Fig. 42.1
Vascularized fibula grafting
42.2.4 Vascularized Iliac Bone Grafting
Vascularized iliac crest bone grafts is one of the many vascularized procedures used in osteonecrosis of the femoral head for restoration of blood supply [18, 19].
42.2.4.1 Surgical Technique
After an incision made along the iliac crest and downward, it is important to identify, dissect, and ligate the first few tributaries of the deep circumflex iliac artery. A tricortical iliac bone graft is harvested, keeping its vascular pedicle intact. In addition, cortico-cancellous chips are also harvested from the iliac crest [20]. The joint capsule is then exposed by separating the interval between the sartorius and tensor fascia lata superficially, and the interval between the gluteus medius and the rectus femoralis underneath. An arthrotomy is made to expose the femoral neck. With a high-speed burr, under direct vision, the necrotic bone is excised from the anterior aspect of the head–neck junction. The vascularized graft with its pedicle is then mobilized and fixed to the femoral neck after the defect is packed with cancellous bone graft.
42.3 Nonvascularized Bone Grafting
Nonvascularized bone grafting has been used because cancellous bone graft provides an osteoconductive and osteoinductive substrate for filling of voids left after decompressive procedures in the treatment of osteonecrosis of the femoral head. One of the limitations with nonvascularized bone grafting is that it fails to improve the vascularity of the recipient femoral head [12]. The three basic types of nonvascularized grafts used in ONFH are femoral neck grafting, cortical strut grafting, and grafting through the articular cartilage.
42.3.1 Femoral Neck Grafting (Light Bulb Procedure)
In the early pre-collapse stages of the disease, the necrotic region of the femoral head can be replaced with cancellous bone graft in an effort to aid healing of the lesion.
42.3.1.1 Surgical Technique
After the proximal femur is exposed, an approximate 1.0 by 1.5 cm bone window should be made at the femoral head–neck junction using osteotomes. Through the window previously created, a curette is used to create a cavity inside the femoral head and remove all of the necrotic bone found up to the sub-cartilage bone lamellae. Then measure the volume of the light bulb-shaped cavity using saline solution. The sclerotic bone should then be perforated using a power-assisted drill until bleeding bone is found. The next would be to obtain the bone graft which can typically be an auto-iliac-harvested bone (cortical and cancellous bone) combined with demineralized bone matrix. Subsequently, bone graft should be packed into layers to fill the light bulb-shaped cavity. At last the cortical segment previously removed should be replaced and fixed with one 3-mm absorbable pin [13]. See Figs. 42.2 and 42.3.
