 10.3).
Several articles on the impact of PET/CT in adult HCC have been published, but there are no reports on the use of this imaging technique in pediatric patients. Lee et al. evaluated 138 adult patients with low-grade or high-grade HCC, either newly diagnosed or reevaluated after treatment (tumor resection, transcatheter arterial chemoembolization, radiofrequency ablation, systemic chemotherapy), who underwent 18F-FDG–PET/CT or conventional imaging modalities [29]. The detection rate for lung metastases by 18F-FDG–PET/CT was lower than that obtained with CT, and for lesions below 1 cm, it diminished dramatically, probably because of the limited resolution. In the detection of lymph node lesions, by contrast, there were no differences between CT and 18F-FDG–PET/CT. Moreover, 18F-FDG–PET/CT was significantly superior to bone scan in patients with bone metastases, depicting all bone lesions [29].
Talbot et al. [30] compared 18F-FDG with 18F-fluorocholine in the detection and staging of HCC in patients with chronic liver disease and suspected liver nodules. FDG was shown to be significantly more sensitive, especially in the detection of well-differentiated tumors. Although 18F-FDG was unable to demonstrate focal nodular hyperplasia, it was more sensitive than 18F-fluorocholine for other malignancies. Consequently, the authors suggested performing PET/CT with both radiopharmaceuticals as the best option [30]. Another study proposed the use of FDG–PET/CT in the assessment of tumor response and tumor viability after interventional therapy (transcatheter arterial chemoembolization) but further investigations on the benefits of this application are warranted [31].
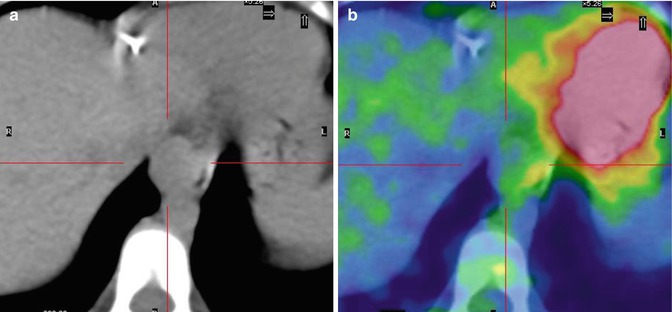
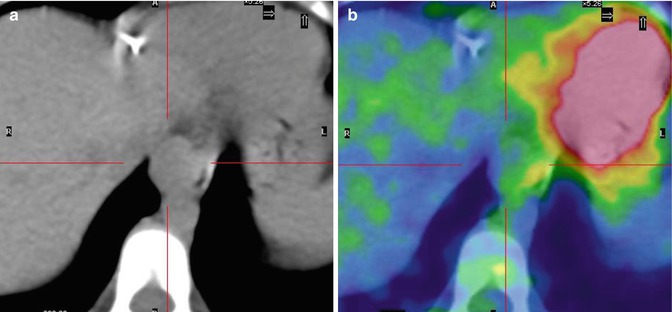
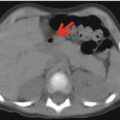
Fig. 10.3
An 8-year-old boy treated for hepatoblastoma. PET evaluation following increased alpha-fetoprotein levels. Axial CT (a) and CT/PET fusion (b) images show no FDG uptake in a small cardiac lesion seen on CT. The patient underwent surgery; the histological finding was hepatocarcinoma
10.3 Undifferentiated Sarcoma of the Liver
Undifferentiated sarcoma of the liver is the third most frequently occurring hepatic malignancy of childhood. Unlike HB and HCC, in this rapidly growing tumor [2], α-FP levels are usually normal and thus are of no diagnostic relevance. On US but also on CT and MRI, USLs are generally large and solid in appearance. While FDG–PET has been suggested as a valuable method in the evaluation of USL patients during postoperative chemotherapy, it has yet to be confirmed in the literature (Figs. 10.4 and 10.5) [32]. The treatment of choice is chemotherapy followed by resection. Preferential sites of metastases are the lungs and bones [33].