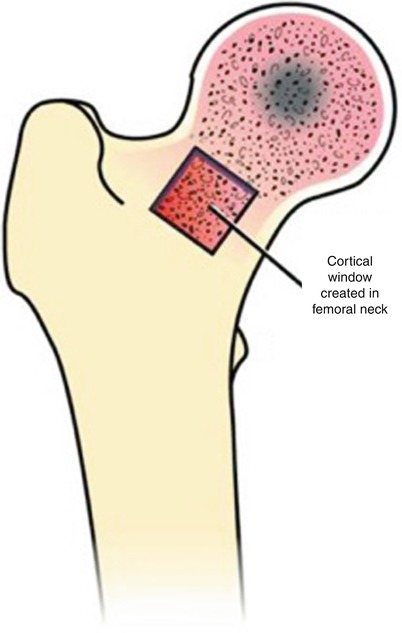
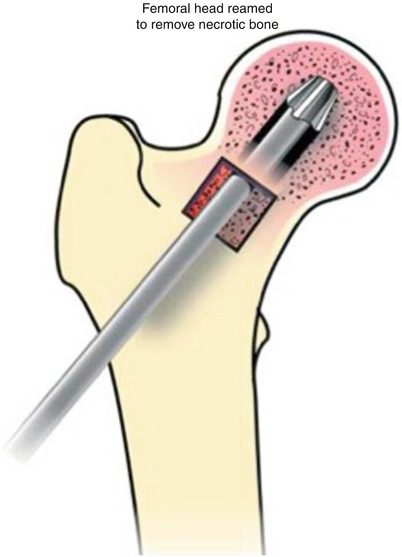
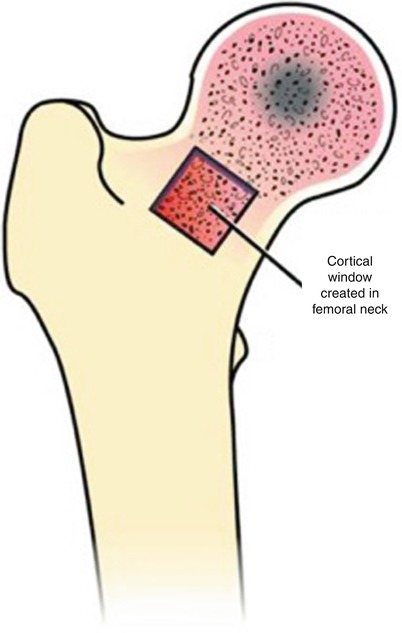
Fig. 42.2
Light bulb procedure
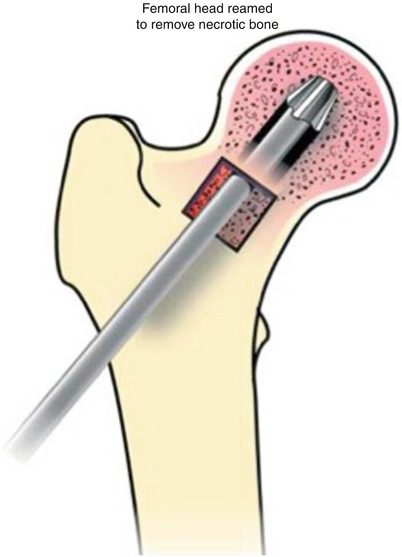
Fig. 42.3
Removal of necrotic bone during the light bulb procedure
42.3.2 Cortical Strut Grafting (Phemister)
Cortical strut grafting was first described by Phemister in 1949 [4] and is therefore commonly known as the Phemister procedure. It consists of drilling two cores of bone that will decompress the femoral head. The large surface area is presumed to act as conduit for blood vessels to grow and perfuse the femoral head. In addition, the bone grafts provide mechanical stability to prevent articular surface collapse [4].
42.3.2.1 Surgical Technique
After exposure of the greater trochanter and femoral neck, two 2-mm guide pins are inserted under fluoroscopic guidance with a power-assisted drill. The first pin is inserted below the vastus tubercle of the greater trochanter and directed toward the anterior superior half of the femoral head until it is placed in the subchondral bone. The second pin should be inserted 1.5–2 cm below the previous pin and should aim 1 cm below the level of the subchondral cortex. These pins are used as a guide to drill 4–5 cm with a 7- and then a 9-mm cannulated drill. This will prepare the outer portion of the channel. Subsequently, drilling is performed without the pins at low speeds with a Phemister trephine (using saline to avoid overheating) through the previous channels until the necrotic bone is taken out. The core tissue which is removed during the procedure should be sent for histopathological examination. The procedure should then be repeated in the inferior channel.
To obtain the graft, there should be an adequate exposure of the anteromedial part of the tibia, and the periosteum should be vertically stripped (approximately 13 mm wide). With a twin-oscillating saw, a 10-mm wide graft (kept cool with saline), which is long enough for both channels, should be used. The tibial bone grafts should be trimmed to remove excess cancellous bone from the posterior surface and to achieve the desired length. The exact length of the channels should be measured, and the graft should be cut to accurately fit the channel. The grafts are then inserted (so that the broad surface is in the coronal plane) and tapped until it gets to the subchondral plane [5, 21].
42.3.3 Grafting Through the Articular Cartilage (Trapdoor Procedure)
In advanced cases, or when the articular cartilage is compromised, bone grafting through a so-called trapdoor in the femoral head may be considered as an alternative procedure. The nonvascularized cortical and cancellous autografts, which replace the necrotic bone, may act as support for the subchondral bone and cartilage, as well as stimulating bone formation [3].
42.3.3.1 Surgical Technique
After an adequate exposure of the hip’s capsule is obtained, it is incised at the superior rim of the acetabulum and peeled back posteriorly and anteriorly, maintaining its blood supply. Then, dislocate the hip and expose the area of the segmental collapse. Using a scalpel and an osteotome, the edges of the necrotic segment are defined. The necrotic segment is then removed using osteotomes, curettage, and power burrs, until a bleeding surface and viable bone is encountered at the base of the cavity.
An iliac (the tibia can also be used) bone graft should be harvested consisting of cortico-cancellous struts and cancellous bone. Depending on the size of the lesion, two to three cortical struts should be placed (perpendicular) in the troughs previously made. The remaining space in the femoral head should be packed with cancellous bone graft which was previously harvested. After replacing the trapdoor, it should be fixed with two or three absorbable pins. The hip joint should then be reduced and the capsule should be sutured loosely [3]. See Figs. 42.4, 42.5, and 42.6.
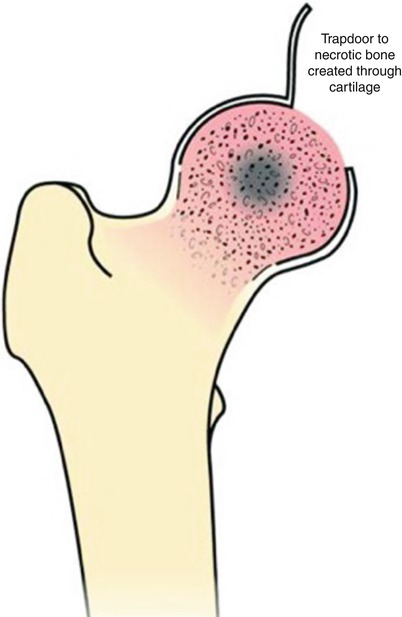
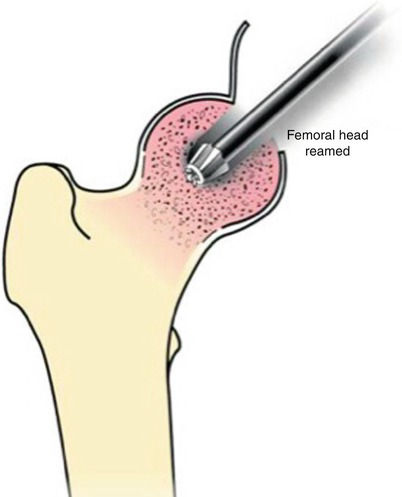
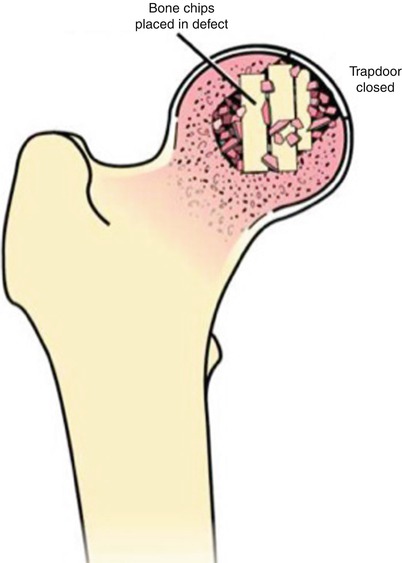
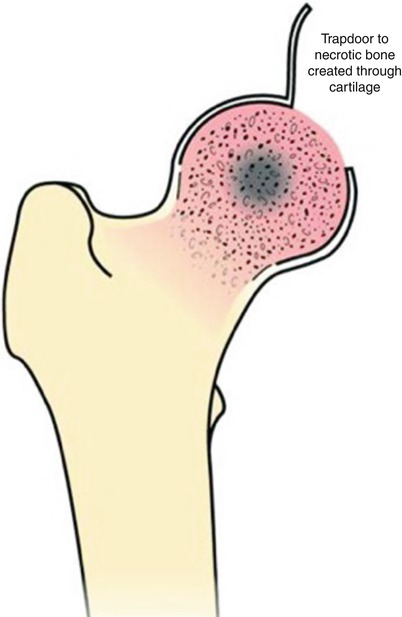
Fig. 42.4
Trapdoor procedure