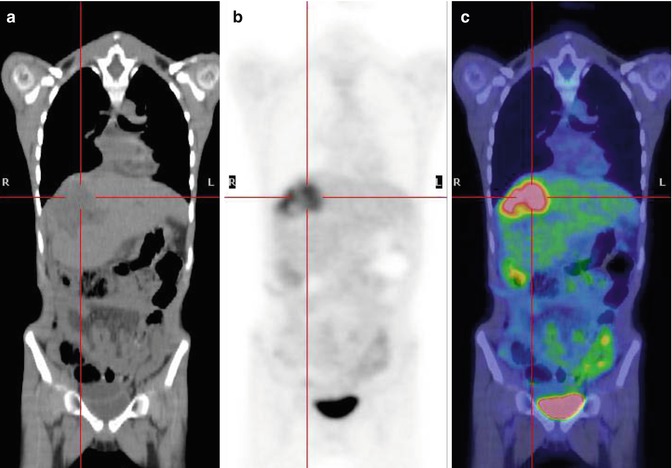
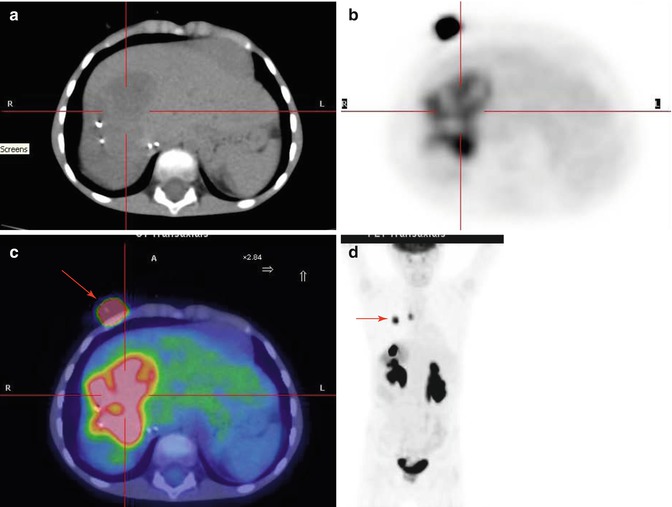
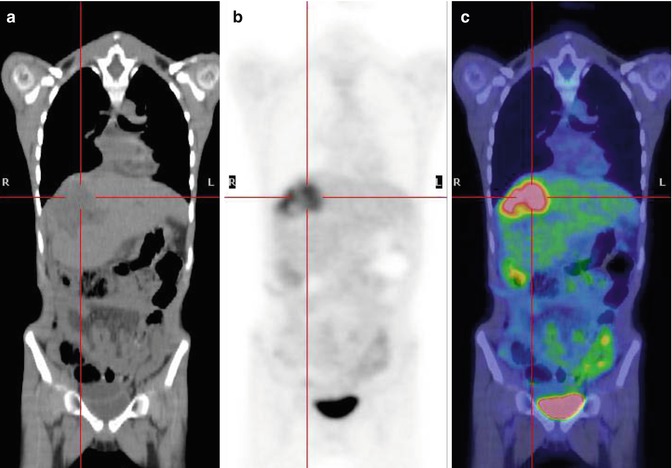
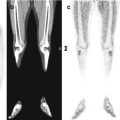
Fig. 10.4
An 8-year-old boy treated for sarcoma of the liver. Coronal CT (a), PET (b), and PET/CT fusion (c) images show a large FDG-avid lesion of the right hepatic lobe, corresponding to disease recurrence
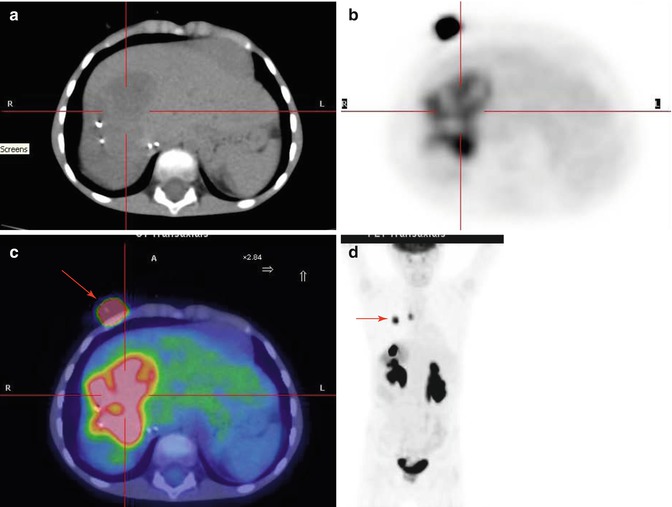
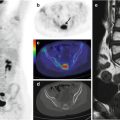
Fig. 10.5
(a–c) Axial images of the same patient as in Fig. 10.4. The lesion involves almost the entire right lobe of the liver. (d) Maximal intensity projection shows two other areas of focal uptake, in the right lung and mediastinum (red arrow). On axial images, these areas correspond to tracer stasis in the catheter reservoir of the central venous line (red arrow in c)
10.4 Carcinoid
Derived from neuroendocrine cells, carcinoid tumors spread throughout the body, especially to the liver (Fig. 10.6), and often produce functional peptide hormones. Approximately 56 % arise in the gastrointestinal tract followed by the lungs (30.1 %), pancreas (2.3 %), reproductive system (1.2 %), biliary tract (1.1 %), and head and neck (0.4 %). Primary hepatic carcinoid tumors (PHCT) are extremely rare [34]. Neither CT, nor MRI is advantageous in