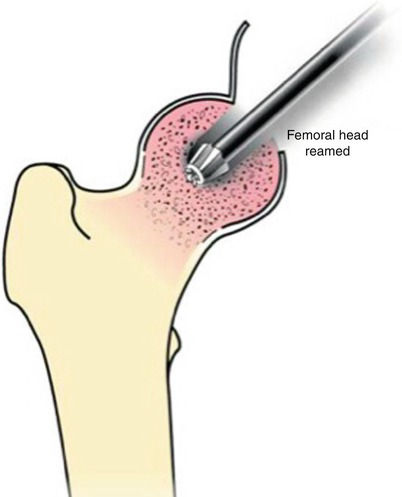
Fig. 42.5
Removal of necrotic tissue through the trapdoor
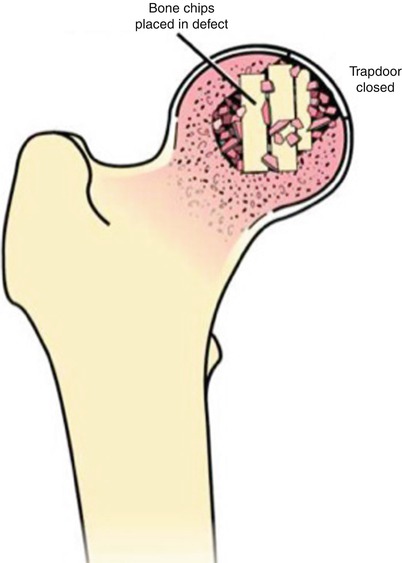
Fig. 42.6
Packing of the defect with bone grafts
42.4 Results of Vascularized Bone Grafting
Yoo et al. reported 89 % survivorship at a mean follow-up of 13.9 years (range, 10–23.7 years) in 124 hips with Ficat and Arlet stage II or III disease [22]. Similar results were reported in a study of 103 hips at a mean of 5 year follow-up by Urbanik et al. who observed 91 and 77 % survivorship in stage II and stage III hips, respectively [8]. Results by Edward et al. were in agreement with those reported by Urbanik and Yoo [23]. Following 65 pre-collapse osteonecrotic hips treated with vascularized bone grafting for a mean of 14.4 years (range, 10.5–26 years), the results demonstrated that 75 % of the hips did not require total hip arthroplasty after 10 years. See Table 42.1 for a summary of studies on vascularized bone grafting procedures.
Table 42.1
Vascularized bone grafting
Author (year) | Level of evidence | Stage | Number of hips | Mean age (years) | Mean follow-up (years) | Survivorship |
|---|---|---|---|---|---|---|
Eward et al. (2012) [23] | IV | Ficat stages I and II | 65 | 32.1 | 14.4 | 75 |
Yin et al. (2011) [24] | IV | Steinberg stages II to IV | 14 | 34 | 3.3 | 100 |
Chen et al. (2009) [19] | IV | ARCO stages IIIA and IIIB | 33 | 37 | 6.2 | 24 |
Sun et al. (2009) [25] | IV | Steinberg stages II to V | 80 | 31 | 4.3 | 100 |
Babhulkar et al. (2009) [26] | IV | ARCO stages IIB and IIIC | 31 | 32 | 8 | 96.7 |
Bakshi et al. (2009) [27] | IV | Ficat stages I to III | 187 | 35.5 | 16.5 | 71 |
Kawate et al. (2007) [28] | IV
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|