the imaging of neuroendocrine tumors (NETs), which are generally better detected by OctreoScan scintigraphy [35]. Recent data indicated that higher quality images obtained with a shorter acquisition protocol are possible with 68Ga-DOTA-NOC PET/CT than with 111In-DTPA-octreotide [36]. 18F-FDG–PET may be useful for identifying NETs characterized by rapid growth or aggressive behavior, with increased tumor uptake of the FDG tracer indicative of a worse prognosis. Although NETs with multiple tumor sites show broad-ranging heterogeneity in tracer uptake, FDG–PET may be able to detect unsuspected distant metastases, contributing to better staging of advanced disease [37].
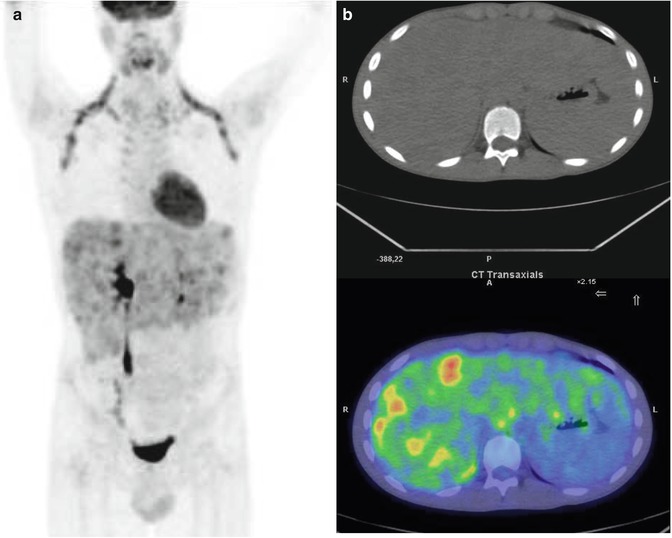
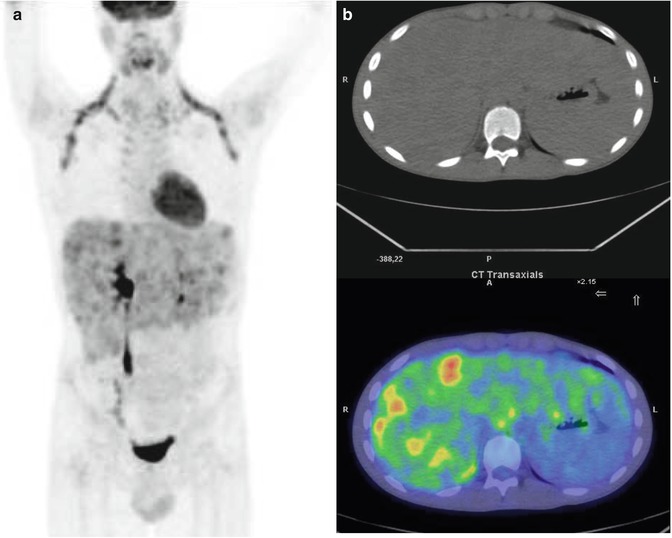
Fig. 10.6
A 7-year-old boy operated on for carcinoid of the terminal ileum. Maximal intensity projection (a) and axial and PET/CT fusion images (b) show multiple nonhomogeneous 18F-FDG uptake in the right lobe of the liver, corresponding to hepatic metastasis. In (a), note the FDG uptake by brown fat in the laterocervical, supraclavicular, and axillary regions
References
1.
Agarwala S (2012) Primary malignant liver tumors in children. Indian J Pediatr 79:793–800PubMedCrossRef
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree